No products in the cart.
Trilactan, eye drops 0.005% 2.5ml 3 pcs.
€36.27 €31.44
Description
Pharmacotherapeutic group
Antiglaucoma drug – prostaglandin F2α analogue synthetic
ATX code
S01EE
Pharmacodynamics:
Latanoprost, a prostaglandin F2α analog, is a selective FP (prostaglandin F) receptor agonist and reduces intraocular pressure (IOP) by increasing aqueous humor outflow primarily by the uveoscleral route as well as through the trabecular meshwork. IOP lowering starts approximately 3-4 hours after the drug is injected; the maximum effect is observed after 8-12 hours and the action lasts for at least 24 hours.
Latanoprost has been found to have no significant effect on aqueous humor production and the blood-ophthalmic barrier.
Latanoprost has no significant pharmacological effect on the cardiovascular and respiratory systems when used in therapeutic doses. Pharmacokinetics:
Latanoprost (molecular weight 43258) is a prodrug esterified with isopropyl group is inactive; after hydrolysis to acidic form it becomes biologically active.
Intake
The prodrug is well absorbed through the cornea and is fully hydrolyzed when exposed to aqueous moisture.
Distribution
Studies in humans have shown that the maximum concentration in aqueous humor is reached 2 hours after instillation. After instillation in monkeys, latanoprost is predominantly distributed in the anterior chamber of the eye, the conjunctiva and the eyelids. Only a small amount of latanoprost reaches the posterior chamber of the eye.
Biotransformation
The active form of latanoprost is virtually unmetabolized in the eye but is biotransformed in the liver.
Elimation
The plasma elimination half-life is 17 minutes.
The animal studies have shown that the major metabolites (12-dinor- and 1234-tetranormetabolites) have no (or low) biological activity and are excreted mainly in the urine.
Children
Exposure to latanoprost is approximately 2 times higher in children aged 3 to 12 years compared to adult patients and 6 times higher in children younger than 3 years.
However, the safety profile of the drug does not differ between children and adults. The time to reach the maximum plasma concentration of latanoprost acid is 5 minutes for all age groups. The elimination half-life of latanoprost acid in children is the same as in adults. At equilibrium concentration there is no plasma cumulation of latanoprost acid.
Indications
Indications
Reduction of elevated intraocular pressure in adults and children (over 1 year of age) with open-angle glaucoma or increased ophthalmotonus.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Antiglaucoma agent – prostaglandin F2α analogue synthetic
ATX code
S01EE
Pharmacodynamics:
Latanoprost, a prostaglandin F2α analogue, is a selective FP (prostaglandin F) receptor agonist and reduces intraocular pressure (IOP) by increasing the outflow of aqueous humor mainly through the uveoscleral pathway and also through the trabecular meshwork. The decrease in IOP begins approximately 3-4 hours after administration of the drug; the maximum effect is observed after 8-12 hours; the effect persists for at least 24 hours.
It has been established that latanoprost does not have a significant effect on the production of aqueous humor and the blood-ophthalmic barrier.
When used in therapeutic doses, latanoprost does not have a significant pharmacological effect on the cardiovascular and respiratory systems.
Pharmacokinetics:
Latanoprost (molecular weight 43258) is a prodrug esterified with an isopropyl group and is inactive; after hydrolysis to the acid form it becomes biologically active.
Suction
The prodrug is well absorbed through the cornea and is completely hydrolyzed when it enters the aqueous humor.
Distribution
Studies in humans have shown that the maximum concentration in aqueous humor is achieved 2 hours after instillation. After instillation in monkeys, latanoprost is distributed predominantly in the anterior chamber of the eye, conjunctiva and eyelids. Only a small amount of latanoprost reaches the posterior chamber of the eye.
Biotransformation
The active form of latanoprost is practically not metabolized in the eye, but undergoes biotransformation in the liver.
Removal
The plasma half-life is 17 minutes.
Animal studies have shown that the main metabolites (12-dinor- and 1234-tetrano-normetabolites) have no (or low) biological activity and are excreted primarily in the urine.
Children
Exposure to latanoprost is approximately 2 times higher in children aged 3 to 12 years compared to adult patients and 6 times higher in children under 3 years of age.
However, the safety profile of the drug does not differ between children and adults. The time to reach the maximum concentration of latanoprost acid in the blood plasma is 5 minutes for all age groups. The half-life of latanoprost acid in children is the same as in adults. At equilibrium concentration, latanoprost acid does not camulate in the blood plasma.
Special instructions
Special instructions
Latanoprost can gradually change eye color by increasing the amount of brown pigment in the iris. Before starting treatment, patients should be informed about the possible permanent change in eye color. Using the drug in one eye may cause irreversible heterochromia. This change in eye color was predominantly observed in patients with unevenly colored irises, namely: brown-blue gray-brown yellow-brown and green-brown. In studies of latanoprost, darkening usually began within the first 8 months of treatment, rarely during the second and third years, and was not observed after four years of treatment.
The progression of iris pigmentation decreased over time and stabilized after 5 years. There is no data on increased pigmentation over 5 years. In an open-label, 5-year safety study of latanoprost, 33% of patients developed iris pigmentation (see section “Side Effects”). In most cases, the change in iris color was minor and often not clinically detected. The incidence ranged from 7 to 85% in patients with unequal-colored irises, predominant in patients with yellow-brown irises. No changes were observed in patients with uniformly colored blue irises; in rare cases, changes were observed in uniformly colored gray green and brown irises.
The change in eye color is caused by an increase in the melanin content in the stromal melanocytes of the iris and not by an increase in the number of melanocytes themselves. In typical cases, brown pigmentation appears around the pupil and extends concentrically to the periphery of the iris. In this case, the entire iris or parts of it acquire a brown color. After discontinuation of therapy, no further pigmentation was observed. According to available clinical data, the color change was not associated with any symptoms or pathological disorders.
The drug has no effect on nevi and lentigines of the iris. According to the results of 5-year clinical studies, pigment accumulation in the sclerocorneal trabecular meshwork or other parts of the anterior chamber of the eye was not noted. It has been shown that darkening of the iris does not lead to undesirable clinical consequences, so the use of latanoprost when such darkening occurs can be continued. However, such patients should be monitored regularly and treatment may be discontinued depending on the clinical situation.
Experience with the use of latanoprost in the treatment of angle-closure and congenital glaucoma, pigmentary glaucoma, and open-angle glaucoma in patients with pseudophakia is limited.
There is no information on the use of latanoprost in the treatment of secondary glaucoma due to inflammatory eye diseases and neovascular glaucoma.
Latanoprost has no effect on pupil size.
Due to the fact that information on the use of latanoprost in the postoperative period of cataract extraction is limited, caution should be exercised when using the drug in this category of patients.
Caution should be exercised when using latanoprost in patients with a history of herpetic keratitis. In case of acute herpetic keratitis, as well as in the case of anamnestic information about chronic recurrent herpetic keratitis, it is necessary to avoid prescribing latanoprost.
Macular edema, including cystic edema, was observed during latanoprost therapy, mainly in patients with aphakia and pseudophakia. rupture of the posterior capsule of the lens or in patients with risk factors for the development of cystoid macular edema (in particular, diabetic retinopathy and retinal vein occlusion). Caution should be exercised when using latanoprost in aphakic pseudophakic patients with posterior capsule rupture or anterior chamber intraocular lenses, as well as in patients with known risk factors for cystoid macular edema.
Caution should be exercised when using latanoprost in patients with risk factors for developing iritis/uveitis.
Experience with the use of latanoprost in patients with bronchial asthma is limited, but in a number of cases, in the post-registration period, exacerbation of asthma and/or the appearance of shortness of breath was noted. Caution should be exercised when using latanoprost in this category of patients (see also section “Side effects”). There have been cases of darkening of the skin of the periorbital area, which in some patients was reversible with continued therapy with latanoprost.
Latanoprost can cause gradual changes in eyelashes and vellus hair such as lengthening, thickening, increasing pigmentation, increasing thickness and changing the direction of eyelash growth. Changes in eyelashes were reversible and disappeared after cessation of therapy.
Trilactan® contains benzalkonium chloride, often used as a preservative in ophthalmic medicinal products. Benzalkonium chloride may cause eye irritation, punctate keratopathy and/or toxic ulcerative keratopathy, and may be absorbed and discolored by soft contact lenses. Careful monitoring of the condition of patients with dry eye syndrome or other corneal diseases is required during long-term use of latanoprost. Before using the drug, you must remove contact lenses and reinsert them no earlier than 15 minutes after instillation (see also section “Method of administration and dosage”).
Children
Information on the effectiveness and safety of latanoprost in children under one year of age is limited. There is no experience with the use of the drug in premature infants (gestational age less than 36 weeks).
There is no information on the safety of long-term use of latanoprost in children. For primary congenital glaucoma in children aged 0 to 3 years, surgical intervention (goniotomy/trabeculotomy) remains the standard treatment.
Impact on the ability to drive vehicles. Wed and fur.:
As with the use of other ophthalmic drugs, temporary visual impairment is possible; It is not recommended to drive vehicles or operate machinery until it is restored.
Active ingredient
Active ingredient
Latanoprost
Composition
Composition
1 ml of the drug contains:
Active ingredient:
Latanoprost 0.05 mg
Excipients:
Benzalkonium chloride 0.20 mg
Sodium chloride 4.10 mg
Sodium dihydrogen phosphate monohydrate 4.60 mg
Sodium hydrogen phosphate anhydrous 4.74 mg
Water for injections up to 1 ml.
Pregnancy
Pregnancy
Pregnancy
The safety of latanoprost during pregnancy in humans has not been established. Latanoprost may have toxic effects on the fetus and newborn during pregnancy. Use during pregnancy is contraindicated.
Breastfeeding period
Latanoprost and its metabolites can pass into breast milk. Use during breastfeeding is contraindicated. If it is necessary to use the drug, breastfeeding should be stopped.
Fertility
No effect of latanoprost on male or female fertility was found in animal studies.
Contraindications
Contraindications
Hypersensitivity to latanoprost or other components of the drug. Age up to 1 year (efficacy and safety have not been established).
With caution:
Aphakia pseudophakia with rupture of the posterior capsule of the lens; patients with risk factors for macular edema (cases of development of macular edema, including cystoid, have been described during treatment with latanoprost); inflammatory neovascular glaucoma (due to lack of sufficient experience in using the drug); bronchial asthma; history of herpetic keratitis.
The use of the drug should be avoided in patients with active herpetic keratitis and recurrent herpetic keratitis, especially associated with the use of prostaglandin F2α analogues. The drug should be used with caution in patients with risk factors for developing iritis/uveitis. There is limited data on the use of the drug in patients undergoing cataract surgery. In this regard, the drug should be used with caution in this group of patients.
Side Effects
Side Effects
Most of the adverse reactions were observed in the organ of vision. In an open-label 5-year safety study, 33% developed iris pigmentation (see Precautions section). Other undesirable reactions from the organ of vision are usually transient and are noted immediately after instillation. The gradation of adverse reactions according to frequency of occurrence was carried out as follows: very often (≥1/10); often (≥1/100 <1/10); uncommon (≥1/1000 <1/100); rare (≥1/10,000 <1/1000); very rare (<1/10,000); frequency unknown (frequency cannot be estimated based on available data).
Infections and infestations
Frequency unknown: herpetic keratitis.
From the side of the organ of vision
Very common: hyperpigmentation of the iris, hyperemia of the conjunctiva, mild to moderate eye irritation (burning sensation, feeling of sand in the eyes, itching, tingling and foreign body sensation) changes in eyelashes (increase in length, thickness, number and pigmentation).
Common: transient punctate erosions of the epithelium (mostly asymptomatic) blepharitis pain in the eye.
Uncommon: swelling of the eyelids, dry mucous membrane of the eye, keratitis, blurred vision, conjunctivitis.
Rarely: iritis/uveitis (mainly in predisposed patients) macular edema eyelid edema corneal edema corneal erosion periorbital edema darkening of the eyelid skin reactions of the eyelid skin changes in the direction of eyelash growth thickening darkening and lengthening of eyelashes distichiasis photophobia.
Very rare: changes in the periorbital area and in the eyelash area leading to a deepening of the furrow of the upper eyelid.
Frequency unknown: conjunctival pseudopemphigoid iris cyst.
From the nervous system
Frequency unknown: dizziness, headache.
From the side of the heart
Uncommon: angina pectoris, palpitations.
Frequency unknown: unstable angina.
From the respiratory system
Rarely: bronchospasm (including exacerbation of the disease in patients with a history of bronchial asthma), shortness of breath.
From the skin and subcutaneous tissues
Uncommon: rash.
Rarely: skin itching.
Very rare: darkening of the skin of the eyelids and local skin reactions on the eyelids.
From the musculoskeletal system and connective tissue
Frequency unknown: myalgia, arthralgia.
General disorders and local reactions
Very rare: chest pain.
Interaction
Interaction
When two prostaglandin analogs are instilled into the eyes simultaneously, a paradoxical increase in IOP has been described; therefore, the simultaneous use of two or more prostaglandin analogs or derivatives is not recommended.
Pharmaceutically incompatible with eye drops containing thiomersal – precipitation.
Overdose
Overdose
In addition to irritation of the mucous membrane of the eyes, hyperemia of the conjunctiva or episclera, other undesirable changes in the organ of vision are not known with an overdose of latanoprost.
In case of accidental ingestion of latanoprost, the following information should be taken into account: one bottle of 25 ml of solution contains 125 mcg of latanoprost. More than 90% of the drug is metabolized during the first passage through the liver. Intravenous infusion at a dose of 3 mcg/kg in healthy volunteers did not cause any symptoms; however, when a dose of 55-10 mcg/kg was administered, nausea, abdominal pain, dizziness, fatigue, hot flashes and sweating were observed. In patients with moderate bronchial asthma, administration of latanoprost into the eyes at a dose 7 times higher than the therapeutic dose did not cause bronchospasm.
In case of overdose, symptomatic treatment is carried out.
Storage conditions
Storage conditions
At temperatures from 2 to 8 °C.
Store the opened bottle at a temperature not exceeding 25 °C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
After opening the bottle – 1 month.
Do not use after the expiration date!
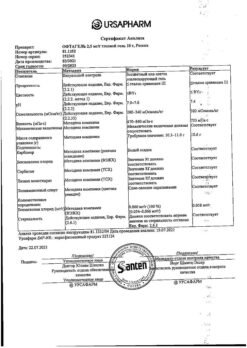
Manufacturer
Manufacturer
Grotex LLC, Russia
Additional information
| Shelf life | 3 years. 1 month after opening the bottle. Do not use after the expiration date! |
|---|---|
| Conditions of storage | At a temperature of 2 to 8 ° C. Store opened bottle at a temperature not exceeding 25 °С. Store out of reach of children. |
| Manufacturer | Grotex Ltd, Russia |
| Medication form | eye drops |
| Brand | Grotex Ltd |
Other forms…
Related products
Buy Trilactan, eye drops 0.005% 2.5ml 3 pcs. with delivery to USA, UK, Europe and over 120 other countries.