No products in the cart.
Description
Pharmacodynamics
Valacyclovir is a nucleoside inhibitor of DNA polymerase of herpes viruses. It blocks the synthesis of viral DNA and viral replication. In humans valacyclovir is completely converted to acyclovir and L-valine. In vitro acyclovir has specific inhibitory activity against herpes simplex virus (HPV, Herpes simplex) types 1, 2, varicella zoster virus (VZV, Varicella zoster), CMV, Epstein-Barr virus (VEB) and human herpes virus type 6.
Acyclovir inhibits the synthesis of viral DNA immediately after phosphorylation and transformation into the active form – acyclovir triphosphate. The first stage of phosphorylation occurs with the participation of virus-specific enzymes.
For HPV, VZV and VEB viruses this enzyme is viral thymidine kinase, which is present in virus-affected cells. Partial selectivity of phosphorylation is retained in CMV and is mediated through the product of the phosphotransferase gene UL 97. Activation of acyclovir by a specific viral enzyme largely explains its selectivity.
The process of acyclovir phosphorylation (conversion from mono- to triphosphate) is completed by cellular kinases. Acyclovir triphosphate competitively inhibits viral DNA polymerase and, being a nucleoside analog, is incorporated into viral DNA, which leads to obligate breaking of the chain, cessation of DNA synthesis and, consequently, blocking of viral replication.
In immunocompromised patients, viruses with hypersensitivity to Valacyclovir are extremely rare (less than 0.1%), but may occasionally be found in patients with severe immune impairments, such as those treated with bone marrow transplants, those receiving chemotherapy for malignancies, and those who are HIV-infected.
Resistance is caused by a thymidine kinase deficiency in the virus, which leads to excessive spread of the virus in the host. Sometimes decreased sensitivity to acyclovir is due to the emergence of virus strains with disrupted viral thymidine kinase or DNA polymerase structure. The virulence of these varieties of the virus is similar to that of its wild strain.
Pharmacokinetics
Assimilation. After oral administration valacyclovir is well absorbed from the gastrointestinal tract, quickly and almost completely converted to acyclovir and valine. This conversion is catalyzed by liver enzyme – valacyclovir hydrolase. After a single dose of 250-2000 mg of valacyclovir, the average Cmax of acyclovir in plasma in healthy volunteers with normal renal function is on average 10-37 µmol/L (2.2-8.3 µg/ml) and the average Tmax is 1-2 hours.
The bioavailability of acyclovir is 54% when valacyclovir is taken at a dose of 1000 mg or more and is independent of food intake. Cmax of valacyclovir in plasma is only 4% of the concentration of acyclovir, Tmax on average is 30-100 minutes after taking the drug; after 3 hours the Cmax level remains the same or decreases. Valacyclovir and acyclovir have similar pharmacokinetic parameters after oral administration.
Distribution. Protein binding of valacyclovir is 13-18%, acyclovir is 9-33%. Acyclovir is well distributed in tissues and body fluids, including brain, kidney, lung, liver, aqueous humor, tear fluid, intestine, muscle, spleen, uterus, mucous membrane and vaginal secretion, semen, amniotic fluid, cerebrospinal fluid (50% of concentration in plasma), herpes vesicle fluid. The highest concentrations are produced in the kidneys, liver, and intestine. It penetrates through the placenta and into the breast milk.
Evacuation. Valacyclovir is excreted with the urine, mainly as acyclovir (more than 30% of the dose) and its metabolite 9-carboxymethoxymethylguanine; less than 1% of the drug is excreted unchanged. T1/2 of valacyclovir is less than 30 minutes, of acyclovir – 2.5-3.3 hours. In elderly patients (65-83 years old) T1/2 of acyclovir is 3.3-3.7 hours, and in patients with terminal renal failure – about 14 hours.
The pharmacokinetics of valacyclovir and acyclovir are not significantly impaired in patients infected with HPV and VZV.
In HIV-infected patients, the pharmacokinetic parameters of acyclovir after oral administration of valacyclovir at doses of 1000 and 2000 mg are comparable to those observed in healthy volunteers.
In organ transplant recipients receiving valacyclovir at a dose of 2000 mg 4 times daily, the Cmax of acyclovir was equal to or greater than that of healthy volunteers receiving the same dose of the drug, and the daily AUC values were significantly higher.
In late pregnancy, the sustained daily AUC after receiving 1000 mg of valacyclovir was approximately 2 times greater than that of acyclovir at a dose of 1200 mg/day.
Indications
Indications
Adults:
treatment of herpes zoster (the drug helps relieve pain, reduces its duration and the percentage of patients with pain caused by herpes zoster, including acute and postherpetic neuralgia);
treatment of infections of the skin and mucous membranes caused by the Herpes simplex virus type 1.2, including newly diagnosed and recurrent genital herpes (Herpes genitalis), as well as labial herpes (Herpes labialis);
prevention (suppression) of recurrent infections of the skin and mucous membranes caused by the Herpes simplex virus type 1.2, including genital herpes;
prevention of transmission of the genital herpes virus to a healthy partner when using the drug as suppressive therapy in combination with safe sex;
Adults and children aged 12 years and older: prevention of cytomegalovirus (CMV) infection, as well as acute graft rejection (in patients with kidney transplants), opportunistic infections and other herpesvirus infections (HSV, VZV) after organ transplantation.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Valaciclovir is a nucleoside inhibitor of DNA polymerase of herpes viruses. Blocks viral DNA synthesis and viral replication. In the human body, valacyclovir is completely converted into acyclovir and L-valine. Acyclovir in vitro has specific inhibitory activity against herpes simplex viruses (HSV, Herpes simplex) types 1, 2, varicella zoster virus and herpes zoster (VZV – varicella-zoster virus, Varicella zoster), CMV, Epstein-Barr virus (EBV) and human herpes virus type 6.
Acyclovir inhibits the synthesis of viral DNA immediately after phosphorylation and conversion to the active form – acyclovir triphosphate. The first stage of phosphorylation occurs with the participation of virus-specific enzymes.
For the HSV, VZV and EBV viruses, this enzyme is viral thymidine kinase, which is present in cells affected by the virus. Partial phosphorylation selectivity is conserved in CMV and is mediated through the phosphotransferase gene product UL 97. Activation of acyclovir by a specific viral enzyme largely explains its selectivity.
The process of phosphorylation of acyclovir (conversion from mono-to triphosphate) is completed by cellular kinases. Acyclovir triphosphate competitively inhibits viral DNA polymerase and, being a nucleoside analogue, is incorporated into viral DNA, which leads to obligate chain breakage, cessation of DNA synthesis and, consequently, blocking of viral replication.
In patients with preserved immunity, HSV and VZV viruses with reduced sensitivity to valacyclovir are extremely rare (less than 0.1%), but can sometimes be detected in patients with severe immune disorders, for example with a bone marrow transplant, in those receiving chemotherapy for malignant neoplasms and in HIV-infected patients.
Resistance is caused by a deficiency of the virus’ thymidine kinase, which leads to excessive spread of the virus in the host. Sometimes a decrease in sensitivity to acyclovir is due to the emergence of virus strains with a violation of the structure of the viral thymidine kinase or DNA polymerase. The virulence of these variants of the virus resembles that of the wild strain.
Pharmacokinetics
Suction. After oral administration, valacyclovir is well absorbed from the gastrointestinal tract and is quickly and almost completely converted to acyclovir and valine. This transformation is catalyzed by the liver enzyme, valacyclovir hydrolase. After a single dose of 250-2000 mg of valacyclovir, the average Cmax of acyclovir in blood plasma in healthy volunteers with normal renal function averages 10-37 µmol/L (2.2-8.3 µg/ml), and the average Tmax is 1-2 hours.
When taking valacyclovir in a dose of 1000 mg or more, the bioavailability of acyclovir is 54% and does not depend on food intake. Cmax of valacyclovir in blood plasma is only 4% of the concentration of acyclovir, Tmax on average is 30–100 minutes after taking the drug; after 3 hours, the Cmax level remains the same or decreases. Valacyclovir and acyclovir have similar pharmacokinetic parameters after oral administration.
Distribution. Protein binding of valacyclovir is 13–18%, acyclovir is 9–33%. Acyclovir is well distributed in tissues and body fluids, including the brain, kidneys, lungs, liver, aqueous humor, tear fluid, intestines, muscles, spleen, uterus, mucous membrane and vaginal secretions, sperm, amniotic fluid, cerebrospinal fluid (50% of the concentration in plasma), fluid of herpetic vesicles. The highest concentrations are created in the kidneys, liver and intestines. Penetrates through the placenta and into breast milk.
Excretion. Valaciclovir is excreted in the urine, mainly in the form of acyclovir (more than 30% of the dose) and its metabolite 9-carboxymethoxymethylguanine; less than 1% of the drug is excreted unchanged. T1/2 of valacyclovir is less than 30 minutes, acyclovir – 2.5–3.3 hours. In elderly patients (65-83 years), T1/2 of acyclovir is 3.3-3.7 hours, and in patients with end-stage renal failure – approximately 14 hours.
The pharmacokinetics of valacyclovir and acyclovir are not significantly affected in patients infected with the HSV and VZV viruses.
In HIV-infected patients, the pharmacokinetic parameters of acyclovir after oral administration of valacyclovir at doses of 1000 and 2000 mg are comparable to those observed in healthy volunteers.
In organ transplant recipients receiving valacyclovir 2000 mg 4 times daily, acyclovir Cmax was equal to or greater than that of healthy volunteers receiving the same dose of the drug, and daily AUC values were significantly higher.
In late pregnancy, the steady-state daily AUC after taking 1000 mg of valacyclovir was approximately 2 times greater than that after taking acyclovir at a dose of 1200 mg/day.
Special instructions
Special instructions
In patients at risk of dehydration, especially in elderly patients, adequate fluid replacement must be ensured during the treatment period.
Since acyclovir is excreted by the kidneys, the dose of Valcicon should be adjusted depending on the degree of renal impairment. Patients with renal failure are at increased risk of developing neurological complications and should be closely monitored. As a rule, these reactions are reversible and disappear after discontinuation of the drug.
In patients with chronic renal failure (CRF), it is recommended that creatinine clearance be determined frequently, especially during periods when renal function is rapidly changing (particularly immediately after transplantation or engraftment), and the dose of valacyclovir is adjusted according to creatinine clearance.
There are no data on the use of valacyclovir in high doses (4 g or more per day) in patients with liver disease, so high doses of Valcicon should be administered to them with caution.
Suppressive therapy with valacyclovir reduces the risk of transmission of genital herpes, but does not eliminate the risk of infection and does not lead to a complete cure. Therapy with Valcicon is recommended in combination with safe sex.
Taking the drug in high doses for a long time in conditions accompanied by severe immunodeficiency (bone marrow transplantation, clinical forms of HIV infection, kidney transplantation) led to the development of thrombocytopenic purpura and hemolytic-uremic syndrome, including death.
If side effects from the central nervous system occur (including agitation, hallucinations, confusion, delirium, convulsions and encephalopathy), the drug is discontinued.
Impact on driving vehicles and machinery
There is no data on the effect of valacyclovir, used in therapeutic doses, on the ability to drive vehicles and machines. However, when assessing the patient’s ability to drive a car or move machinery, it must be taken into account that side effects from the central nervous system may occur, so caution should be exercised.
Active ingredient
Active ingredient
Valaciclovir
Composition
Composition
1 film-coated tablet contains:
active ingredient:
valacyclovir hydrochloride – 556.00 mg (in terms of valacyclovir 500.00 mg);
excipients:
microcrystalline cellulose – 95.00 mg,
hyprolose (hydroxypropylcellulose) – 14.00 mg,
crospovidone – 28.00 mg,
magnesium stearate – 7.00 mg;
film shell:
hypromellose – 10.5 mg;
hyprolose (hydroxypropylcellulose) – 4.07 mg;
talc – 4.12 mg;
titanium dioxide – 2.31 mg or dry mixture for film coating white (hypromellose – 50%, hydroxypropylcellulose – 19.4%, talc – 19.6%, titanium dioxide – 11%) – 21 mg.
Pregnancy
Pregnancy
There are limited data on the use of valacyclovir during pregnancy.
Valacyclovir is used only when the potential benefit to the mother outweighs the possible risk to the fetus. Reported data on pregnancy outcomes in women taking valacyclovir or acyclovir (the active metabolite of valacyclovir) have not shown an increase in the number of birth defects in their children compared with the general population.
Since the registry included a small number of women who took valacyclovir during pregnancy, reliable and definite conclusions about the safety of valacyclovir during pregnancy cannot be made.
Acyclovir, the main metabolite of valacyclovir, is excreted in breast milk. After taking valacyclovir orally at a dose of 500 mg, Cmax of acyclovir in breast milk is 0.5-2.3 times
(on average 1.4 times) exceeded the corresponding concentrations of acyclovir in the maternal blood plasma.
The mean concentration of acyclovir in breast milk was 2.24 μg/ml (9.95 μmol/L). When the mother takes valacyclovir orally at a dose of 500 mg 2 times a day, the child will be exposed to the same acyclovir as when taking oral acyclovir at a dose of about 0.61 mg/kg/day.
Contraindications
Contraindications
hypersensitivity to valacyclovir, acyclovir and/or any other component included in the drug;
HIV infection with a CD4+ lymphocyte count of less than 100 in 1 μl;
children’s age (up to 12 years for the prevention of CMV infection after transplantation, up to 18 years for other indications).
With caution: liver/renal failure; old age; hypohydration; simultaneous use of nephrotoxic drugs; pregnancy; lactation period; clinically expressed forms of HIV infection.
Side Effects
Side Effects
From the central nervous system: headache, dizziness, psychotic symptoms, agitation, decreased mental capacity, ataxia, coma, confusion or depression of consciousness, dysarthria, encephalopathy, mania, hallucinations, convulsions, tremor.
These reactions are reversible and are usually observed in patients with impaired renal function or against the background of other predisposing conditions. In patients with a transplanted organ receiving valacyclovir in high doses (8 g/day) for the prevention of cytomegalovirus infection, neurological reactions develop more often than when taken in lower doses.
From the respiratory system: dyspnea.
From the digestive system: nausea, abdominal discomfort, vomiting, diarrhea, reversible disorders of liver function tests (increased activity of alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase), which are sometimes regarded as manifestations of hepatitis.
From the hematopoietic system: leukopenia (mainly observed in patients with reduced immunity), thrombocytopenia, anemia, thrombotic thrombocytopenic purpura.
From the skin: erythema multiforme, rashes, photosensitivity, alopecia.
Allergic reactions: itching, urticaria, angioedema, anaphylaxis.
From the urinary system: pain in the projection of the kidneys, renal dysfunction, incl. acute renal failure, renal colic. Renal colic may be associated with impaired renal function.
From the senses: visual impairment.
Laboratory indicators: decreased hemoglobin content, hypercreatininemia.
Other: dysmenorrhea, nasopharyngitis, respiratory tract infections, increased blood pressure, tachycardia, fatigue; in patients with severe immunocompromise, especially in adult patients with advanced HIV infection, receiving valacyclovir in high doses
(8 g/day daily) for a long time, cases of renal failure, microangiopathic hemolytic anemia and thrombocytopenia (sometimes in combination) have been observed. Similar adverse reactions have been observed in patients with the same diseases, but not receiving valacyclovir.
Interaction
Interaction
Cimetidine and tubular secretion blockers reduce the effect (they reduce the rate, but not the completeness of conversion to acyclovir). No dosage adjustment is required in individuals with normal creatinine clearance.
Nephrotoxic drugs increase the risk of developing renal dysfunction. Caution should be exercised (monitor changes in renal function) when combining Valcicon in higher doses (4 g per day or more) with drugs that affect other renal functions (for example: cyclosporine, tacrolimus).
Acyclovir is excreted by the kidneys, mainly unchanged, through active renal secretion. Concomitant use of drugs with this elimination mechanism may lead to increased plasma concentrations of acyclovir.
After prescribing Valcicon at a dose of 1000 mg, cimetidine and probenecid, which are eliminated in the same way as valacyclovir, increase the AUC value of acyclovir and thus reduce its renal clearance. Due to the wide therapeutic index of acyclovir, dose adjustment of Valcicon is not required in this case.
Caution must be exercised in the case of simultaneous use of valacyclovir in higher doses (4 g per day or higher) and drugs that compete with acyclovir for the elimination pathway, since there is a potential threat of increased plasma levels of one or both drugs or their metabolites.
An increase in the AUC of acyclovir and the inactive metabolite mycophenolate mofetil was observed when these drugs were used simultaneously.
The pharmacokinetics of valacyclovir does not change when taken concomitantly with digoxin, aluminum/magnesium-containing antacids, and thiazide diuretics.
Overdose
Overdose
Symptoms: In case of an overdose of valacyclovir, acute renal failure and the development of neurological symptoms may occur, including confusion, hallucinations, agitation, depression of consciousness and coma, nausea and vomiting are also noted. To prevent overdose, caution should be exercised when using the drug.
Many cases of overdose have been associated with the use of the drug to treat patients with impaired renal function and elderly patients due to non-compliance with the dosage regimen (repeatedly receiving doses of valacyclovir that exceed the recommended ones).
Treatment. Patients should be closely monitored for timely diagnosis of toxic manifestations. Hemodialysis significantly accelerates the elimination of acyclovir from blood plasma and can be considered the optimal treatment method in case of symptomatic overdose.
Storage conditions
Storage conditions
In a place protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Vertex, Russia
Additional information
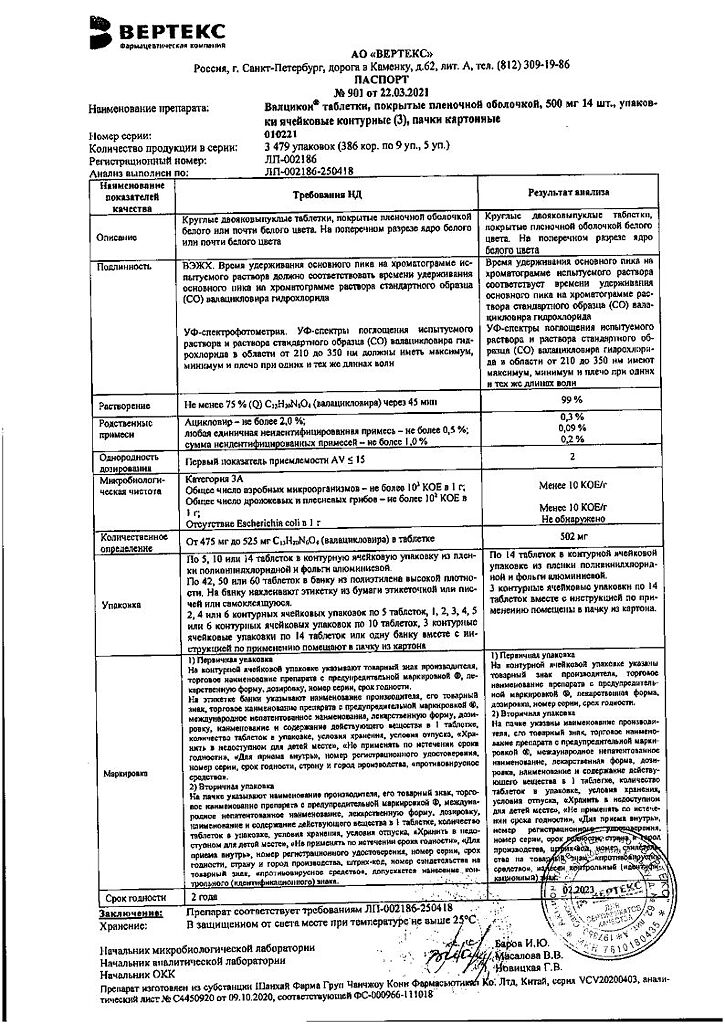
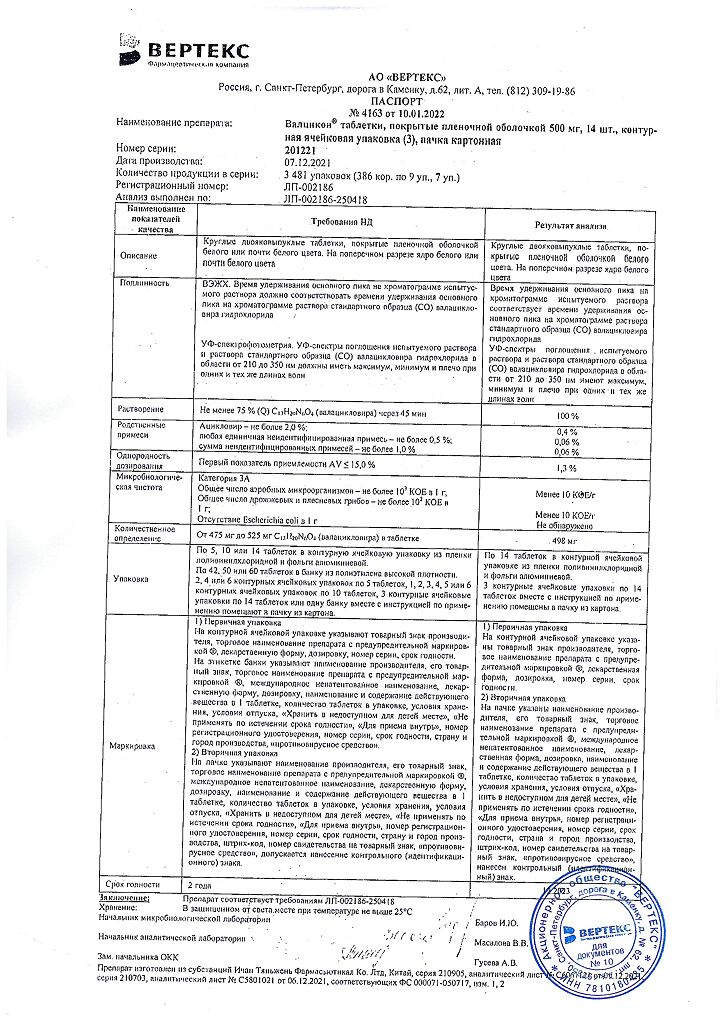
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a light-protected place, at a temperature not exceeding 25 °C |
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Related products
Buy Valcicon, 500 mg 42 pcs with delivery to USA, UK, Europe and over 120 other countries.