No products in the cart.
Tugeo SoloStar, 300 units/ml 1.5 ml cartridges in SoloStar syringe pens 3 pcs
€80.10 €66.75
Out of stock
(E-mail when Stock is available)
Description
Pharmacological action – hypoglycemic.
Pharmacodynamics
The most important action of insulin, including insulin glargine, is the regulation of glucose metabolism. Insulin and its analogues decrease blood glucose concentration by stimulating glucose uptake by peripheral tissues (especially skeletal muscle and adipose tissue) and inhibiting glucose formation in the liver. Insulin suppresses lipolysis in adipocytes (fat cells) and inhibits proteolysis while increasing protein synthesis.
Pharmacodynamic characteristics
Insulin glargine is an analog of human insulin, obtained by recombination of DNA of Escherichia coli bacteria (strain K12), used as a producer strain. It has a low solubility in a neutral medium. At pH 4 (in an acidic environment), insulin glargine is completely soluble. After injection into the subcutaneous fat, the acidic reaction of the solution is neutralized, resulting in the formation of microprecipitates from which small amounts of insulin glargin are continuously released.
The onset of action of b/c injected 100 IU/ml glargin insulin was slower compared to human insulin isophan, its action curve was smooth and devoid of peaks, and its duration of action was prolonged (data from euglycemic clamp studies performed in healthy volunteers and patients with type 1 diabetes).
The hypoglycemic action of Tujeo SoloStar® after p/q administration was more constant in value and more prolonged compared to p/q administration of insulin glargine 100 units/ml (data of 36-hour cross-over euglycemic clamp study in 18 patients with type 1 diabetes). The action of Tujeo SoloStar® lasted more than 24 hours (up to 36 hours) when administered by mouth at clinically relevant doses.
The prolonged hypoglycemic action of Tujeo SoloStar® lasting more than 24 hours allows the time of administration to be changed if necessary within 3 hours before or 3 hours after the patient’s usual time of injection (see “Dosage and Administration”).
Differences in the hypoglycemic action curves of Tujeo SoloStar® and insulin glargine 100 units/ml are due to changes in the release of insulin glargine from the precipitate.
For the same number of units of glargine insulin, the administered volume of Tugeo SoloStar® is one-third that of 100 U/ml glargine insulin. This results in a smaller precipitate surface area, allowing for a more gradual release of glargine insulin from the Tugeo SoloStar® precipitate compared to the 100 U/ml glargine insulin precipitate.
In intravenous administration of equal doses of insulin glargine and human insulin, their hypoglycemic effects were similar.
Binding to insulin receptors. Insulin glargin is metabolized to two active metabolites M1 and M2 (see Pharmacokinetics). In vitro studies have shown that the affinity of insulin glargine and its M1 and M2 metabolites for human insulin receptors is similar to that of human insulin.
Binding to IGF-1 receptors. The affinity of glargine insulin for the IGF-1 receptor is approximately 5-8 times higher than that of human insulin (but approximately 70-80 times lower than that of IGF-1), whereas compared to human insulin, glargine insulin metabolites M1 and M2 have slightly lower affinity for the IGF-1 receptor. The total therapeutic insulin concentration (the concentration of insulin glargine and its metabolites) determined in patients with type 1 diabetes was markedly lower than the concentration required for half-maximal binding to IGF-1 receptors and subsequent activation of the mitogen-proliferative pathway triggered through IGF-1 receptors. Physiological concentrations of endogenous IGF-1 can activate the mitogen-proliferative pathway, but the therapeutic insulin concentrations determined with insulin therapy, including treatment with Tujeo SoloStar®, are significantly lower than the pharmacological concentrations necessary to activate the mitogen-proliferative pathway.
The results from all clinical trials of Tugeo SoloStar® conducted with a total of 546 patients with type 1 diabetes and 2,474 patients with type 2 diabetes showed that the decrease in glycosylated hemoglobin (HbAlc) values compared to their baseline values by the end of the trials was no less than that of treatment with insulin glargine 100 units/ml.
The percentage of patients achieving the target HbA1c (below 7%) was comparable in both treatment groups.
The decrease in plasma glucose concentrations by the end of the study with Tugeo SoloStar® and insulin glargine 100 units/mL was similar, but with treatment with Tugeo SoloStar® the decrease was more gradual during the dose-fitting period.
Glycemic control, including improvement in HbAlc, was comparable when Tugeo SoloStar® was administered in the morning or evening, and changing the time of administration within 3 h before or 3 h after the patient’s usual time of administration had no effect on its effectiveness.
Patients treated with Tujeo SoloStar® showed an average weight change of less than 1 kg by the end of the 6-month therapy period.
The improvement in HbA1c was independent of gender, ethnicity, age, duration of diabetes (<10 and ≥10 years), HbAlc value at outcome (<8 or ≥8%), or BMI at outcome.
In patients with type 2 diabetes, clinical trial results have demonstrated a lower incidence of severe and/or confirmed hypoglycemia as well as documented hypoglycemia with clinical symptoms when treated with Tujeo SoloStar® compared to treatment with 100 units/mL insulin glargine.
The benefit of Tugeo SoloStar® over glargine 100 units/mL insulin in reducing the risk of severe and/or confirmed nocturnal hypoglycemia was shown in patients previously treated with oral hypoglycemic agents (23% risk reduction) or with insulin with meals (21% risk reduction) during the 9 weeks to the end of the study compared to treatment with glargine 100 units/mL insulin.
In the group of patients treated with Tujeo SoloStar® compared with patients treated with 100 U/mL insulin glargine, the reduction in risk of hypoglycemia was observed in both patients previously treated with insulin therapy and in patients not previously treated with insulin; the risk reduction was greater during the first 8 weeks of treatment (initial treatment period) and was independent of age, sex, race, BMI, and duration of diabetes (<10 and ≥10 years).
In patients with type 1 diabetes mellitus, the incidence of hypoglycemia during treatment with Tujeo SoloStar® was similar to that in patients treated with insulin glargine 100 units/ml. However, the incidence of nocturnal hypoglycemia (for all categories of hypoglycemia) during the initial treatment period was lower in patients treated with Tugeo SoloStar® compared to patients treated with 100 units/ml insulin glargine.
. In clinical trials, a single daily infusion of Tugeo SoloStar® in the evening, with a fixed infusion schedule (at the same time) or a flexible infusion schedule (at least twice weekly infusions were given 3 hours before or 3 hours after the usual infusion time, resulting in shortened intervals of up to 18 h or longer intervals of up to 30 h) had similar effects on HbA1c, fasting plasma glucose concentration (FPG), and mean preinjection plasma glucose concentration at self-determination. In addition, no differences in the incidence of hypoglycemia at any time of day or nocturnal hypoglycemia were observed when using Tugeo SoloStar® with fixed or flexible administration time schedules. Study results did not indicate any differences related to insulin antibody formation in efficacy, safety, or basal insulin dose between patients treated with Tugeo SoloStar® and insulin glargine 100 units/ml (see “Adverse Events”). The ORIGIN (Outcome Reduction with Initial Glargine Intervention) study was an international, multicenter, randomized study conducted in 12537 patients with impaired fasting glycemia (ADG), impaired glucose tolerance (IGT) or early stage type 2 diabetes and confirmed cardiovascular disease. Study participants were randomly allocated into groups – those receiving insulin glargine ≤100 units/mL (n=6264), which was titrated until reaching a GPA <5.3 mmol concentration, or standard treatment (n=6273). the mean follow-up period was approximately 6.2 years.
The median baseline HbA1c value was 6.4%. The median HbA1c during treatment ranged from 5.9-6.4% in the glargine insulin group and 6.2-6.6% in the standard treatment group over the entire follow-up period.
. The ORIGIN study showed that treatment with glargine insulin 100 units/ml, compared with standard hypoglycemic therapy, did not change the risk of cardiovascular complications (cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke), risk of revascularization procedure (coronary, carotid or peripheral arteries) or hospitalization for the development of heart failure, the risk of developing microvascular complications (combined index of microvascular complications: laser photocoagulation or vitrectomy, vision loss due to diabetic retinopathy, progression of albuminuria or doubling of the blood creatinine concentration index, or occurrence of the need for dialysis therapy).
In a five-year follow-up study evaluating the effect of insulin glargine 100 units/ml on the development of diabetic retinopathy in patients with type 2 diabetes there was no significant difference in the progression of diabetic retinopathy with treatment with insulin glargine 100 units/ml compared to insulin isophane.
Particular patient groups
Gender and race. There were no differences in efficacy and safety between Tugeo SoloStar® and insulin glargine 100 units/ml based on patient gender and race.
Elderly age. In controlled clinical trials, 716 patients (23% of the safety assessment population) with type 1 and 2 diabetes were ≥65 years of age and 97 patients (3%) were ≥75 years of age. Overall, there were no differences in efficacy or safety between these patients and younger patients. In elderly patients with diabetes mellitus, to avoid hypoglycemic reactions, the starting and maintenance doses should be lower and dose increases should be slower. In elderly patients it may be difficult to recognize hypoglycemia. Close monitoring of blood glucose concentrations is recommended, and the insulin dose should be adjusted individually (see “Dosage and administration” and “Pharmacokinetics”).
Renal insufficiency. In controlled clinical trials, a subgroup analysis based on renal functional status (determined at outcome by GFR <60 or ≥60 ml/min/1.73 m2 body surface area) showed no difference in safety or efficacy between Tugeo SoloStar® and insulin glargine 100 units/mL. Close monitoring of blood glucose concentrations is recommended, and the insulin dose should be adjusted individually (see Administration and Doses and Pharmacokinetics).
Patients with obesity. In clinical trials, a subgroup analysis based on BMI (up to 63 kg/m2) showed no difference in efficacy and safety between Tugeo SoloStar® and insulin glargine 100 units/mL.
Children. There are no data on the use of Tugeo SoloStar® in children.
Pharmacokinetics
Absorption and distribution. Following p/k injection of Tugeo SoloStar® in healthy volunteers and patients with diabetes, serum insulin concentrations indicate much slower and longer absorption, resulting in a flatter AUC curve for up to 36 h compared to insulin glargine 100 units/ml. The AUC curve of Tujeo SoloStar® was consistent with its pharmacodynamic activity curve. Css within the therapeutic concentration range was achieved after 3-4 days of daily use of Tugeo SoloStar®.
The variability in the same patient, defined as the coefficient of variation of systemic insulin exposure over 24 hours in the state of achieving Css, was low (17.4%) after a p/k injection of Tugeo SoloStar®.
Metabolism. In humans, insulin glargin is rapidly metabolized from the carboxyl end (C-end) of the β-chain to form two active metabolites M1 (21A-Gly insulin) and M2 (21A-Gly-des-30B-Thr-insulin) after p/c administration of Tugeo SoloStar®. Metabolite M1 predominantly circulates in blood plasma. Systemic exposure to M1 metabolite increases with increasing dose of Tujeo SoloStar®. Comparison of pharmacokinetic and pharmacodynamic data showed that the drug action is mainly due to systemic exposure of M1 metabolite. In the vast majority of patients, insulin glargine and M2 metabolite could not be detected in the systemic bloodstream. In cases where insulin glargin and metabolite M2 were detected in the blood, their concentrations were independent of the dose administered and the dosage form of insulin glargin.
Elimination. The T1/2 of metabolite M1, the quantitatively predominant metabolite of Tujeo SoloStar®, is 18-19 h after a p/k injection of the drug, regardless of the dose.
Particular patient groups
Gender and race. There is no information about the effect of race and gender on the pharmacokinetics of insulin glargine (see “Pharmacodynamics”).
Elderly age. The effect of age on the pharmacokinetics of Tujeo SoloStar® has not been studied at present. In elderly patients with diabetes mellitus, in order to avoid hypoglycemic reactions, the starting dose and maintenance dose should be lower and dose increases should be made more slowly (see “Pharmacodynamics” and “Dosage and administration”).
In children. In children, the pharmacokinetics of Tujeo SoloStar® have not been studied at this time.
Hepatic and renal insufficiency. The effect of renal and hepatic impairment on the pharmacokinetics of Tujeo SoloStar® has not been studied to date. However, some studies conducted with human insulin have shown increased insulin concentrations in patients with renal and hepatic impairment. Close monitoring of blood glucose concentrations and individual adjustment of insulin dose is recommended (see “Dosage and administration” and “Pharmacodynamics”).
Indications
Indications
Diabetes mellitus in adults requiring treatment with insulin.
Pharmacological effect
Pharmacological effect
Pharmacological action – hypoglycemic.
Pharmacodynamics
The most important action of insulin, incl. and insulin glargine, is the regulation of glucose metabolism. Insulin and its analogues reduce blood glucose concentrations by stimulating glucose uptake into peripheral tissues (especially skeletal muscle and adipose tissue) and inhibiting glucose production in the liver. Insulin suppresses lipolysis in adipocytes (fat cells) and inhibits proteolysis, while increasing protein synthesis.
Pharmacodynamic characteristics
Insulin glargine is an analogue of human insulin, obtained by recombining the DNA of Escherichia coli bacteria (strains K12), used as a producer strain. It has low solubility in neutral media. At pH 4 (in an acidic environment), insulin glargine is completely soluble. After injection into the subcutaneous fat, the acidic reaction of the solution is neutralized, which leads to the formation of microprecipitates, from which small amounts of insulin glargine are constantly released.
The onset of action of subcutaneously administered insulin glargine 100 U/mL was slower than that of human isophane insulin, its action curve was smooth and peak-free, and its duration of action was prolonged (euglycemic clamp studies in healthy volunteers and patients with type 1 diabetes mellitus).
The hypoglycemic effect of the drug Tujeo SoloStar® after its subcutaneous administration, compared with that with subcutaneous administration of insulin glargine 100 U/ml, was more constant in magnitude and more prolonged (data from a 36-hour crossover euglycemic clamp study conducted in 18 patients with type 1 diabetes mellitus). The effect of Tujeo SoloStar® lasted more than 24 hours (up to 36 hours) when administered subcutaneously in clinically significant doses.
The prolonged hypoglycemic effect of the drug Tujeo SoloStar®, lasting more than 24 hours, allows, if necessary, to change the time of administration of the drug within 3 hours before or 3 hours after the patient’s usual injection time (see “Dosage and Administration”).
Differences in the hypoglycemic action curves of Tujeo SoloStar® and insulin glargine 100 U/ml are associated with changes in the release of insulin glargine from the precipitate.
For the same number of units of insulin glargine, the administered volume of Tujeo SoloStar® is one third of that when administering 100 U/ml insulin glargine. This results in a decrease in the surface area of the precipitate, which provides a more gradual release of insulin glargine from the precipitate of Toujeo SoloStar® compared to the precipitate of insulin glargine 100 U/ml.
With intravenous administration of the same doses of insulin glargine and human insulin, their hypoglycemic effect was the same.
Connection with insulin receptors. Insulin glargine is metabolized to two active metabolites M1 and M2 (see Pharmacokinetics). In vitro studies have shown that the affinity of insulin glargine and its metabolites M1 and M2 for human insulin receptors is similar to that of human insulin.
Connection with IGF-1 receptors. The affinity of insulin glargine for the IGF-1 receptor is approximately 5-8 times higher than that of human insulin (but approximately 70-80 times lower than that of IGF-1), while at the same time, compared with human insulin, the insulin glargine metabolites M1 and M2 have slightly lower affinity for the IGF-1 receptor. Total therapeutic insulin concentrations (concentrations of insulin glargine and its metabolites) determined in patients with type 1 diabetes mellitus were markedly lower than the concentration required for half-maximal binding to IGF-1 receptors and subsequent activation of the mitogenic-proliferative pathway triggered through IGF-1 receptors. Physiological concentrations of endogenous IGF-1 can activate the mitogenic-proliferative pathway, however, therapeutic concentrations of insulin determined during insulin therapy, including treatment with Tujeo SoloStar®, are significantly lower than the pharmacological concentrations required to activate the mitogenic-proliferative pathway.
Results obtained from all clinical studies of Toujeo SoloStar®, conducted in a total of 546 patients with type 1 diabetes mellitus and 2474 patients with type 2 diabetes mellitus, showed that the decrease in glycosylated hemoglobin (HbAlc) values compared to their baseline values at the end of the studies was no less than that observed with treatment with insulin glargine 100 U/ml.
The percentage of patients achieving target HbA1c (below 7%) was comparable in both treatment groups.
The decrease in plasma glucose concentrations at the end of the study with Toujeo SoloStar® and insulin glargine 100 U/ml was the same, but with Toujeo SoloStar® treatment the decrease was more gradual during the dose adjustment period.
Glycemic control, including improvement in HbAlc, was comparable when Tujeo SoloStar® was administered in the morning or evening, and changing the dosing time within 3 hours before or 3 hours after the patient’s usual dosing time did not affect its effectiveness.
Patients treated with Tujeo SoloStar® experienced an average change in body weight of less than 1 kg by the end of the 6-month treatment period.
Improvement in HbA1c was independent of gender, ethnicity, age, duration of diabetes (<10 vs. ≥10 years), outcome HbAlc (<8 vs. ≥8%), or outcome BMI.
In patients with type 2 diabetes mellitus, the results of clinical studies have demonstrated a lower incidence of severe and/or confirmed hypoglycemia, as well as documented hypoglycemia occurring with clinical symptoms, when treated with Tujeo SoloStar® compared to treatment with insulin glargine 100 U/ml.
The benefit of Tujeo SoloStar over insulin glargine 100 U/mL in reducing the risk of severe and/or documented nocturnal hypoglycemia was demonstrated in patients previously treated with oral hypoglycemic agents (23% risk reduction) or mealtime insulin (21% risk reduction) during the period from week 9 to the end of the study, compared with treatment with insulin glargine 100 U/mL.
In the group of patients treated with Tujeo SoloStar® compared with patients treated with insulin glargine 100 U/ml, a decrease in the risk of hypoglycemia was observed both in patients who had previously received insulin therapy and in patients who had not previously received insulin; The risk reduction was greater during the first 8 weeks of treatment (initial treatment period) and was independent of age, sex, race, BMI, and duration of diabetes mellitus (<10 and ≥10 years).
In patients with type 1 diabetes mellitus, the incidence of hypoglycemia during treatment with Tujeo SoloStar® was similar to that in patients treated with insulin glargine 100 U/ml. However, the incidence of nocturnal hypoglycemia (for all hypoglycemia categories) during the initial treatment period was lower in patients treated with Tujeo SoloStar® compared to patients treated with insulin glargine 100 U/mL.
In clinical studies, a single 24-hour administration of Tujeo SoloStar® in the evening, with a fixed dosing schedule (at the same time) or a flexible dosing schedule (at least 2 times a week, the drug was administered 3 hours before or 3 hours after the usual dosing time, resulting in the intervals between dosing being shortened to 18 hours or extended to 30 hours) had the same effect on HbA1c, plasma glucose concentrations fasting (FPG) and the average value of pre-injection plasma glucose concentration during self-determination. In addition, when using Tujeo SoloStar® with a fixed or flexible dosing schedule, no differences were observed in the incidence of hypoglycemia at any time of the day or nocturnal hypoglycemia. Study results did not indicate any differences related to the formation of insulin antibodies in the efficacy, safety, or dose of basal insulin between patients treated with Tujeo SoloStar® and insulin glargine 100 U/mL (see “Side Effects”). The ORIGIN (Outcome Reduction with Initial Glargine Intervention) trial was an international, multicenter, randomized trial conducted in 12,537 patients with impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or early stage type 2 diabetes mellitus and established cardiovascular disease. Study participants were randomly assigned to receive insulin glargine ≤100 U/mL (n=6264), titrated to FPG <5.3 mmol, or standard care (n=6273). the mean follow-up period was approximately 6.2 years.
The median baseline HbA1c value was 6.4%. Mean HbA1c during treatment ranged from 5.9% to 6.4% in the insulin glargine group and 6.2% to 6.6% in the standard care group throughout follow-up.
The ORIGIN study showed that treatment with insulin glargine 100 U/mL, compared with standard hypoglycemic therapy, did not change the risk of cardiovascular events (cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke), the risk of undergoing a revascularization procedure (coronary, carotid, or peripheral arteries) or hospitalization for heart failure, or the risk of microvascular complications (a composite indicator of microvascular complications: laser photocoagulation or vitrectomy, vision loss due to diabetic retinopathy, progression of albuminuria or doubling of blood creatinine concentration, or the need for dialysis therapy).
In a study evaluating the effect of insulin glargine 100 U/ml on the development of diabetic retinopathy during a five-year follow-up of patients with type 2 diabetes, there were no significant differences in the progression of diabetic retinopathy when treated with insulin glargine 100 U/ml compared with isophane insulin.
Special patient groups
Gender and race. There were no differences in the effectiveness and safety of Tujeo SoloStar® and insulin glargine 100 U/ml depending on the gender and race of patients.
Old age. In controlled clinical trials, 716 patients (23% of the safety population) with type 1 and type 2 diabetes mellitus were ≥65 years of age and 97 patients (3%) were ≥75 years of age. Overall, there were no differences in efficacy and safety between these patients and younger patients. In elderly patients with diabetes mellitus, to avoid hypoglycemic reactions, the initial and maintenance dose should be lower, and dose increases should be carried out more slowly. Elderly patients may have difficulty recognizing hypoglycemia. Careful monitoring of blood glucose concentrations is recommended, and the dose of insulin should be adjusted individually (see “Dosage and Administration” and “Pharmacokinetics”).
Kidney failure. In controlled clinical trials, a subgroup analysis based on renal function (defined as outcome GFR <60 or ≥60 mL/min/1.73 m2 body surface area) showed no differences in safety and efficacy between Toujeo SoloStar® and insulin glargine 100 U/mL. Careful monitoring of blood glucose concentrations is recommended, and the dose of insulin should be adjusted individually (see "Dosage and Administration" and "Pharmacokinetics").
Obese patients. In clinical studies, subgroup analysis based on BMI (up to 63 kg/m2) showed no differences in efficacy and safety between Tujeo SoloStar® and insulin glargine 100 U/ml.
Children. There are no data on the use of Tujeo SoloStar® in children.
Pharmacokinetics
Absorption and distribution. Following subcutaneous injection of Toujeo SoloStar® in healthy volunteers and diabetic patients, serum insulin concentrations indicate a much slower and more prolonged absorption, resulting in a flatter AUC curve for up to 36 hours compared to insulin glargine 100 U/mL. The AUC curve of Toujeo SoloStar® corresponded to the curve of its pharmacodynamic activity. Css within the therapeutic concentration range was achieved after 3–4 days of daily use of Tujeo SoloStar®.
After subcutaneous injection of Toujeo SoloStar®, inter-patient variability, defined as the coefficient of variation in systemic insulin exposure over 24 hours at Css, was low (17.4%).
Metabolism. In humans, after subcutaneous administration of the drug Tujeo SoloStar®, insulin glargine is rapidly metabolized from the carboxyl end (C-terminus) of the β-chain with the formation of two active metabolites M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin). The M1 metabolite circulates predominantly in the blood plasma. Systemic exposure of the M1 metabolite increases with increasing doses of Tujeo SoloStar®. A comparison of pharmacokinetics and pharmacodynamics data showed that the effect of the drug is mainly due to the systemic exposure of the M1 metabolite. In the vast majority of patients, insulin glargine and the M2 metabolite could not be detected in the systemic circulation. In cases where it was nevertheless possible to detect insulin glargine and the M2 metabolite in the blood, their concentrations did not depend on the administered dose and dosage form of insulin glargine.
Excretion. T1/2 of metabolite M1, the quantitatively predominant metabolite of the drug Tujeo SoloStar®, after subcutaneous injection of the drug is 18–19 hours, regardless of the dose.
Special patient groups
Gender and race. There is no information on the influence of race and gender on the pharmacokinetics of insulin glargine (see Pharmacodynamics).
Old age. The effect of age on the pharmacokinetics of Tujeo SoloStar® has not yet been studied. In elderly patients with diabetes mellitus, in order to avoid hypoglycemic reactions, the initial dose and maintenance dose should be lower, and dose increases should be carried out more slowly (see “Pharmacodynamics” and “Dosage and Administration”).
Children. In children, the pharmacokinetics of Tujeo SoloStar® have not yet been studied.
Kidney and liver failure. The effect of renal and hepatic failure on the pharmacokinetics of Tujeo SoloStar® has not yet been studied. However, some studies conducted with human insulin have shown increased insulin concentrations in patients with renal and hepatic impairment. Careful monitoring of blood glucose concentrations and individual adjustment of the insulin dose is recommended (see “Dosage and Administration” and “Pharmacodynamics”).
Special instructions
Special instructions
Patients must have skills in self-control of diabetes mellitus, including monitoring blood glucose concentrations, as well as adhere to the correct technique for performing subcutaneous injections and be able to stop the development of hypoglycemia and hyperglycemia. Insulin therapy requires constant vigilance regarding the possibility of developing hyperglycemia or hypoglycemia.
In case of insufficient control of the concentration of glucose in the blood, as well as in the presence of a tendency to develop hypo- or hyperglycemia, before proceeding with the correction of the dosage regimen, you should check the accuracy of the prescribed treatment regimen, compliance with the instructions regarding the drug administration sites, the correct technique for performing subcutaneous injections and handling the SoloStar® syringe pen, and also take into account the possibility of all other factors that can cause such a condition.
Hypoglycemia
The time for the development of hypoglycemia depends on the action profile of the insulins used and may thus change with changes in the treatment regimen. Particular caution should be exercised and intensified monitoring of blood glucose concentrations when using the drug in patients in whom episodes of hypoglycemia may be of particular clinical significance, such as patients with severe stenosis of the coronary arteries or cerebral vessels (risk of developing cardiac and cerebral complications of hypoglycemia), as well as patients with proliferative retinopathy, especially if they are not receiving photocoagulation treatment (risk of transient loss of vision following hypoglycemia). As with any insulin, in some conditions the warning signs of hypoglycemia may change, become less pronounced, or be absent.
These include:
– noticeable improvement in glycemic control;
– gradual development of hypoglycemia;
– old age;
– presence of autonomic neuropathy;
– long history of diabetes mellitus;
– presence of mental disorders;
– simultaneous use of insulin glargine with some other drugs (see “Interaction”).
Such situations may result in severe hypoglycemia (with possible loss of consciousness) before the patient is aware that he is developing hypoglycemia.
It should be taken into account that the prolonged action of the drug Tujeo SoloStar® when administered subcutaneously may delay the patient’s recovery from the hypoglycemia state.
If normal or reduced levels of glycosylated Hb are observed, it is necessary to consider the possibility of developing repeated unrecognized episodes of hypoglycemia (especially at night).
Patients’ compliance with the dosage regimen and diet, correct administration of insulin and knowledge of the warning signs of hypoglycemia help to significantly reduce the risk of developing hypoglycemia.
Factors that increase the tendency to hypoglycemia, the presence of which require particularly careful monitoring and may require adjustment of the insulin dose:
– changing the site of insulin administration;
– increasing sensitivity to insulin (for example, when eliminating stress factors);
– unusual, increased or prolonged physical activity;
– intercurrent diseases accompanied by vomiting, diarrhea;
– insufficient food intake;
– ethanol consumption;
– some uncompensated endocrine disorders (such as hypothyroidism, anterior pituitary insufficiency or adrenal insufficiency);
– simultaneous use of insulin glargine with some other drugs (see “Interaction”).
In patients with renal failure, insulin requirements may be reduced by slowing insulin metabolism (see Pharmacodynamics, Pharmacokinetics, and Dosage and Administration). In elderly patients, progressive deterioration of renal function may lead to a sustained decrease in insulin requirements (see Pharmacodynamics, Pharmacokinetics, and Dosage and Administration).
In patients with severe hepatic impairment, insulin requirements may be reduced due to decreased gluconeogenic capacity and decreased insulin metabolism (see Pharmacodynamics, Pharmacokinetics, and Dosage and Administration).
Hypoglycemia can generally be reversed by immediate intake of rapidly digestible carbohydrates. Because initial steps to correct hypoglycemia must be immediate, patients should always carry at least 20 g of rapidly digestible carbohydrates with them.
Intercurrent diseases
Intercurrent illnesses require more intensive control of blood glucose concentrations. In many cases, an analysis for the presence of ketone bodies in the urine is indicated, and adjustment of the insulin dosage regimen is also often required. When intercurrent illness occurs, insulin requirements often increase. Patients with type 1 diabetes should continue to consume carbohydrates on a regular basis, even if they are able to eat only small meals or not at all or if they develop vomiting; Patients with type 1 diabetes should never skip insulin completely.
Combination of insulin glargine with pioglitazone
Cases of heart failure have been reported when pioglitazone is used in combination with insulin, especially in patients at risk of developing heart failure. This information should be taken into account when considering the use of the combination of pioglitazone with Toujeo SoloStar®. When using this combination, patients should be monitored for signs and symptoms of heart failure, such as weight gain and edema. If cardiac symptoms appear or worsen, use of pioglitazone should be discontinued.
Preventing errors when administering insulin medications
In order not to confuse Tujeo SoloStar® with other insulins, you should always check the markings on the syringe pen before each injection. Cases have been reported in which other insulins, particularly short-acting insulins, were accidentally administered instead of long-acting insulins.
To avoid dosing errors and possible overdose, patients should never use a syringe to remove Toujeo® from a SoloStar® pen (see Dosage and Administration, Overdose).
As with other insulin pens, patients should visually check the number of dose units drawn in the dose indicator window on the pen. Patients who are blind or have low vision should receive assistance from others with good vision and who are able to use the Tujeo SoloStar® Syringe Pen.
Recommendations for storing the Tujeo SoloStar® syringe pen
When storing Tujeo SoloStar® in the refrigerator (unopened/prior to use), you must ensure that the packages of syringe pens do not come into direct contact with the freezer compartment or frozen foods, because the drug should not be frozen. If insulin has been frozen, it cannot be used and the pen should be discarded.
Used SoloStar® syringe pens should be stored at a temperature not exceeding 30 °C, protected from exposure to light and heat.
Impact on the ability to drive vehicles and engage in other potentially hazardous activities. Patients’ ability to concentrate and speed of psychomotor reactions may be impaired, for example as a result of the development of hypoglycemia or hyperglycemia, as well as as a result of visual impairment. This may pose a risk in situations where these abilities are particularly important (for example, driving a car or operating machinery). Patients are advised to take precautions to avoid the development of hypoglycemia while driving. This is especially important for those who have mild or no symptoms that are warning signs of developing hypoglycemia, or for patients with frequent episodes of hypoglycemia. These characteristics of the patient should be taken into account when deciding whether he can drive vehicles.
Active ingredient
Active ingredient
Insulin glargine
Composition
Composition
1 ml of solution contains:
active substance:
insulin glargine 300 units (10.91 mg);
excipients:
metacresol (m-cresol) – 2.70 mg,
zinc chloride – 0.19 mg (corresponds to 0.09 mg zinc),
glycerol (85%) – 20 mg,
sodium hydroxide – up to pH 4.0,
hydrochloric acid – up to pH 4.0,
water for injection – up to 1.0 ml.
Contraindications
Contraindications
hypersensitivity to insulin glargine or any of the excipients of the drug;
age under 18 years (due to the lack of clinical data confirming the effectiveness and safety of the drug in children and adolescents).
With caution: pregnant women (the possibility of changes in insulin requirements during pregnancy and after childbirth), elderly patients (see “Pharmacokinetics”, “Pharmacodynamics”, “Dosage and Administration” and “Special Instructions”); patients with uncompensated endocrine disorders (such as hypothyroidism, insufficiency of the adenohypophysis and adrenal cortex); diseases accompanied by vomiting or diarrhea; severe stenosis of the coronary arteries or cerebral vessels; proliferative retinopathy (especially if patients have not undergone photocoagulation); renal failure; severe liver failure (see “Special Instructions”).
Side Effects
Side Effects
The following adverse reactions (ARs) were observed during clinical studies conducted with Tujeo SoloStar® and during clinical use of insulin glargine 100 U/ml. These ADRs are presented by organ system (in accordance with the MedDRA classification in accordance with the following gradations of the frequency of their occurrence recommended by WHO: very common (≥10%); common (≥1; <10%); infrequently (≥0.1; <1%); rare (≥0.01; <0.1%); very rare (<0.01%), frequency unknown (determine the incidence of ADRs by not possible based on the available data).
Metabolism and nutrition: hypoglycemia. Hypoglycemia, the most common adverse reaction of insulin therapy, can occur when the dose of insulin is too high compared to the need. As with other insulins, episodes of severe hypoglycemia, especially repeated episodes, can lead to neurological impairment.
Episodes of prolonged and severe hypoglycemia can be life-threatening for patients.
In many patients, signs and symptoms of neuroglycopenia (feeling tired, inappropriate fatigue or weakness, decreased ability to concentrate, drowsiness, visual disturbances, headache, nausea, confusion or loss of consciousness, seizures) are preceded by signs of adrenergic counterregulation (activation of the sympathetic-adrenal system in response to hypoglycemia) – hunger, irritability, nervous agitation or tremor, anxiety, pale skin, cold sweat, tachycardia, palpitations. Typically, the faster hypoglycemia develops and the more severe it is, the more severe the symptoms of adrenergic counterregulation are.
On the part of the organ of vision: a significant improvement in glycemic control may cause a temporary deterioration in vision due to a temporary disturbance in the turgor and refractive index of the lens of the eye.
Long-term improvement in glycemic control reduces the risk of progression of diabetic retinopathy. However, as with any insulin regimen, intensification of insulin therapy with a sharp improvement in glycemic control may be associated with a temporary worsening of diabetic retinopathy.
In patients with proliferative retinopathy, especially those not receiving photocoagulation treatment, episodes of severe hypoglycemia may lead to transient vision loss.
From the skin and subcutaneous tissues: as with treatment with any other insulin preparations, lipodystrophy may develop at the injection site, which can slow down the local absorption of insulin. With insulin regimens containing insulin glargine, lipodystrophy was observed in 1–2% of patients, and lipoatrophy was observed infrequently. Constantly changing injection sites within areas of the body recommended for subcutaneous insulin administration may help reduce the severity of this reaction or prevent its development.
From the musculoskeletal and connective tissue side: very rarely – myalgia.
General disorders and disorders at the injection site: local allergic reactions at the injection site. As with all insulin therapy, such reactions include skin redness, pain, itching, hives, rash, swelling and inflammation. In clinical studies conducted in adult patients, the incidence of all injection site reactions in patients treated with Tujeo SoloStar® (2.5%) was similar to that in patients treated with insulin glargine 100 U/mL (2.8%). Most minor insulin injection site reactions usually resolve within a few days to a few weeks.
From the immune system: systemic allergic reactions. Immediate allergic reactions to insulin are rare. Such reactions to insulin (including insulin glargine) or excipients may, for example, be accompanied by generalized skin reactions, angioedema (Quincke’s edema), bronchospasm, decreased blood pressure and shock and pose a threat to the patient’s life.
Other reactions: the use of insulin may cause the formation of antibodies to it. In clinical studies comparing Tujeo SoloStar® and insulin glargine 100 U/ml, the formation of antibodies to insulin in both treatment groups was observed with the same frequency. As with other insulins, in rare cases, the presence of such insulin antibodies may require changes in the insulin dose to eliminate the tendency to develop hypoglycemia or hyperglycemia.
In rare cases, insulin may cause sodium retention and edema, especially when previously poor metabolic control is improved by intensifying insulin therapy.
Children. The safety profile for children and adolescents under 18 years of age has not yet been established.
Interaction
Interaction
A number of drugs affect glucose metabolism, as a result of which, when used simultaneously with insulins, adjustment of the insulin dose and especially careful monitoring may be required.
Medicines that can increase the hypoglycemic effect of insulin and the tendency to develop hypoglycemia. Oral hypoglycemic agents, ACE inhibitors, salicylates, disopyramide; fibrates, fluoxetine, MAO inhibitors, pentoxifylline, propoxyphene, sulfonamide antibiotics. Concomitant use of these drugs with insulin glargine may require adjustment of the insulin dose.
Medicines that can weaken the hypoglycemic effect of insulin. GCS, danazol, diazoxide, diuretics, sympathomimetics (such as adrenaline, salbutamol, terbutaline); glucagon, isoniazid, phenothiazine derivatives, growth hormone, thyroid hormones, estrogens and gestagens (for example, in hormonal contraceptives), protease inhibitors and atypical antipsychotics (for example, olanzapine and clozapine). Concomitant use of these drugs with insulin glargine may require adjustment of the insulin dose.
Beta-blockers, clonidine, lithium salts and ethanol – it is possible to either enhance or weaken the hypoglycemic effect of insulin.
Pentamidine, when combined with insulin, can cause hypoglycemia, which sometimes gives way to hyperglycemia.
Sympatholytic drugs – under the influence of sympatholytic drugs, such as beta-blockers, clonidine, guanethidine and reserpine, signs of adrenergic counterregulation (activation of the sympathetic nervous system in response to the development of hypoglycemia) may decrease or be absent.
Interaction with pioglitazone. When pioglitazone is used in combination with insulin, cases of heart failure have been reported, especially in patients at risk of developing heart failure (see “Special Instructions”). If cardiac symptoms appear or worsen, use of pioglitazone should be discontinued.
Overdose
Overdose
Symptoms: Insulin overdose (excess insulin relative to food intake, energy expenditure, or both) can lead to severe and sometimes long-term and life-threatening hypoglycemia in the patient.
Treatment: Episodes of moderate hypoglycemia are usually controlled by ingestion of rapidly digestible carbohydrates. It may be necessary to change the drug dosage regimen, diet, or physical activity.
Episodes of more severe hypoglycemia, manifested by coma, seizures or neurological disorders, can be treated with intramuscular or subcutaneous administration of glucagon or intravenous administration of a concentrated solution of dextrose (glucose). Long-term intake of carbohydrates and specialist supervision may be required, because After visible clinical improvement, relapse of hypoglycemia is possible.
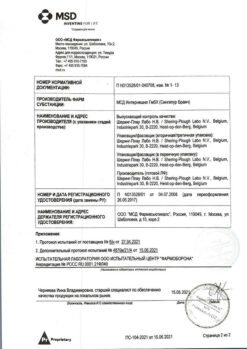
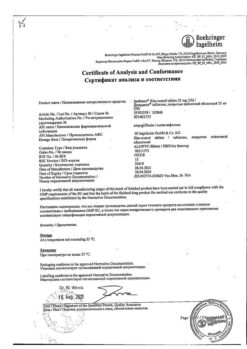
Manufacturer
Manufacturer
Sanofi-Vostok JSC, Russia
Additional information
| Manufacturer | Sanofi-Vostok JSC, Russia |
|---|---|
| Medication form | solution |
| Brand | Sanofi-Vostok JSC |
Other forms…
Related products
Buy Tugeo SoloStar, 300 units/ml 1.5 ml cartridges in SoloStar syringe pens 3 pcs with delivery to USA, UK, Europe and over 120 other countries.