No products in the cart.
Tulip, 10 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Tulip is hypolipidemic.
Pharmacodynamics
Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, the enzyme involved in the conversion of 3-hydroxy-3-methylglutaryl-coenzyme A to mevalonate, a precursor of steroids, including cholesterol.including cholesterol. Cholesterol and triglycerides (TG) circulate in the vascular bed as part of lipoprotein molecules. From triglycerides and cholesterol, LDL are synthesized in the liver. From the liver they enter blood plasma and are delivered to peripheral tissues. LDL are formed from LDLNP, their catabolism is carried out mainly through interaction with LDL receptors.
Atorvastatin reduces LDL cholesterol synthesis and content, total cholesterol content, apolipoprotein B in patients with homozygous and heterozygous familial hypercholesterolemia, primary hypercholesterolemia and mixed hyperlipidemia. It also causes decreases in LDL cholesterol and triglyceride levels and increases in HDL-cholesterol and apolipoprotein A levels.
. Atorvastatin reduces total cholesterol, LDL-cholesterol, HDL-cholesterol, apolipoprotein B, triglycerides and non-LDL-cholesterol levels and increases HDL-cholesterol levels in patients with isolated hypertriglyceridemia, LDL-cholesterol levels in patients with dysbetalipoproteinemia. Like LDL, cholesterol-rich and triglyceride-rich lipoproteins (LDLNP, intermediate-density lipoproteins, and chylomicron residues) may also contribute to the progression of atherosclerosis. Elevated plasma triglyceride levels are often combined with decreased HDL levels and the appearance of small LDL particles, as well as other non-lipid metabolic risk factors for CHD.
Pharmacokinetics
Absorption and distribution
Absorption is high. Cmax in plasma after oral administration is reached after 1-2 h. Cmax in women is 20% higher, AUC is 10% lower than in men. Cmax in patients with alcoholic liver cirrhosis (class B according to Child-Pugh scale) is 16 times higher, and AUS is 11 times higher than normal.
Eating slightly reduces the rate and degree of absorption of the drug (by 25 and 9%, respectively), but the decrease in LDL cholesterol is similar to that of atorvastatin without concomitant ingestion.
After oral administration of atorvastatin in the evening, plasma concentrations are lower (Cmax and AUC approximately by 30%) than after administration in the morning, but decrease in LDL-cholesterol concentration is independent of the time of day in which the drug is taken. A linear correlation between the degree of absorption and the dose of the drug was found.
The bioavailability is 12%, the systemic bioavailability of HMG-CoA reductase inhibitory activity is about 30%. Low systemic bioavailability is due to presystemic metabolism in the gastrointestinal tract and during first passage through the liver.
The average Vd is 381 liters, the binding to plasma proteins is 98%.
It is metabolized mainly in the liver under the action of cytochrome P4503A4 with the formation of pharmacologically active metabolites (ortho- and parahydroxylated derivatives, beta-oxidation products). Tulip® (tablets 10 and 20 mg) causes a decrease of total cholesterol levels by 29 and 33%, LDL-cholesterol by 39 and 43%, apolipoprotein B by 32 and 35% and triglycerides by 14 and 26%. HDL-cholesterol level in this case increases by 6 and 9%, respectively. It is excreted mainly with bile after hepatic and/or extrahepatic metabolism (atorvastatin does not undergo marked intestinal-hepatic recirculation and is not excreted with hemodialysis). T1/2 – 14 h. Inhibitory activity against HMG-CoA reductase persists for about 20-30 hours due to the presence of active metabolites. Less than 2% of the oral dose of the drug is determined in the urine.
Indications
Indications
elevated blood cholesterol levels
coronary heart disease
coronary atherosclerosis.
Pharmacological effect
Pharmacological effect
Tulip – hypolipidemic.
Pharmacodynamics
Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, an enzyme involved in the conversion of 3-hydroxy-3-methylglutaryl coenzyme A to mevalonate, a precursor to steroids, including cholesterol. Cholesterol and triglycerides (TG) circulate in the vascular bed as part of lipoprotein molecules. VLDL is synthesized from triglycerides and cholesterol in the liver. From the liver they enter the blood plasma and are delivered to peripheral tissues. LDL is formed from VLDL and is catabolized mainly through interaction with LDL receptors.
Atorvastatin reduces the synthesis and content of LDL cholesterol, total cholesterol, and apolipoprotein B in patients with homozygous and heterozygous familial hypercholesterolemia, primary hypercholesterolemia and mixed hyperlipidemia. It also causes a decrease in VLDL cholesterol and triglycerides and an increase in HDL cholesterol and apolipoprotein A.
Atorvastatin reduces the content of total cholesterol, LDL cholesterol, VLDL cholesterol, apolipoprotein B, triglycerides and non-HDL cholesterol and increases the level of HDL cholesterol in patients with isolated hypertriglyceridemia, and the level of HDL cholesterol in patients with dysbetalipoproteinemia. Like LDL, cholesterol-rich and triglyceride-rich lipoproteins (VLDL, intermediate-density lipoproteins, and chylomicron remnants) may also contribute to the progression of atherosclerosis. An increase in plasma triglyceride levels is often combined with a decrease in HDL levels and the appearance of small LDL particles, as well as other non-lipid metabolic risk factors for coronary artery disease.
Pharmacokinetics
Absorption and distribution
Absorption is high. Cmax in blood plasma after oral administration is achieved within 1–2 hours. Cmax in women is 20% higher, AUC is 10% lower than in men. Cmax in patients with alcoholic cirrhosis (class B on the Child-Pugh scale) is 16 times higher, and AUC is 11 times higher than normal.
Eating slightly reduces the rate and extent of drug absorption (by 25 and 9%, respectively), but the reduction in LDL-cholesterol is similar to that when using atorvastatin without simultaneous food intake.
After oral administration of atorvastatin in the evening, plasma concentrations are lower (Cmax and AUC by approximately 30%) than after administration in the morning, however, the reduction in LDL-cholesterol concentrations does not depend on the time of day at which the drug is taken. A linear relationship was revealed between the degree of absorption and the dose of the drug.
Bioavailability is 12%, systemic bioavailability of inhibitory activity against HMG-CoA reductase is about 30%. Low systemic bioavailability is due to first-pass metabolism in the gastrointestinal tract and during the first passage through the liver.
Average Vd – 381 l, binding to blood plasma proteins – 98%.
Metabolized primarily in the liver under the influence of cytochrome P4503A4 with the formation of pharmacologically active metabolites (ortho- and parahydroxylated derivatives, beta-oxidation products). Tulip® (10 and 20 mg tablets) causes a decrease in total cholesterol by 29 and 33%, LDL cholesterol by 39 and 43%, apolipoprotein B by 32 and 35%, and triglycerides by 14 and 26%. The level of HDL cholesterol increases by 6 and 9%, respectively. It is excreted mainly in bile after hepatic and/or extrahepatic metabolism (atorvastatin does not undergo significant enterohepatic recirculation and is not excreted by hemodialysis). T1/2 – 14 hours. Inhibitory activity against HMG-CoA reductase lasts about 20-30 hours due to the presence of active metabolites. Less than 2% of the dose taken orally is determined in the urine.
Special instructions
Special instructions
Liver dysfunction. The use of HMG-CoA reductase inhibitors to reduce blood lipid levels can lead to changes in biochemical parameters reflecting liver function.
Liver function should be monitored before starting treatment, 6 weeks, 12 weeks after starting Tulip® and after each dose increase, as well as periodically, for example, every 6 months. Changes in liver enzyme activity are usually observed within the first three months after starting Tulip®. Patients who experience elevated transaminase levels should be monitored until enzyme levels return to normal. If ALT or AST values are more than 3 times higher than the upper permissible limit, it is recommended to reduce the dose of Tulip® or discontinue treatment.
Skeletal muscles. Patients with diffuse myalgia, muscle flaccidity or weakness, and/or significantly elevated CPK are at risk for the development of myopathy (defined as muscle pain with a concomitant increase in CPK levels greater than 10 times the upper limit of normal).
When prescribing combination therapy with Tulip® and cyclosporine, fibric acid derivatives, erythromycin, clarithromycin, immunosuppressants and azole antifungals, as well as lipid-lowering doses of niacin, it is necessary to weigh the potential benefits and risks of this treatment and monitor patients who develop signs or symptoms of muscle pain, lethargy or weakness, especially during the first months of treatment and when increasing the dose of any of the drugs.
Treatment with Tulip® should be temporarily suspended or discontinued if a serious condition develops that may result from myopathy, as well as in the presence of risk factors for the development of acute renal failure due to rhabdomyolysis (for example, acute severe infection, arterial hypotension, major surgery, trauma, severe metabolic and endocrine disorders, as well as electrolyte imbalances).
The patient should immediately consult a doctor if unexplained muscle pain or weakness occurs, especially if it is accompanied by malaise and fever. Women of reproductive age should use reliable methods of contraception.
Impact on the ability to drive vehicles and engage in other activities that require concentration and speed of psychomotor reactions
Tulip® does not affect the ability to drive a car or operate machinery.
Active ingredient
Active ingredient
Atorvastatin
Composition
Composition
1 tablet contains:
Active ingredient:
atorvastatin (in the form of calcium salt) 10 mg;
Excipients:
microcrystalline cellulose,
lactose monohydrate,
sodium croscarmellose,
hydroxypropylcellulose,
polysorbate 80,
magnesium oxide heavy,
colloidal silicon dioxide,
magnesium stearate;
Shell composition:
hypromellose, hydropropylcellulose, titanium dioxide (E171), polyethylene glycol 6000, talc.
Pregnancy
Pregnancy
Use during pregnancy and breastfeeding is contraindicated.
Contraindications
Contraindications
hypersensitivity to atorvastatin and other excipients of the drug;
liver diseases in the active stage (including active chronic hepatitis, chronic alcoholic hepatitis); increased ALT or AST activity (more than 3 times the upper limit of normal) of unknown origin; liver failure (grades A and B on the Child-Pug scale);
women of reproductive age who do not use adequate methods of contraception.
With caution: history of liver disease, alcohol abuse, severe electrolyte imbalance, endocrine and metabolic disorders, arterial hypotension, severe acute infections (sepsis), uncontrolled epilepsy, skeletal muscle diseases, extensive surgical interventions, trauma, childhood (efficacy and safety of use have not been established).
Side Effects
Side Effects
Digestive system: in more than 2% of cases – nausea; in less than 2% – heartburn, constipation or diarrhea, flatulence, abdominal pain, anorexia, decreased or increased appetite, dry mouth, belching, dysphagia, vomiting, stomatitis, esophagitis, glossitis, erosive and ulcerative lesions of the oral cavity, gastroenteritis, hepatitis, biliary colic, cheilitis, duodenal ulcer, pancreatitis, cholestatic jaundice, liver dysfunction, melena, bleeding gums, tenesmus.
Respiratory system: in more than 2% of cases – bronchitis, rhinitis; less often – pneumonia, dyspnea, bronchial asthma, nosebleeds.
Nervous system: in more than 2% of cases – insomnia, dizziness; in less than 2% – headache, asthenia, malaise, drowsiness, unusual dreams, paresthesia, amnesia, emotional lability, peripheral neuropathy, ataxia, facial paralysis, hyperkinesis, depression, hyperesthesia, loss of consciousness.
Musculoskeletal system: in more than 2% of cases – arthritis; in less than 2% – leg muscle cramps, bursitis, tenosynovitis, myositis, myopathy, arthralgia, myalgia, joint contractures, stiff neck muscles, rhabdomyolysis.
Allergic reactions: in less than 2% of cases – itching, skin rash, contact dermatitis; rarely – urticaria, anaphylaxis, Quincke’s edema, exudative erythema multiforme (Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), photosensitivity.
Skin: in less than 2% of cases – alopecia, sweating, eczema, seborrhea, ecchymosis, petechiae.
Genitourinary system: in more than 2% of cases – urogenital infections, peripheral edema; in less than 2% of cases – dysuria (including pollakiuria, nocturia, urinary incontinence or urinary retention, imperative urge to urinate), nephritis, hematuria, vaginal bleeding, urolithiasis, epididymitis, decreased libido, impaired ejaculation, impotence, uterine bleeding.
Sense organs: in less than 2% of cases – amblyopia, tinnitus, dry conjunctiva, impaired accommodation, hemorrhages in the eyes, deafness, increased intraocular pressure, parosmia, taste perversion, loss of taste.
Cardiovascular system: in more than 2% of cases – chest pain; in less than 2% – palpitations, vasodilation, orthostatic hypotension, phlebitis, arrhythmia, angina pectoris, increased blood pressure.
Hematopoietic system: in less than 2% of cases – anemia, lymphadenopathy, thrombocytopenia.
Laboratory indicators: in less than 2% of cases – hyperglycemia, hypoglycemia, increased levels of creatine phosphokinase (CPK), albuminuria.
Other: in less than 2% of cases – weight gain, gynecomastia, exacerbation of gout, mastodynia.
Interaction
Interaction
Antacids: with the simultaneous administration of atorvastatin and antacid drugs in the form of a suspension containing magnesium and aluminum hydroxide, the concentration of atorvastatin in the blood plasma is reduced by approximately 35%, while the degree of reduction in LDL cholesterol remains unchanged.
Colestipol: with simultaneous use of atorvastatin and colestipol, the concentration of atorvastatin in the blood plasma is reduced by approximately 25%, while the lipid-lowering effect of the combination of atorvastatin and colestipol is superior to that of each drug separately.
Digoxin: with repeated simultaneous administration of atorvastatin and digoxin, the concentration of digoxin in the blood plasma increases by approximately 20%, and therefore the patient should be monitored.
Erythromycin: When atorvastatin is taken concomitantly with erythromycin, which has an inhibitory effect on cytochrome P450 CYP3A4, the plasma concentration of atorvastatin increases by approximately 40%.
Oral contraceptives: When atorvastatin is coadministered with oral contraceptives, AUC values increase by approximately 30% for norethisterone and 20% for ethinyl estradiol. These data should be taken into account when selecting contraceptives for patients taking atorvastatin.
Warfarin: in patients taking warfarin for a long time, atorvastatin slightly reduces the prothrombin time in the first days after the start of its use, however, after 15 days this indicator returns to normal. After prescribing atorvastatin, patients taking warfarin should have their PT monitored more frequently than usual.
With the simultaneous administration of cyclosporine, fibrates, clarithromycin, antifungal drugs (related to azoles) and nicotinamide, the concentration of atorvastatin in the blood plasma (the risk of myopathy) increases.
Overdose
Overdose
There is no specific treatment in case of Tulip overdose.
Treatment is symptomatic; take measures to maintain vital functions and prevent further absorption of the drug (gastric lavage, taking activated charcoal).
Due to the fact that the drug actively binds to blood plasma proteins, hemodialysis does not seem to be an effective way to accelerate its removal from the body.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
2 years
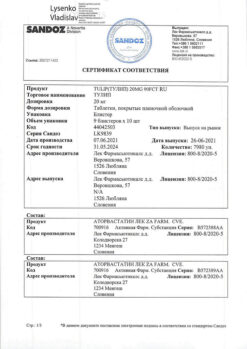
Manufacturer
Manufacturer
Lek d.d., Slovenia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Lek d.d., Slovenia |
| Medication form | pills |
| Brand | Lek d.d. |
Other forms…
Related products
Buy Tulip, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.