No products in the cart.
Vancomycin, lyophilizate and oral administration 1 g
€7.71 €6.99
Description
Pharmacotherapeutic group
Antibiotic glycopeptide
ATX code: J01XA01
Pharmacodynamics:
Vancomycin is a tricyclic glycopeptide antibiotic produced by Amycolatopsisorientalis. The bactericidal effect of vancomycin is manifested in the inhibition of bacterial cell wall biosynthesis is able to change the permeability of the bacterial cell membrane and the synthesis of ribonucleic acid (RNA). It blocks the synthesis of the bacterial cell wall at a site different from that where penicillins and cephalosporins act (without competing with them for binding sites) by firmly binding to O-alanyl-O-alanine residues of peptidoglycan subunits (located on the outer surface of the cytoplasmic membrane), the main component of the cell wall, leading to cell lysis.
It has bactericidal action against many Gram-positive bacteria and bacteriostatic action against Enterococcus spp. Bactericidal effect on Enterococcus spp. is achieved by the combined administration of vancomycin and aminoglycosides. There is no cross-resistance between vancomycin and antibiotics of other classes.
Active against Gram-positive microorganisms: StaphylococcusaureusStaphylococcusushaemolyticusStaphylococcusepidermidis (including heterogeneous methicillin-resistant strains) Streptococcus spp. (Streptococcuspyogenes Streptococcuspneumoniae Streptococcusagalactiae and others including penicillin-resistant strains) Enterococcus spp. (including Enterococcus faecalis) Clostridium spp. Propionibacterium acnes Actinomyces spp. some strains of Lactobacillus spp. Rhodococcus spp. Corynebacterium spp. Listeria monocytogenes Bacillus spp.
Invitro some isolated strains of Enterococcus spp. and Staphylococcus spp. can show resistance to vancomycin.
In combination with aminoglycosides, in-vitro synergism is observed against many strains of Staphylococcus aureus group D non Enterococcus spp. Streptococcus viridans group. In combination with gentamicin tobramycin rifampicin imipenem, synergistic action against Staphylococcus aureus is observed. In some cases when combining vancomycin and rifampicin antagonism is observed against strains of Staphylococcus spp. this combination of drugs also shows synergistic action against some strains of Streptococcus spp.
Vancomycin is inactive against Gram-negative mycobacteria and fungi.
The optimum of action is at pH 8 with a decrease in pH to 6, the effect is drastically reduced.
The development of Staphylococcus aureus resistance during therapy is very rare. The value of the minimum suppressive concentration (MSC) for most antibiotic-sensitive microorganisms is less than 5 µg/ml the MSC value for vancomycin-resistant strains of Staphylococcusaureus reaches 10-20 mg/l.
In oral administration, it has minimal systemic action locally on sensitive microflora in the gastrointestinal tract (GIT) (StaphylococcusaureusClostridiumdifficile).
Pharmacokinetics:
Intake. After oral administration it is absorbed in minimal amounts. Absorption of the drug is slightly higher in intestinal mucosa inflammation in such patients after administration of 05 g of the drug every 6 hours the maximum concentration in plasma (Cmax) is 24-30 mg/l.
After intravenous administration of 05 g of vancomycin, the Cmax is observed at the end of the infusion and is about 33 mg/L; 1 h and 4 h after administration, it decreases to 73 mg/L and 57 mg/L, respectively.
After intravenous administration of 1 g of vancomycin, its plasma concentration doubles. The cmax is observed immediately after infusion and ranges from 20 to 50 µg/ml; 12 h after infusion, plasma concentrations of vancomycin range from 5 to 10 µg/ml. Plasma concentrations with multiple infusions are similar to those with single infusions.
Distribution. Distribution volume 02-125 l/kg in children is slightly less than in adults and is 053-082 l/kg. Binding with plasma proteins is 30-55%. After intravenous administration vancomycin is detected in tissues (kidneys liver lungs heart vascular wall abscess tissue atrial auricle) and body fluids (pleural pericardial ascitic peritoneal synovial) and also in urine in concentrations inhibiting the growth of sensitive microorganisms. Slowly penetrates into the cerebrospinal fluid the rate of penetration through the blood-brain barrier increases with inflammation of the meninges. It penetrates through the placental barrier and is excreted with breast milk.
Metabolism. It is practically not metabolized.
Elimation. Elimination half-life (T1/2) in case of normal renal function: adults 4-6 hours (3-9 hours) premature infants – 98 hours newborns – 67 hours in children aged 3 years – 24 hours in children aged 7 years – 22 hours.
80-90 % of the drug is excreted by the kidneys through glomerular filtration during the first 24 hours in unchanged form. Small amounts (less than 5%) can be excreted with bile. It is excreted in small amounts by hemodialysis or peritoneal dialysis.
In adults the total clearance of vancomycin 07-31 ml/s in children the clearance of vancomycin is higher and reaches maximum values at the age of 39 years (about 3 ml/s).
Pharmacokinetics in special clinical cases. Impaired renal function slows the excretion of vancomycin so dose adjustment is required in these patients. In patients with a removed or absent kidney the average T1/2 is 75 days. Total systemic and renal clearance of vancomycin may be reduced in elderly patients as a result of natural slowing of glomerular filtration.
Indications
Indications
For intravenous infusion:
Serious or severe infections caused by vancomycin-sensitive microorganisms including Staphylococcus spp. (including penicillin- and methicillin-resistant strains) Streptococcus spp. (including penicillin-resistant strains); in allergic reaction to penicillin; in intolerance or lack of response to treatment with other antibiotics, including penicillins or cephalosporins; in infections caused by microorganisms sensitive to vancomycin but resistant to other antimicrobials:
– endocarditis:
– caused by Streptococcusviridans or Streptococcusbovis (as monotherapy or in combination with aminoglycosides);
– caused by enterococci such as Enterococcusfaecalis (only in combination with aminoglycosides);
– early endocarditis caused by Staphylococcusepidermidis or Corynebacterium spp. after valve replacement (in combination with rifampicin aminoglycosides or with both antibiotics);
– prevention of bacterial endocarditis in patients with hypersensitivity reactions to penicillin antibiotics and heart valve disease (before dental and surgical procedures);
– sepsis;
– central nervous system infections (meningitis);
– lower respiratory tract infections (pneumonia pulmonary abscess);
– bone and joint infections (including
– infections of the skin and soft tissues.
For oral administration:
– pseudomembranous colitis caused by Clostridiumdifficile;
– enterocolitis caused by Staphylococcus aureus.
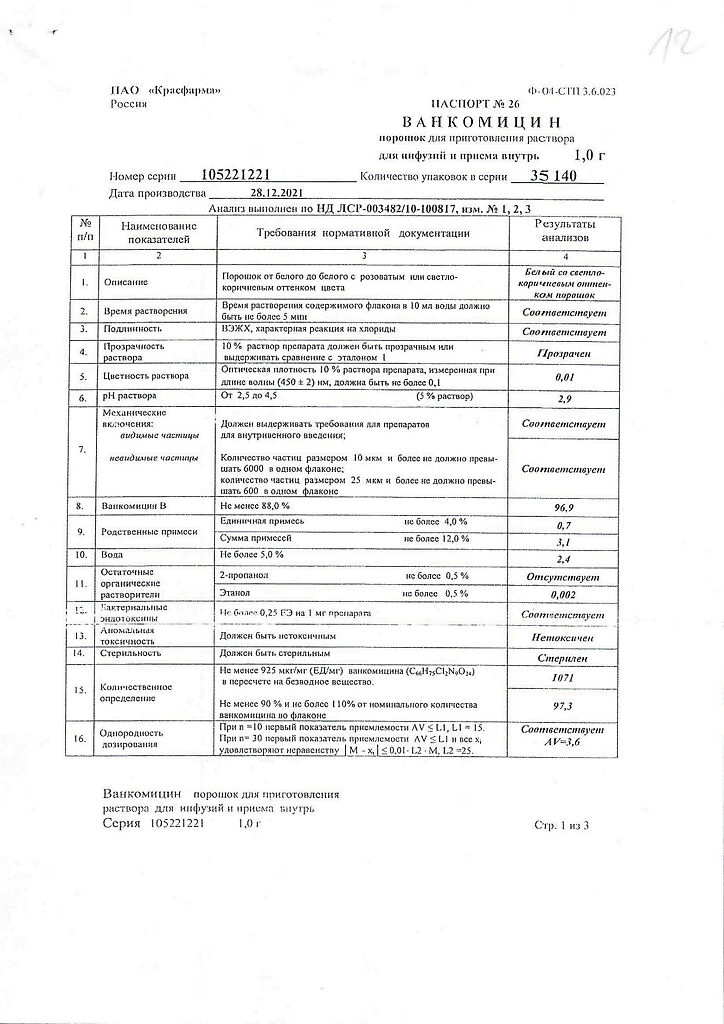
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Dosing regimens for intravenous drip administration
Intravenous (IV) drip. The drug must not be given intramuscularly or intravenously by bolus (stream)!
Adults and children over 12 years of age with normal renal function: 05 g every 6 hours or 1 g every 12 hours. Each dose is recommended to be administered at a rate of no more than 10 mg/min infusion duration of at least 60 min. The daily dose is 2 g. Age, presence of obesity may require modification of the usual dose based on determination of serum vancomycin concentrations.
Children from 1 month to 12 years of age:10 mg/kg every 6 hours. Each dose is administered for at least 60 minutes. The recommended daily dose is 40 mg/kg.
Infants:Initial dose 15 mg/kg followed by a maintenance dose of 10 mg/kg every 12 hours during the first week of life; starting the second week of life, a maintenance dose of 10 mg/kg every 8 hours until age 1 month. Each dose should be administered for at least 60 minutes and continuous monitoring of serum vancomycin concentrations is required.
The concentration of prepared vancomycin solution is not more than 25-5 mg/ml. The maximum daily dose for a child should not exceed the daily dose for an adult – 2 g.
Patients with impaired renal function need individual selection of the dose taking into account serum creatinine levels. Correction can be made by increasing the intervals between doses or by reducing the single dose.
In elderly patients with a lower clearance of vancomycin, the volume of distribution is greater and the dose selection is based on serum vancomycin concentration.
In premature infants and elderly patients as a result of reduced renal function, a significant dose reduction may be required. Plasma vancomycin concentrations should be monitored regularly.
In anuria the starting dose is 15 mg/kg to quickly build up therapeutic serum concentrations of vancomycin for stable drug concentrations the maintenance dose is 19 mg/kg/day.
Correction by increasing the intervals between injections
Patients with severe renal insufficiency should be given maintenance doses of 250-1000 mg once every few days: in CKR 10-50 ml/min – 1 g every 3-7 days in CKR <10 ml/min – 1 g every 7-14 days. In case of anuria, a dose of 1 g every 7-10 days is recommended.
From the known serum creatinine concentration, calculate creatinine clearance using the formula:
For men: body weight kg x (140 – age years) / 72 x serum creatinine concentration mg/100 ml
For women: the result obtained is multiplied by 085.
Patients on hemodialysis:The starting dose is 20-25 mg/kg when using high permeability membranes. Maintenance doses are administered based on the residual plasma concentration of the drug and adjusted to maintain a residual drug concentration of 15-20 mcg/ml.
Vancomycin is effectively eliminated by hemodialysis using high permeability membranes (such as polysulfone) but is poorly eliminated using normal permeability membranes.
Patients with hepatic impairment do not require dose adjustment.
Preparation and administration of solution for infusion
The solution for infusion is prepared in two steps.
The first stage is to dissolve the drug in water for injection: 05 g in 10 ml and 1 g in 20 ml (the concentration of the solution is 50 mg/ml). The solution prepared in this way can be stored at room temperature (not exceeding 25 °C) for 24 h or in a refrigerator (2 to 8 °C) for 96 h.
The second step: vancomycin solutions obtained in the first step must be further diluted to a concentration not exceeding 5 mg/ml before administration, for which they are transferred to a compatible solution for infusion: 05 g in 100 ml and 1 g in 200 ml of 09 % sodium chloride solution of 5 % dextrose solution or Ringer’s solution.
The required dose of vancomycin so diluted should be administered by fractional infusion for at least 60 minutes.
Infusion solutions of the drug on the basis of 09% sodium chloride solution or 5% dextrose solution can be stored in refrigerator (from 2 to 8 °С) for 14 days without significant loss of activity. Solutions prepared with Ringer’s solution can be stored in refrigerator for 4 days (96 hours).
Before administration the prepared solution for infusion should be checked visually for mechanical impurities and color changes.
Intravenous dosing regimens
Vancomycin may be used orally to treat pseudomembranous colitis caused by Clostridium difficile due to antibiotic use and to treat staphylococcal enterocolitis. Intravenous administration of vancomycin has no advantage in the treatment of these diseases.
The drug should be used in the following doses: adults 05-2 g 3-4 times a day children 004 g/kg 3-4 times a day. Total daily dose should not exceed 2 g. The appropriate dose is prepared in 30 ml of water and given to the patient to drink or administered through a tube. To improve the taste of the solution, the usual food syrups can be added to it. The duration of treatment is 7 to 10 days. Vancomycin is not effective when taken orally for other localized infections.
Interaction
Interaction
Erythema and anaphylactoid reactions (including decreased blood pressure, rash, urticaria and pruritus) have been reported with concomitant use of vancomycin and anesthetics. Administration of vancomycin as a 60-minute infusion prior to induction of anesthesia may reduce the likelihood of these reactions. If vancomycin is administered during or immediately after surgery with simultaneous use of muscle relaxants (e.g. suxamethonium iodide), their effects (neuromuscular blockade) may be enhanced and prolonged.
When other potentially ototoxic and/or nephrotoxic drugs (amphoglycosides amphotericin B aminosalicylic acid or other salicylates bacitracin capreomycin carmustine paramomycin cyclosporine “loop” diuretics polymyxine B cisplatin etacrynic acid) are used simultaneously and/or sequentially systemically or topically, close monitoring of the possible development of these symptoms is required.
Colestyramine decreases the effectiveness of vancomycin (when taken orally). Antihistamines meclosine phenothiazines tioxaptenes may mask the symptoms of ototoxic effects of vancomycin (tinnitus vertigo). Pharmaceutical Interaction. Vancomycin solution has a low pH, which may cause physical or chemical instability when mixed with other solutions. Mixing with alkaline solutions should be avoided.
The mixing or simultaneous use of vancomycin solution with chloramphenicol glucocorticoids aminophylline and phenobarbital is not recommended.
Vancomycin and beta-lactam antibiotic solutions are pharmaceutically incompatible when mixed. The likelihood of precipitation increases with increasing vancomycin concentration.
The IV system should be flushed thoroughly between applications of these antibiotics. It is recommended that the concentration of vancomycin solution be reduced to 5 mg/ml or less.
Special Instructions
Special Instructions
The rapid administration (e.g. within a few minutes) may be accompanied by a marked decrease in blood pressure and in rare cases by cardiac arrest. Vancomycin solution for infusion should be administered for at least 60 minutes to avoid adverse reactions associated with the infusion.
With caution, vancomycin should be used in patients with renal impairment (vancomycin doses should be set individually; It is recommended to monitor plasma concentrations of vancomycin in renal failure in patients over 60 years of age) because high sustained blood concentrations of the drug may increase the risk of toxic effects of the drug; the maximum concentration should not exceed 40 mcg/ml minimum concentration is 10 mcg/ml concentrations over 80 mcg/ml are considered toxic.
Vancomycin should be used with caution in patients with an allergy to teicoplanin because cross-allergy has been reported.
Long-term use of vancomycin requires audiogram monitoring of the peripheral blood picture of renal function (total urine analysis creatinine and urea nitrogen values).
Vancomycin is an irritant, so the diffusion of the dissolved drug through the vascular wall may cause necrosis of the adjacent tissues. Thrombophlebitis has been observed, although the likelihood of its development can be reduced by slow administration of dilute solutions (25-5 mg/ml concentration) and by alternating the sites where the drug is administered.
Pediatric use. When administering to newborns (including premature infants) it is recommended to monitor the concentration of vancomycin in blood plasma.
Vancomycin is poorly absorbed after oral administration so it should only be used orally for the treatment of Staphylococcal enterocolitis and pseudomembranous colitis caused by Clostridiumdifficile.
The effect of vancomycin on driving vehicles and engaging in other potentially dangerous activities that require increased concentration and rapid psychomotor reactions has not been studied. However, it should be taken into account that the use of vancomycin may be accompanied by such adverse events as dizziness associated with a drop in blood pressure. Patients experiencing dizziness should refrain from driving vehicles and working with potentially dangerous mechanisms.
Contraindications
Contraindications
Hypersensitivity to vancomycin neuritis of the auditory nerve lactation period.
Hearing impairment (including history) renal failure in patients allergic to teicoplanin (possibility of cross-allergy) pregnancy.
Side effects
Side effects
Blood and lymphatic system disorders: leukopenia reversible neutropenia transient thrombocytopenia agranulocytosis eosinophilia pancytopenia anemia.
Immune system disorders: anaphylactic reactions.
Cardiac disorders:cardiac arrest.
vascular disorders:decreased blood pressure shock vasculitis.
Gastrointestinal disorders:nausea pseudomembranous colitis.
Liver and biliary tract disorders:increased activity of “hepatic” transaminases.
Visual organ disorders:transient long-term (up to 10 hours) lacrimation.
Hearing and labyrinth disorders:Transient or permanent hearing loss decreased hearing vertigo tinnitus.
Respiratory system disorders of the thorax and mediastinum: dyspnea respiratory murmurs.
Dermatological and subcutaneous tissue disorders: rash itchy urticaria exfoliative dermatitis benign (IgA) vesicular dermatosis pruritic dermatosis malignant erythema exudative (Stevens-Johnson syndrome) toxic epidermal necrolysis; drug rash accompanied with eosinophilia and systemic manifestations (DRESS syndrome).
Renal and urinary tract disorders: renal failure manifested by increased serum concentrations of creatinine and urea nitrogen interstitial nephritis acute renal failure.
General disorders and disorders at the injection site:Phlebitis hyperemia of the upper half of the trunk and face spasm of the muscles of the chest and back chills drug fever pain at the injection site tissue necrosis at the injection site. During or shortly after too rapid infusion of vancomycin patients may develop anaphylactoid reactions (decreased blood pressure up to shock and cardiac arrest respiratory murmurs dyspnea skin rash itching). Rapid administration of the drug may also cause “red man” syndrome (chills, fever, palpitations, hyperemia of the upper half of the torso and face, spasm of the muscles of the chest and back).
After stopping the infusion, the reactions usually go away within 20 minutes but can sometimes last up to several hours. A number of patients who have received vancomycin have experienced ototoxicity symptoms. These may be transient or persistent. Most of these cases were observed in patients receiving high doses of vancomycin with a history of hearing loss and renal failure or in patients receiving concomitant treatment with other drugs with possible ototoxicity development such as aminoglycosides.
Overdose
Overdose
Symptoms: increased severity of dose-dependent side effects on the urinary system and sensory organs.
Treatment: There is no specific antidote. It is recommended to cancel the drug or reduce the dose. Symptomatic therapy to maintain glomerular filtration is carried out. Fluid administration and monitoring of plasma concentrations of vancomycin are recommended.
Vancomycin is poorly tolerated by dialysis. Hemofiltration and hemoperfusion via polysulfone ion exchange resin have been reported to increase vancomycin clearance.
Pregnancy use
Pregnancy use
Additional information
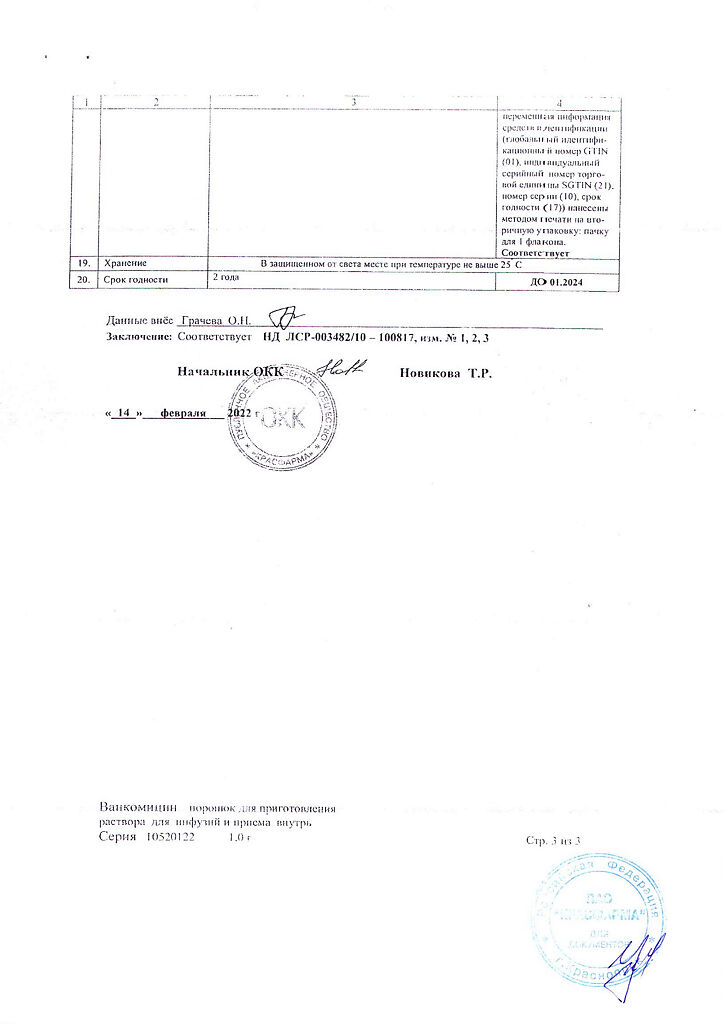
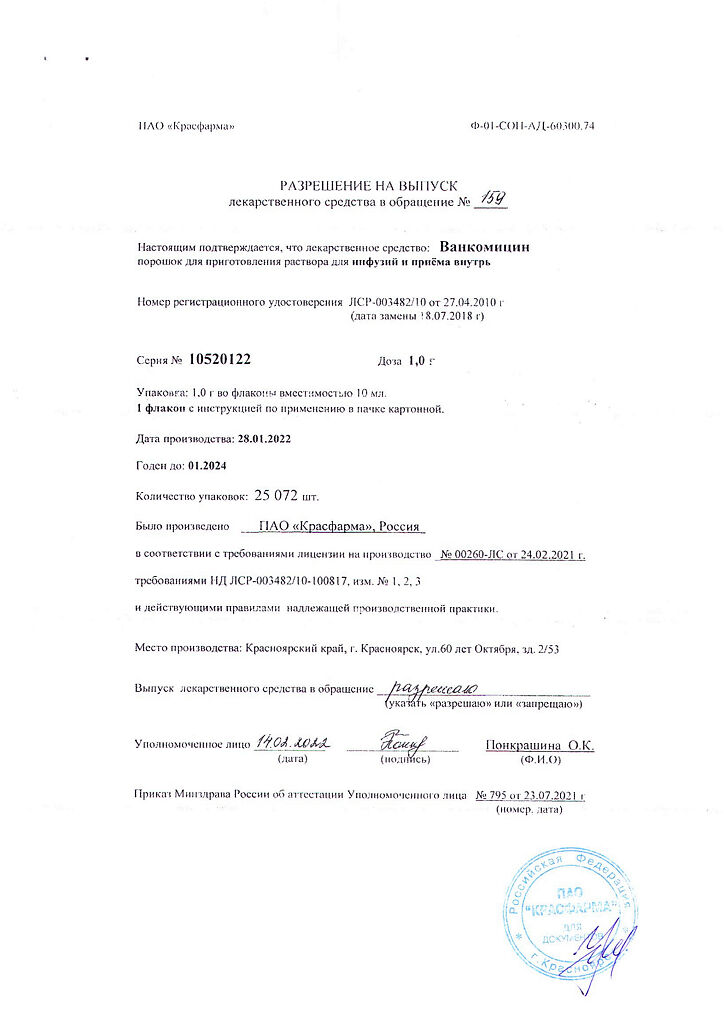
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | The drug should be stored in a dry place, protected from light, out of reach of children at a temperature not exceeding 8 ° C. |
| Manufacturer | Kraspharma PJSC, Russia |
| Medication form | lyophilizate |
| Brand | Kraspharma PJSC |
Related products
Buy Vancomycin, lyophilizate and oral administration 1 g with delivery to USA, UK, Europe and over 120 other countries.