No products in the cart.
Voriconazole Canon, 50 mg 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmgroup: Antifungal agent.
Pharmacological action: Antifungal agent, triazole derivative. The mechanism of action is associated with inhibition of 14α-sterol demethylation mediated by fungal cytochrome P450, this reaction is a key step in ergosterol biosynthesis.
In vitro voriconazole has a broad spectrum of antifungal action, is active against Candida spp. (including fluconazole-resistant strains of Candida krusei and resistant strains of Candida glabrata and Candida albicans) and has a fungicidal effect against all studied strains of Aspergillus spp, as well as pathogenic fungi that have become relevant recently, including Scedosporium or Fusarium, which are sensitive to antifungal agents to a limited extent.
The clinical efficacy of voriconazole has been demonstrated in infections caused by Aspergillus spp. (including Aspergillus flavus, Aspergillus fumigatus, Aspergillus terreus, Aspergillus niger, Aspergillus nidulans), Candida spp. (including Candida albicans, Candida dubliniensis, Candida glabrata, Candida inconspicua, Candida krusei, Candida parapsilosis, Candida tropicalis and Candida guillermondii strains), Scedosporium spp. (including Scedosporium apiospermum /Pseudoallescheria boydii/, Scedosporium prolifecans) and Fusarium spp.
Other fungal infections in which partial or complete antifungal effects were observed included isolated infections caused by Alternaria spp, Blastomyces dermatitidis, Blastoschizomyces capitatus, Cladosporium spp, Coccidoides immitis, Conidiobolus coronatus, Cryptococcus neoformans, Exserohilum rostratum, Exophiala spinifera, Fonsecaea pedrosoi, Madurella mycetomatis, Paecilomyces lilacinus, Penicillium spp. (including Penicillium marneffei), Philaphora richardsiae, Scopulariopsis brevicaulis and Trychosporon spp. (including Trychosporon beigelii).
In vitro activity of voriconazole against clinical strains of Acremonium spp, Alternaria spp., Bipolaris spp., Cladophialophora spp., Histoplasma capsulatum. The growth of most strains was suppressed at voriconazole concentrations from 0.05 to 2 µg/ml.
In vitro activity of voriconazole against Curvularia spp. and Sporothrix spp. was detected, but its clinical significance is unknown.
Indications
Indications
Invasive aspergillosis; severe invasive candidiasis infections (including Candida krusei); esophageal candidiasis; severe fungal infections caused by Scedosporium spp. and Fusarium spp.; severe fungal infections with intolerance or refractoriness to other drugs; prevention of breakthrough fungal infections in febrile patients from high risk groups (allogeneic bone marrow recipients, patients with relapsed leukemia).
Active ingredient
Active ingredient
Composition
Composition
Active ingredient: voriconazole 50 mg.
How to take, the dosage
How to take, the dosage
It is administered orally or parenterally as an infusion.
The dose is set individually, depending on the indication, age and body weight of the patient, the treatment regimen.
Interaction
Interaction
Voriconazole is metabolized with participation of CYP2C19, CYP2C9 and CYP3A4 isoenzymes. Inhibitors or inducers of these isoenzymes may cause, respectively, an increase or decrease in plasma concentrations of voriconazole.
Concomitant use with rifampicin (CYP isoenzyme inducer) at a dose of 600 mg/day decreases Cmax and AUC of voriconazole by 93% and 96% respectively (the combination is contraindicated).
When concomitantly used with voriconazole, ritonavir (a CYP isoenzyme inducer, inhibitor and substrate of CYP3A4) at a dose of 400 mg every 12 h reduced the Cmax at equilibrium and AUC of oral voriconazole by an average of 66% and 82% respectively. The effect of lower doses of ritonavir on voriconazole concentrations is not yet known. It was found that repeated oral use of voriconazole had no significant effect on the Cmax at equilibrium and AUC of ritonavir also taken repeatedly (concomitant use of voriconazole and ritonavir at a dose of 400 mg every 12 hours is contraindicated).
Co-administration with potent inducers of CYP isoenzymes carbamazepine or long-acting barbiturates (phenobarbital) may significantly decrease plasma Cmax of voriconazole, although their interaction has not been studied. This combination is contraindicated.
Co-administration with cimetidine (nonspecific inhibitor of CYP isoenzymes) at a dose of 400 mg 2 times per day increases Cmax and AUC of voriconazole by 18% and 23% respectively (dose adjustment of voriconazole is not required).
Voriconazole inhibits activity of CYP2C19, CYP2C9, CYP3A4, that is why concentration increase in plasma of medicines metabolized by these isoenzymes is possible.
Concomitant use of voriconazole with terfenadine, astemizole, cisapride, pimozide and quinidine may significantly increase their plasma concentrations, which may lead to prolonged QT interval and in rare cases to the development of ventricular fibrillation/tripping (the combination is contraindicated).
Co-administration of voriconazole increases Cmax and AUC of sirolimus (2 mg once) by 556% and 1014% respectively (combination contraindicated).
Co-administration of voriconazole may increase concentrations of ergot alkaloids (ergotamine and dihydroergotamine) in plasma and ergotism (this combination is contraindicated).
When co-administered in patients who have undergone renal transplantation and are stable, voriconazole increases Cmax and AUC of cyclosporine by at least 13% and 70%, respectively, which is accompanied by an increased risk of nephrotoxic reactions. When using voriconazole in patients receiving cyclosporine, it is recommended to reduce the dose of cyclosporine by half and monitor its plasma levels. After voriconazole cancellation it is necessary to control cyclosporine levels and increase the dose if necessary.
Co-administration of voriconazole increases Cmax and AUC of tacrolimus (used in 0.1 mg/kg single dose) by 117% and 221% respectively, which may be accompanied by nephrotoxic reactions. When using voriconazole in patients receiving tacrolimus, it is recommended to reduce the dose of the latter to 1/3 and monitor its plasma levels. After voriconazole withdrawal the concentration of tacrolimus should be controlled and the dose should be increased if necessary.
Concomitant administration of voriconazole (300 mg 2 times per day) and warfarin (30 mg 1 time per day) was accompanied by the increase of maximal prothrombin time up to 93%. It is recommended to monitor prothrombin time in concomitant administration of warfarin and voriconazole.
Combined use of voriconazole may increase plasma concentration of phenprocoumon, acenocoumarol (CYP2C9, CYP3A4 substrates) and prothrombin time. When using voriconazole in patients receiving coumarin preparations the prothrombin time should be controlled at short intervals, and the doses of anticoagulants should be adjusted accordingly.
In co-administration voriconazole may increase plasma concentration of sulfonylurea derivatives (CYP2C9 substrates) – tolbutamide, glipizide and glibenclamide and cause hypoglycemia. In concomitant use it is necessary to carefully monitor blood glucose levels.
In vitro voriconazole inhibits metabolism of lovastatin (CYP3A4 substrate). Co-administration may increase plasma concentrations of statins metabolized by CYP3A4, which may increase the risk of rhabdomyolysis. In concomitant use it is recommended to assess the feasibility of statin dose adjustment.
In vitro voriconazole inhibits metabolism of midazolam (CYP3A4 substrate). Co-administration may increase plasma concentrations of benzodiazepines (midazolam, triazolam, alprazolam) metabolized under the influence of CYP3A4 and develop prolonged sedative effect. It is recommended to discuss the expediency of benzodiazepine dose adjustment if these drugs are used concomitantly.
In concomitant use voriconazole may increase plasma levels of barberry alkaloids (CYP3A4 substrates) – vincristine, vinblastine and lead to the development of neurotoxic reactions. It is recommended to discuss the expediency of dose adjustment of periwinkle alkaloids.
Voriconazole increases Cmax and AUC of prednisolone (CYP3A4 substrate) used at a dose of 60 mg once by 11% and 34% respectively. It is not recommended to correct the dose.
In concurrent usage with voriconazole, efavirenz (CYP3A4 substrate, according to some studies it is CYP3A4 inhibitor or inducer depending on the dose) used in dose 400 mg once daily in equilibrium reduces Cmax and AUC of voriconazole in average by 61% and 77% respectively. Voriconazole in equilibrium (400 mg orally every 12 hours on the first day, then 200 mg orally every 12 hours for 8 days) increases equilibrium Cmax and AUC of efavirenz on average by 38% and 44% respectively (this combination is contraindicated).
Co-administration of phenytoin (CYP2C9 substrate and potent inducer of cytochrome P450 isoenzymes), administered in dose 300 mg once per day, decreases Cmax and AUC of voriconazole by 49% and 69% respectively; and voriconazole (400 mg 2 times/day) increases Cmax and AUC of phenytoin by 67% and 81%, respectively (if co-administration is necessary, the ratio of estimated benefit to potential risk of combined therapy should be carefully evaluated, and plasma levels of phenytoin should be carefully monitored).
When co-administered rifabutin (cytochrome P450 inducer) administered at a dose of 300 mg once daily reduces Cmax and AUC of voriconazole (200 mg once daily) by 69% and 78% respectively. When co-administration with rifabutin Cmax and AUC of voriconazole (350 mg 2 times/day) were 96% and 68% respectively from those of voriconazole monotherapy (200 mg 2 times/day). Cmax and AUC of voriconazole at a dose of 400 mg 2 times per day were 104% and 87% higher respectively than those of voriconazole monotherapy at a dose of 200 mg 2 times per day. Voriconazole at a dose of 400 mg 2 times/day increases Cmax and AUC of rifabutin by 195% and 331%, respectively. In concomitant treatment with rifabutin and voriconazole it is recommended to conduct regular detailed analysis of peripheral blood picture and control undesirable effects of rifabutin (e.g. uveitis).
When used together in dose 40 mg once daily omeprazole (CYP2C19 inhibitor; CYP2C19 and CYP3A4 substrate) increased Cmax and AUC of voriconazole by 15% and 41% respectively, and voriconazole increased Cmax and AUC of omeprazole by 116% and 280% respectively (accordingly, there is no need to adjust voriconazole dose, and omeprazole dose should be reduced by half). The possibility of drug interactions between voriconazole and other H+-K+-ATPase inhibitors that are CYP2C19 substrates should be considered.
When concomitant use with other HIV protease inhibitors (CYP3A4 substrates and inhibitors) the patient should be carefully monitored for possible toxic effects.Because in vitro studies have shown that voriconazole and HIV protease inhibitors (saquinavir, amprenavir, nelfinavir) can mutually inhibit each other’s metabolism.
Special Instructions
Special Instructions
Use with caution in patients with severe hepatic insufficiency, with severe renal failure (when parenteral administration) and with hypersensitivity to other drugs – azole derivatives.
Correction of electrolyte disturbances (hypokalemia, hypomagnesemia and hypocalcemia) is required prior to the start of therapy.
Sampling for culture and other laboratory tests (serological and histopathological) for pathogen isolation and identification should be performed prior to the start of therapy. The therapy may be started before the results of laboratory tests are obtained and then, if necessary, adjusted.
The use of voriconazole may lead to prolongation of QT interval on ECG, which is accompanied by rare cases of ventricular flutter in patients with multiple risk factors (cardiotoxic chemotherapy, cardiomyopathy, hypokalemia and concomitant therapy that may have contributed to cardiovascular adverse events). In patients with these potentially proarrhythmic conditions voriconazole should be used with caution.
During the treatment liver function should be controlled regularly (in case of clinical signs of liver disease the termination of therapy should be discussed), renal function (including serum creatinine level).
In the progression of dermatological reactions the drug should be discontinued.
During treatment patients receiving voriconazole should avoid sun exposure and UV exposure.
If voriconazole is concomitantly used in patients receiving cyclosporine and tacrolimus, the dose of the latter should be adjusted and their plasma concentrations monitored. After withdrawal of voriconazole, plasma concentrations of cyclosporine and tacrolimus should be assessed and, if necessary, their doses should be increased.
If the combined use of voriconazole and phenytoin is necessary, the estimated benefit and potential risk of combined therapy should be carefully evaluated and phenytoin levels should be continuously monitored.
If the combined use of voriconazole and rifabutin is necessary, the estimated benefit and potential risk of combined therapy should be carefully evaluated and the peripheline picture should be controlled. During the use of voriconazole, patients should not drive in the dark.
Contraindications
Contraindications
Concurrent use of CYP3A4 substrate drugs – terfenadine, astemizole, cisapride, pimozide and quinidine; simultaneous use of sirolimus; simultaneous use of rifampicin, carbamazepine and long-acting barbiturates; concomitant use of ritonavir; concomitant use of efavirenz; concomitant use of ergot alkaloids (ergotamine, dihydroergotamine); hypersensitivity to voriconazole.
Side effects
Side effects
The body in general: very often – fever, peripheral edema; often – chills, asthenia, chest pain, reactions and inflammation at the injection site, flu-like syndrome.
Cardiovascular system disorders: common – decreased BP, thrombophlebitis, phlebitis; rare – atrial arrhythmias, bradycardia, tachycardia, ventricular arrhythmias; very rare – supraventricular tachycardia, complete AV blockade, Gis bundle leg block, nodal arrhythmias, ventricular tachycardia (including ventricular flutter), prolonged QT interval, ventricular fibrillation.
Digestive system disorders: very common – nausea, vomiting, diarrhea, abdominal pain; common – increased activity of ALT, AST, ALF, LDH, GGT and plasma bilirubin levels, jaundice, cheilitis, cholestasis; rare – cholecystitis, cholelithiasis, constipation, duodenitis, dyspepsia, liver enlargement, gingivitis, glossitis, hepatitis, liver failure, pancreatitis, tongue edema, peritonitis; very rare – pseudomembranous colitis, liver coma. In patients with serious underlying diseases (malignant hematologic diseases) against the background of using voriconazole rarely observed cases of severe hepatotoxicity (cases of jaundice, hepatitis, hepatocellular failure, leading to death).
Endocrine system: rare – insufficiency of the adrenal cortex, very rare – hyperthyroidism, hypothyroidism.
Allergic reactions: rare – toxic epidermal necrolysis, Stevens-Johnson syndrome, urticaria; very rare – angioedema, erythema multiforme. In intravenous infusion anaphylactoid reactions have been described, including hot flashes, fever, sweating, tachycardia, chest tightness, shortness of breath, fainting states, itching, rash.
Blood system disorders: often – thrombocytopenia, anemia (incl. macrocytic, microcytic, normocytic, megaloblastic, aplastic), leukopenia, pancytopenia; rarely – lymphadenopathy, agranulocytosis, eosinophilia, disseminated intravascular coagulation syndrome, suppression of medullar hemopoiesis; very rarely – lymphangitis.
Metabolism: frequently – hypokalemia, hypoglycemia, rarely – hypocholesterolemia.
Musculoskeletal system: frequently – back pain, rarely – arthritis.
CNS and peripheral nervous system disorders: very common Рheadache; common Рdizziness, hallucinations, confusion, depression, anxiety, tremor, agitation, paresthesias; rare Рataxia, cerebral edema, intracranial hypertension, hyposthesia, nystagmus, dizziness, syncope; very rare РGuillain-Barr̩ syndrome, oculomotor crisis, ectrapyramid syndrome.
Respiratory system: common – respiratory distress syndrome, pulmonary edema, sinusitis.
Dermatological reactions: very common – rash, common – itching, maculopapular rash, photosensitization, alopecia, exfoliative dermatitis, facial edema, purpura, rarely – psoriasis, very rare – lupus erythematosus.
Senses: frequently – visual disturbances (including visual disturbance/enhancement, fogging of the eyes, altered color perception, photophobia), rarely – blepharitis, optic neuritis, papilledema, scleritis, impaired sense of taste, diplopia, very rarely – retinal hemorrhage, corneal clouding, optic atrophy.
Urinary system: often – increased serum creatinine level, acute renal failure, hematuria; rarely – increased residual urea nitrogen, albuminuria, nephritis; very rarely – renal tubule necrosis.
Similarities
Similarities
Additional information
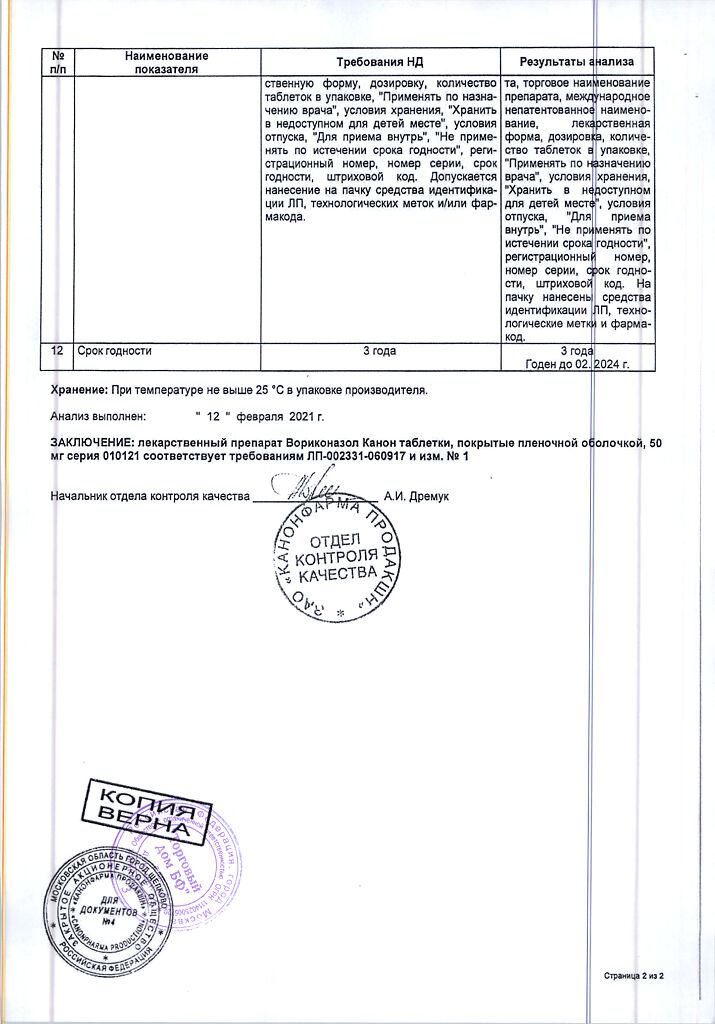
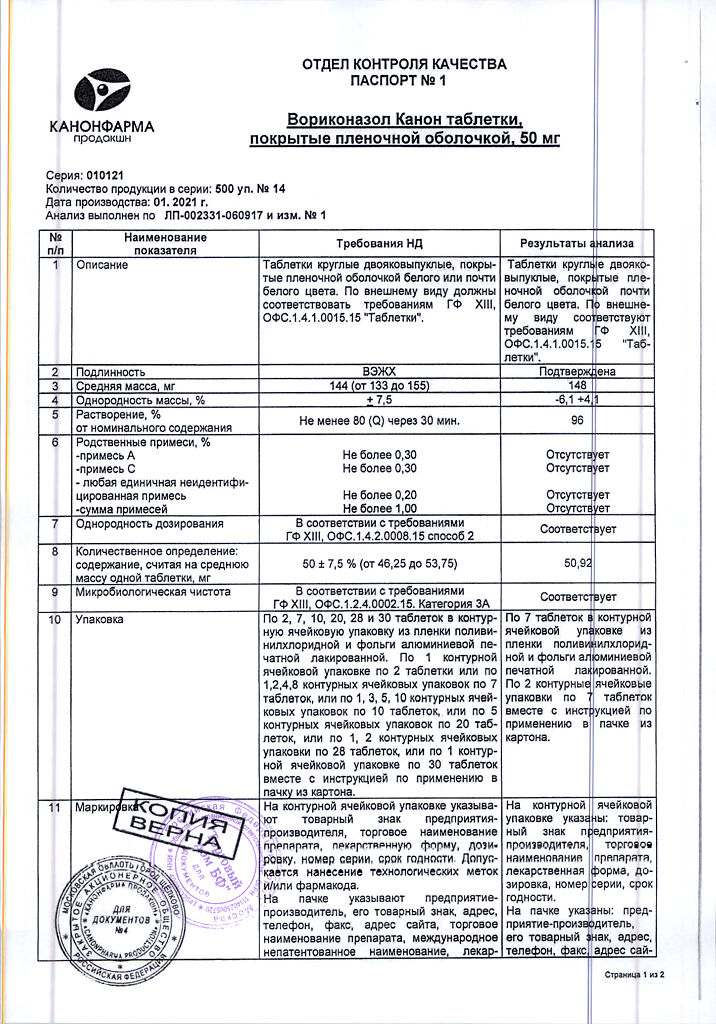
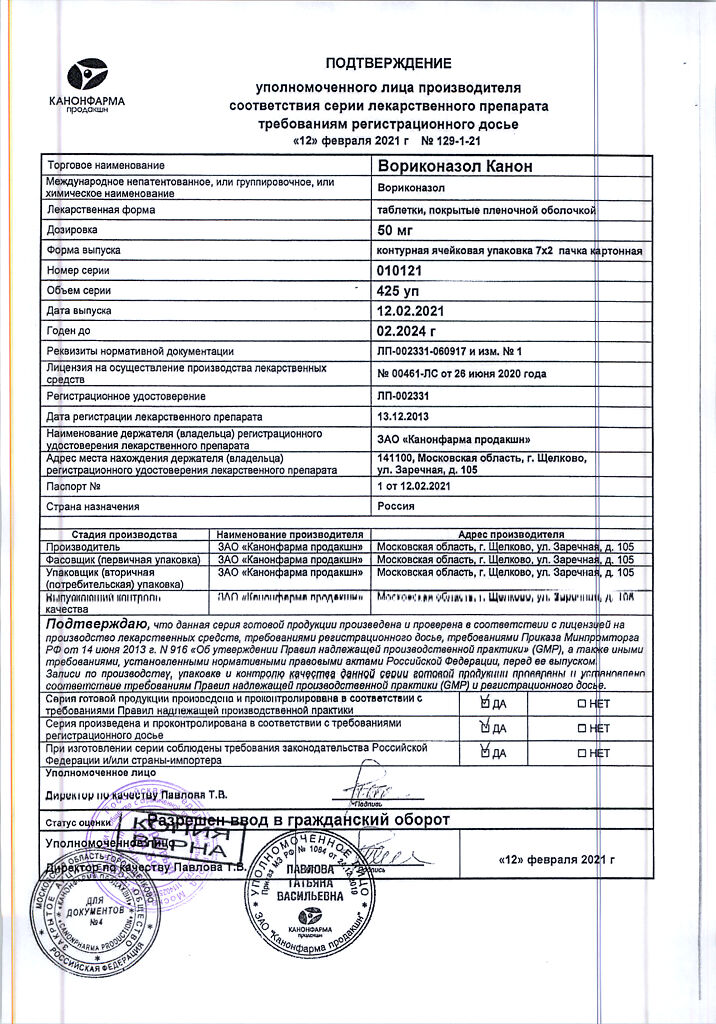
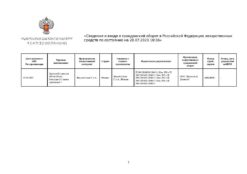
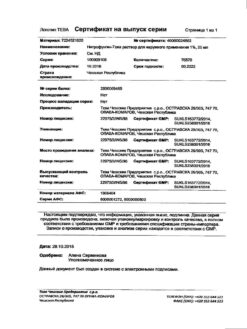
| Manufacturer | Kanonfarma Production ZAO, Russia |
|---|---|
| Medication form | pills |
| Brand | Kanonfarma Production ZAO |
Related products
Buy Voriconazole Canon, 50 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.