No products in the cart.
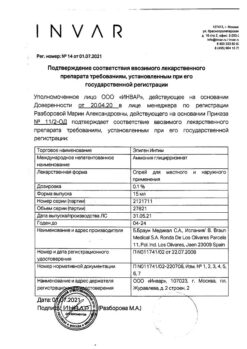
Vidora Micro, 3 mg+0.02 mg 24+4 pcs.
€21.39 €17.82
EAN: 8437009433836
SKU: 281029
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Contraception
Contraception.
Contraception and treatment of moderate acne (acne vulgaris).
Contraception and treatment of severe premenstrual syndrome (PMS).
Indications
Indications
Contraception.
Contraception and treatment of moderate acne (acne vulgaris).
Contraception and treatment of severe premenstrual syndrome (PMS).
Pharmacological effect
Pharmacological effect
Combined contraceptive (estrogen + gestagen)
Special instructions
Special instructions
Before starting to use the drug, pregnancy should be excluded and it is recommended to undergo a thorough general medical and gynecological examination, including examination of the mammary glands and cytological examination of the cervix. In addition, a violation of the blood coagulation system should be excluded. In case of long-term use, preventive control examinations must be carried out at least once every 6 months.
The woman should be warned that the drug does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
A number of epidemiological studies have revealed an increased incidence of venous and arterial thrombosis and thromboembolism when taking COCs. The greatest risk of developing these complications exists in the first year of taking the drug (especially in the first 3 months) or resuming use after a 4-week break. The use of any COC may be complicated by the development of venous thromboembolism (VTE), manifested as deep vein thrombosis and pulmonary embolism. The estimated incidence of VTE in women taking low-dose estrogen oral contraceptives (less than 50 mcg ethinyl estradiol) is up to 4 per 10,000 women per year, compared with 0.5 to 3 per 10,000 women not using oral contraceptives.
Medicines containing levonorgestrel, norgestimate, or norethindrone have a low risk of developing venous thromboembolism. In drugs that include drospirenone, the risk of developing thromboembolic complications is 2 times higher, therefore, before a woman is recommended to use Vidora® micro, she should be warned about this increased risk.
Per 10,000 women taking COCs with drospirenone, VTE develops in approximately 9-12 within 1 year, and in women taking COCs with levonorgestrel – only 5-7.
However, the incidence of VTE occurring while taking COCs is less than that associated with pregnancy.
In women taking COCs, extremely rare cases of thrombosis of other blood vessels, for example, the hepatic, mesenteric, renal arteries and veins, the central retinal vein and its branches, have been described. The connection with taking COCs has not been proven.
A woman should stop taking the drug and consult a doctor if symptoms of venous or arterial thrombosis develop, which may include unilateral pain in the lower extremities and/or swelling; sudden severe chest pain; with or without irradiation to the left hand; sudden shortness of breath; sudden cough; any unusual, severe, prolonged headache; increased frequency and severity of migraines; sudden partial or complete loss of vision; diplopia; slurred speech or aphasia; dizziness; loss of consciousness or fainting with or without an epileptic seizure; weakness or very significant loss of sensation that suddenly appears on one side or in one part of the body; movement disorders; “sharp” stomach.
The risk of thrombosis (venous and/or arterial) and thromboembolism increases: with age; in smokers (with increasing number of cigarettes smoked or increasing age. The risk further increases, especially in women over 35 years of age); in the presence of a family history (i.e., venous or arterial thromboembolism ever in close relatives or parents at a relatively young age), obesity (body mass index more than 30 kg/m2), dyslipoproteinemia; arterial hypertension; heart valve diseases; atrial fibrillation; prolonged immobilization; temporary immobilization, including flights for more than 4 hours; serious surgery, any operation on the lower extremities or major trauma – in these situations it is necessary to stop taking the drug; in case of planned surgery – 4 weeks before it and do not resume taking it for 2 weeks after the end of immobilization.
The increased risk of thromboembolism in the postpartum period should be taken into account.
Peripheral circulatory disorders may also occur in diabetes mellitus, SLE, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn’s disease or ulcerative colitis) and sickle cell anemia.
An increase in the frequency and severity of migraine during the use of COCs (which may precede cerebrovascular events) may be grounds for immediate discontinuation of these medications.
Biochemical parameters that may be a sign of hereditary or acquired predisposition to venous or arterial thrombosis include: APS resistance, hyperhomocysteinemia, antithrombin III deficiency, protein C and S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
When considering the risk/benefit ratio, the physician should consider that adequate treatment of these conditions may reduce the associated risk of thrombosis and that the risk of thrombosis associated with pregnancy is greater than with COCs.
An increased risk of cervical cancer with long-term use of COCs has been reported in some epidemiological studies. Its connection with COC use has not been proven.
A meta-analysis of 54 epidemiological studies demonstrated that there is a slightly increased relative risk (RR=1.24) of developing breast cancer diagnosed in women who were using COCs at the time of the study. Its connection with COC use has not been proven. The observed increased risk may be due to earlier diagnosis of breast cancer (women who use COCs have earlier stages of breast cancer than women who have never used them), biological effects of COCs, or a combination of both.
In rare cases, the development of liver tumors has been observed during the use of COCs. If severe abdominal pain, liver enlargement, or signs of intra-abdominal bleeding occur, this should be taken into account when making a differential diagnosis.
Drospirenone is well tolerated when used in patients with mild to moderate hepatic impairment (Child-Pugh class B).
Recurrent cholestatic jaundice, which develops for the first time during pregnancy or during previous use of sex hormones, requires discontinuation of COCs.
Drospirenone is well tolerated when used in women with mild to moderate renal failure.
K+ excretion may be reduced in patients with renal failure. In a clinical study, drospirenone had no effect on plasma concentrations in patients with mild to moderate renal failure. Since theoretically the risk of developing hyperkalemia exists in cases where the concentration of K+ in the blood plasma before treatment was at the upper limit of the normal range and while taking potassium-sparing drugs, it is recommended to monitor the concentration of K+ in the blood plasma in the first cycle of taking the drug in patients with mild to moderate renal failure and with the concentration of K+ in the blood plasma at the upper limit of the normal range before taking it and, especially, with the concomitant use of potassium-sparing drugs.
Women with hypertriglyceridemia or a family history of hypertriglyceridemia are at increased risk of developing pancreatitis while taking COCs.
Although slight increases in blood pressure (BP) have been described in many women taking COCs, clinically significant increases have been reported rarely. The relationship between taking COCs and a clinically significant increase in blood pressure has not been established. However, if a persistent, clinically significant increase in blood pressure develops while taking a COC, discontinuation of the drug and treatment of arterial hypertension is necessary. Taking COCs can be continued after consulting a doctor if normal blood pressure values are achieved with antihypertensive therapy.
Although COCs may have an effect on insulin resistance and glucose tolerance, there is no need to change the therapeutic regimen in diabetic patients using COCs. However, women with diabetes mellitus should be carefully monitored while taking COCs.
Women with a tendency to chloasma should avoid prolonged exposure to the sun and exposure to ultraviolet radiation while taking COCs.
The drug can affect biochemical indicators of the function of the liver, thyroid gland, adrenal glands and kidneys, as well as the amount of plasma transport proteins, such as DSG and lipid/lipoprotein fractions, indicators of carbohydrate metabolism, blood clotting and fibrinolysis. Changes usually do not go beyond normal values.
Due to its antimineralocorticoid activity, drospirenone increases the concentration of renin and aldosterone in the blood plasma.
While taking COCs, the course of endogenous depression and epilepsy may worsen.
The use of Vidora® micro as a COC may be especially useful for women with hormone-dependent fluid retention, as well as women with acne and seborrhea. The effectiveness of COCs may be reduced by missed pills, vomiting and diarrhea, or as a result of drug interactions.
While taking COCs, irregular bleeding may occur (“spotting” or “breakthrough” bleeding), especially during the first months of use. Therefore, assessing any irregular bleeding is only meaningful after 3-4 months of contraception.
If irregular bleeding recurs or develops after previous regular cycles, careful evaluation should be performed to rule out malignancy or pregnancy.
Some women may not develop withdrawal bleeding while off the pill. If you take COCs as directed, pregnancy is unlikely. However, if you have not been taking COCs regularly before, or if there are no two withdrawal bleedings in a row, then pregnancy must be ruled out before continuing to take the drug.
Impact on the ability to drive vehicles. Wed and fur.:
There was no effect on the ability to drive vehicles and machinery.
Active ingredient
Active ingredient
Drospirenone, Ethinylestradiol
Composition
Composition
drospirenone – 3.00 mg,
Contraindications
Contraindications
– Hypersensitivity to any of the components of the drug;
– thrombosis (venous and arterial) currently or in history (including deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular disorders);
– conditions preceding thrombosis (including transient ischemic attacks, atrial fibrillation, angina) currently or in history;
– the presence of multiple or pronounced risk factors for venous or arterial thrombosis, including: complicated lesions of the heart valve apparatus, atrial fibrillation, diseases of the cerebral vessels or coronary arteries;
– uncontrolled arterial hypertension, prolonged immobilization, extensive surgery, surgery on the lower extremities, extensive trauma, smoking over the age of 35 years, obesity with a body mass index of more than 30 kg/m2;
– hereditary or acquired predisposition to venous or arterial thrombosis, such as resistance to activated protein C (APC), antithrombin III deficiency, protein C deficiency, protein S deficiency, hyperhomocysteinemia and the presence of antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant);
– migraine with focal neurological symptoms currently or in history;
– diabetes mellitus with diabetic angiopathy;
– liver failure and severe liver diseases (before normalization of liver function test values and within three months after these indicators return to normal);
– liver tumors (benign or malignant) currently or in history;
– severe or acute renal failure;
– identified or suspected hormone-dependent malignant diseases (including genital organs or mammary glands);
– bleeding from the vagina of unknown origin;
– pregnancy or suspicion of it;
– breastfeeding period;
– pancreatitis with severe hypertriglyceridemia currently or in history;
– hereditary lactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
If any of the above diseases or conditions develop for the first time while taking the drug, it should be discontinued immediately.
With caution:
– Risk factors for the development of thrombosis and thromboembolism: smoking, obesity with a body mass index less than 30 kg/m2, dyslipoproteinemia, controlled arterial hypertension, migraine without focal neurological symptoms, uncomplicated valvular heart disease, the presence of thrombosis and thromboembolism in a family history (thrombosis, myocardial infarction or cerebrovascular accident at a young age any of the immediate relatives); age over 35 years in non-smoking women;
– diseases in which peripheral circulatory disorders may occur: diabetes mellitus without vascular disorders, systemic lupus erythematosus (SLE), hemolytic-uremic syndrome, Crohn’s disease, ulcerative colitis, sickle cell anemia, phlebitis of the superficial veins;
– hereditary angioedema;
– hypertriglyceridemia;
– mild to moderate liver disease;
– diseases that first appeared or worsened during pregnancy or against the background of previous use of sex hormones (including jaundice and/or itching associated with cholestasis, cholelithiasis, otosclerosis with hearing impairment, porphyria, a history of herpes during pregnancy, Sydenham’s chorea, chloasma, the postpartum period).
Side Effects
Side Effects
The following adverse reactions have been reported in women using COCs, with a very rare incidence or delayed symptoms, which are thought to be related to COC use:
– breast cancer (see section “Special instructions”);
– liver tumors (benign and malignant);
– pancreatitis in women with hypertriglyceridemia;
– the appearance or worsening of conditions whose connection with the use of COCs has not been definitively established: porphyria, epilepsy, uterine fibroids, SLE, herpes during pregnancy, Sydenham’s chorea, hemolytic-uremic syndrome, cholestatic jaundice and/or itching associated with cholestasis; cholelithiasis;
– liver dysfunction;
– changes in glucose tolerance and development of insulin resistance;
– chloasma;
– Crohn’s disease, ulcerative colitis.
In women with hereditary angioedema, estrogen may cause or worsen symptoms.
Interaction
Interaction
Long-term treatment with drugs that induce microsomal liver enzymes, which increases the clearance of sex hormones, can lead to a decrease in contraceptive effectiveness. These drugs include: phenytoin, barbiturates, primidone, carbamazepine, oxcarbazepine, rifampicin, rifabutin, topiramate, felbamate, griseofulvin and drugs containing St. John’s wort.
HIV protease inhibitors (ritonavir), non-nucleoside reverse transcriptase inhibitors (nevirapine) and combinations thereof may also potentially affect hepatic metabolism. Maximum enzyme induction is usually achieved approximately 10 days after starting these medications, but may persist for at least 4 weeks after discontinuation. When taking drugs that affect the induction of microsomal liver enzymes simultaneously and within 28 days after their discontinuation, it is necessary to temporarily use a barrier method of contraception. If it is necessary to continue taking drugs that induce microsomal liver enzymes after taking the last active tablet from the current package of Vidora® micro, you should skip taking placebo tablets and start taking tablets from a new package.
Contraceptive protection is reduced when taking antibiotics of the penicillin and tetracycline series due to their reduction in the intrahepatic circulation of estrogens and, as a consequence, a decrease in the concentration of ethinyl estradiol. While taking these antibiotics and for 7 days after their discontinuation, it is necessary to additionally use a barrier method of contraception.
Since the main metabolites of drospirenone in human plasma are formed without the participation of the cytochrome P450 system, inhibitors of this enzyme system do not affect the metabolism of drospirenone.
Oral combined estrogen-progestin contraceptives may affect the metabolism of other drugs, leading to an increase (cyclosporine) or decrease (lamotrigine) in their plasma and tissue concentrations. Despite the fact that taking COCs affects peripheral insulin resistance and glucose tolerance, adjustment of the dosage regimen of hypoglycemic drugs while taking COCs is not required.
Based on in vitro inhibition studies and in vivo drug interaction studies involving female volunteers, it was found that drospirenone at a dose of 3 mg does not affect the metabolism of omeprazole, simvastatin and midazolam.
There is a theoretical possibility of increasing the concentration of potassium (K+) in the blood plasma in women receiving oral contraceptives simultaneously with drugs that increase the concentration of K+ in the blood plasma: angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, some non-steroidal anti-inflammatory drugs (for example, indomethacin), potassium-sparing diuretics and aldosterone antagonists. However, in a study evaluating the interaction of an ACE inhibitor with the combination of drospirenone + estradiol in women with moderate arterial hypertension receiving enalapril and placebo, there was no significant difference between serum K + concentrations.
Overdose
Overdose
Symptoms may include: nausea, vomiting, spotting, vaginal discharge or metrorrhagia.
Treatment: there is no specific antidote; symptomatic therapy is carried out.
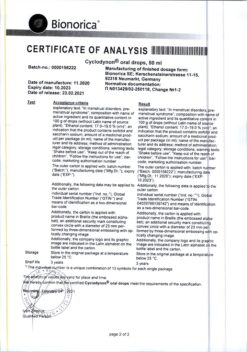
Manufacturer
Manufacturer
Laboratorios Leon Pharma S.A., Spain
Additional information
| Manufacturer | Laboratorios Leon Pharma S.A., Spain |
|---|---|
| Medication form | pills |
| Brand | Laboratorios Leon Pharma S.A. |
Other forms…
Related products
Gynecology and Obstetrics
Buy Vidora Micro, 3 mg+0.02 mg 24+4 pcs. with delivery to USA, UK, Europe and over 120 other countries.