No products in the cart.
Torvacard, 20 mg 30 pcs
€10.92 €9.10
Description
Hypolipidemic drug from the group of statins. Selective competitive inhibitor of HMG-CoA reductase – enzyme converting 3-hydroxy-3-methylglutaryl coenzyme A into mevalonic acid, which is a precursor of sterols, including cholesterol (CH). Triglycerides (TG) and CH in the liver are incorporated into LDL, enter the blood plasma, and are transported to peripheral tissues. LDL are formed from LDL in the course of interaction with LDL receptors.
Atorvastatin reduces plasma concentrations of CH and lipoproteins due to inhibition of HMG-CoA reductase, synthesis of CH in liver and increase in number of hepatic LDL receptors on cell surface that leads to increase of capture and catabolism of LDL. Reduces LDL formation, causes a pronounced and persistent increase in LDL receptor activity. Reduces LDL concentration in patients with homozygous familial hypercholesterolemia, which usually does not respond to therapy with hypolipidemic agents. Reduces the concentration of total cholesterol by 30-46%, LDL by 41-61%, apolipoprotein B by 34-50% and TG by 14-33%; causes an increase in concentration of HDL-C and apolipoprotein A.
Dose-dependently reduces LDL concentration in patients with homozygous hereditary hypercholesterolemia resistant to therapy with other hypolipidemic agents.
Pharmacokinetics
The absorption is high. Cmax in plasma is reached after 1-2 h, Cmax is 20% higher in women, AUC is 10% lower; Cmax in patients with alcoholic liver cirrhosis is 16 times higher than normal, AUC is 11 times higher.
Food slightly reduces rate and duration of drug absorption (by 25% and 9%, respectively), but decrease of LDL-C is similar to that with atorvastatin without food. Concentration of atorvastatin when administered in the evening is lower than in the morning (approximately by 30%). A linear relationship between the degree of absorption and the drug dose was found.
Bioavailability is 12%, systemic bioavailability of HMG-CoA reductase inhibitory activity is 30%. Low systemic bioavailability is due to presystemic metabolism in the gastrointestinal mucosa and during first passage through the liver.
The average Vd is 381 l, the binding to plasma proteins is 98%. It is metabolized mainly in liver under the action of CYP3A4, CYP3A5 and CYP3A7 isoenzymes with formation of pharmacological active metabolites (ortho- and parahydroxylated derivatives, β-oxidation products). In vitro, ortho- and parahydroxylated metabolites have an inhibitory effect on HMG-CoA reductase that is comparable to that of atorvastatin. The inhibitory effect of the drug against HMG-CoA reductase is approximately 70% determined by the activity of circulating metabolites.
Extracted through the intestine with bile after hepatic and/or extrahepatic metabolism (not subject to marked intestinal-hepatic recirculation).
T1/2 – 14 h. Inhibitory activity against HMG-CoA reductase persists for about 20-30 h due to the presence of active metabolites. Less than 2% of the oral dose is detected in the urine. It is not excreted during hemodialysis.
Indications
Indications
diseases of the cardiovascular system (in patients with increased risk factors for ischemic heart disease – old age over 55 years, smoking, arterial hypertension, diabetes mellitus, peripheral vascular disease, previous stroke, left ventricular hypertrophy, protein/albuminuria, ischemic heart disease in close relatives), incl. against the background of dyslipidemia, – secondary prevention to reduce the total risk of death, myocardial infarction, stroke, re-hospitalization for angina pectoris and the need for a revascularization procedure;
in combination with diet to reduce elevated levels of total cholesterol, cholesterol/LDL, apolipoprotein B and TG and increased levels of cholesterol/HDL in patients with primary hypercholesterolemia, heterozygous familial and non-familial hypercholesterolemia and combined (mixed) hyperlipidemia (Fredrickson types IIa and IIb);
in combination with a diet for the treatment of patients with elevated serum TG levels (Fredrickson type IV) and patients with dysbetalipoproteinemia (Fredrickson type III) in whom diet therapy does not provide an adequate effect;
to reduce the levels of total cholesterol and cholesterol/LDL in patients with homozygous familial hypercholesterolemia, when diet therapy and other non-pharmacological treatments are not effective enough (as an addition to lipid-lowering therapy, including autohemotransfusion of LDL-free blood).
Pharmacological effect
Pharmacological effect
A lipid-lowering drug from the group of statins. A selective competitive inhibitor of HMG-CoA reductase, an enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A into mevalonic acid, which is a precursor of sterols, including cholesterol (CH). Triglycerides (TG) and cholesterol in the liver are included in VLDL, enter the blood plasma and are transported to peripheral tissues. LDL is formed from VLDL through interaction with LDL receptors.
Atorvastatin reduces the concentration of cholesterol and lipoproteins in the blood plasma by inhibiting HMG-CoA reductase, cholesterol synthesis in the liver and increasing the number of hepatic LDL receptors on the cell surface, which leads to increased uptake and catabolism of LDL. Reduces the formation of LDL, causes a pronounced and persistent increase in the activity of LDL receptors. Reduces the concentration of LDL in patients with homozygous familial hypercholesterolemia, which usually does not respond to treatment with lipid-lowering drugs. Reduces the concentration of total cholesterol by 30–46%, LDL by 41–61%, apolipoprotein B by 34–50% and TG by 14–33%; causes an increase in the concentration of HDL cholesterol and apolipoprotein A.
Dose-dependently reduces the concentration of LDL in patients with homozygous hereditary hypercholesterolemia, resistant to therapy with other lipid-lowering drugs.
Pharmacokinetics
Absorption is high. Cmax in blood plasma is achieved after 1–2 hours, Cmax in women is 20% higher, AUC is 10% lower; Cmax in patients with alcoholic cirrhosis is 16 times, AUC is 11 times higher than normal.
Food slightly reduces the rate and duration of drug absorption (by 25 and 9%, respectively), but the reduction in LDL-C is similar to that when using atorvastatin without food. The concentration of atorvastatin when used in the evening is lower than in the morning (by approximately 30%). A linear relationship was revealed between the degree of absorption and the dose of the drug.
Bioavailability – 12%, systemic bioavailability of inhibitory activity against HMG-CoA reductase – 30%. Low systemic bioavailability is due to first-pass metabolism in the gastrointestinal mucosa and during the first passage through the liver.
Average Vd – 381 l, binding to blood plasma proteins – 98%. Metabolized primarily in the liver under the influence of isoenzymes CYP3A4, CYP3A5 and CYP3A7 with the formation of pharmacologically active metabolites (ortho- and parahydroxylated derivatives, β-oxidation products). In vitro, ortho- and parahydroxylated metabolites have an inhibitory effect on HMG-CoA reductase comparable to that of atorvastatin. The inhibitory effect of the drug on HMG-CoA reductase is approximately 70% determined by the activity of circulating metabolites.
Excreted through the intestines with bile after hepatic and/or extrahepatic metabolism (not subject to pronounced enterohepatic recirculation).
T1/2 – 14 hours. Inhibitory activity against HMG-CoA reductase lasts about 20-30 hours due to the presence of active metabolites. Less than 2% of the dose taken orally is determined in the urine. It is not excreted during hemodialysis.
Special instructions
Special instructions
Before starting Torvacard therapy, the patient must be prescribed a standard cholesterol-lowering diet, which he must follow during the entire treatment period.
The use of HMG-CoA reductase inhibitors to reduce blood lipid levels can lead to changes in biochemical parameters reflecting liver function. Liver function should be monitored before starting therapy, 6 weeks, 12 weeks after starting Torvacard, and after each dose increase, as well as periodically (for example, every 6 months). An increase in the activity of liver enzymes in the blood serum may be observed during Torvacard therapy. Patients who experience elevated transaminase levels should be monitored until enzyme levels return to normal. If ALT or AST values are more than 3 times the upper limit of normal (ULN), it is recommended to reduce the Torvacard dose or discontinue treatment.
Torvacard should be used with caution in patients who abuse alcohol and/or have liver disease. Active liver disease or persistent elevation of aminotransferase activity of unknown origin are contraindications to the use of Torvacard.
Treatment with Torvacard may cause myopathy. In patients with widespread myalgia, muscle soreness or weakness and/or a marked increase in CPK activity, the possibility of developing myopathy (muscle pain and weakness in combination with an increase in CPK activity by more than 10 times the ULN) should be kept in mind. Patients should be warned that they should immediately tell their doctor if they experience unexplained muscle pain or weakness if they are accompanied by malaise or fever. Treatment with Torvacard should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy. The risk of myopathy during treatment with other drugs in this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, niacin, or azole antifungals. Many of these drugs inhibit CYP3A4-mediated metabolism and/or drug transport. Atorvastatin is biotransformed by CYP3A4. When prescribing atorvastatin in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungals or nicotinic acid in lipid-lowering doses, the expected benefits and risks of treatment should be carefully weighed and patients should be regularly monitored for muscle pain or weakness, especially during the first months of treatment and during periods of increasing dosage of any drug. In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy.
When using atorvastatin, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Torvacard therapy should be temporarily discontinued or completely discontinued if signs of possible myopathy appear or if there is a risk factor for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances, and uncontrolled seizures). Before starting therapy with Torvacard, it is necessary to try to achieve control of hypercholesterolemia through adequate diet therapy, increased physical activity, weight loss in obese patients and treatment of other conditions. Patients should be advised to seek immediate medical attention if they experience unexplained muscle pain or weakness, especially if accompanied by malaise or fever.
Impact on the ability to drive a car and operate machinery
No adverse effects of Torvakard on the ability to drive or use machines have been reported.
Active ingredient
Active ingredient
Atorvastatin
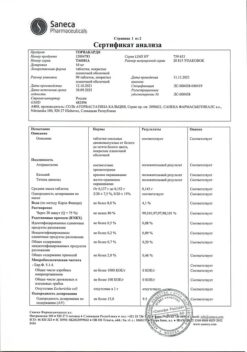
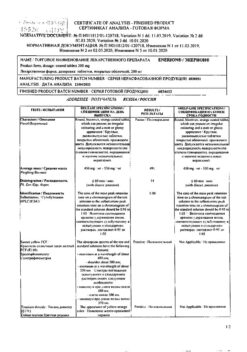
Composition
Composition
1 tablet contains:
Active ingredient: atorvastatin (in the form of calcium salt) 20 mg;
Excipients: heavy magnesium oxide, microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, low-substituted hydroxypropylcellulose LH21, colloidal silicon dioxide, magnesium stearate.
Shell composition: hypromellose 2910/5, macrogol 6000, titanium dioxide, talc.
Pregnancy
Pregnancy
Atorvastatin is contraindicated for use during pregnancy and lactation (breastfeeding).
It is not known whether atorvastatin is excreted in breast milk. Considering the possibility of adverse events in infants, if it is necessary to use the drug during lactation, the issue of stopping breastfeeding should be decided. Women of reproductive age should use adequate contraception during treatment. Atorvastatin should only be prescribed to women of reproductive age if the likelihood of pregnancy is very low and the patient is informed of the possible risk of treatment to the fetus.
Contraindications
Contraindications
acute liver diseases
severe general condition of the patient
hypersensitivity to the drug Torvacard.
Side Effects
Side Effects
Infectious and parasitic diseases: often – nasopharyngitis.
From the blood and lymphatic system: rarely – thrombocytopenia.
From the immune system: often – allergic reactions; very rarely – anaphylaxis.
Metabolism and nutrition: often – hyperglycemia; uncommon – hypoglycemia, weight gain, anorexia.
From the psyche: infrequently – sleep disturbances, including insomnia and nightmares.
From the nervous system: often – headache; infrequently – dizziness, paresthesia, hypoesthesia, taste perversion, loss or decrease in memory; rarely – peripheral neuropathy.
From the side of the organ of vision: infrequently – decreased clarity of vision; rarely – visual impairment.
From the organ of hearing and labyrinthine disorders: infrequently – tinnitus; very rarely – hearing loss.
From the respiratory system, chest and mediastinal organs: often – pain in the pharynx and trachea, nosebleeds.
From the digestive system: often – constipation, flatulence, dyspepsia, nausea, diarrhea; uncommon – vomiting, pain in the upper and lower abdomen, belching, pancreatitis.
From the liver and biliary tract: infrequently – hepatitis; rarely – cholestasis; very rarely – liver failure.
From the skin and subcutaneous tissues: infrequently – urticaria, skin rash, itching, alopecia; rarely – angioedema, bullous dermatitis, including erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis.
From the musculoskeletal and connective tissue: often – myalgia, arthralgia, pain in the extremities, muscle spasms, swelling of the joints, back pain; uncommon – neck pain, muscle weakness; rarely – myopathy, myositis, rhabdomyolysis, tendinopathy (sometimes complicated by tendon rupture).
General disorders and disorders at the injection site: uncommon – malaise, asthenia, chest pain, peripheral edema, fatigue, fever.
Laboratory and instrumental data: often – increased activity of liver transaminases, increased activity of CPK; infrequently – leukocyturia, increased concentration of glycosylated hemoglobin.
Interaction
Interaction
The risk of myopathy during treatment with other drugs in this class is increased by concomitant use of cyclosporine, fibrates, erythromycin, azole antifungals, and niacin.
With simultaneous oral administration of atorvastatin and a suspension containing magnesium and aluminum hydroxide, plasma concentrations of atorvastatin decreased by approximately 35%, but the degree of reduction in LDL-C levels did not change.
With simultaneous use, atorvastatin does not affect the pharmacokinetics of antipyrine, so interactions with other drugs metabolized by the same cytochrome isoenzymes are not expected.
With simultaneous use of colestipol, plasma concentrations of atorvastatin were reduced by approximately 25%. However, the lipid-lowering effect of the combination of atorvastatin and colestipol was superior to that of each drug individually.
With repeated administration of digoxin and atorvastatin at a dose of 10 mg, the equilibrium concentrations of digoxin in the blood plasma did not change. However, when digoxin was used in combination with atorvastatin at a dose of 80 mg/day, digoxin concentrations increased by approximately 20%. Patients receiving digoxin in combination with atorvastatin require observation.
With simultaneous use of atorvastatin and erythromycin (500 mg 4 times / day) or clarithromycin (500 mg 2 times / day), which inhibit the CYP3A4 isoenzyme, an increase in the concentration of atorvastatin in the blood plasma was observed.
With simultaneous use of atorvastatin (10 mg 1 time / day) and azithromycin (500 mg 1 time / day), the concentration of atorvastatin in the blood plasma did not change.
Atorvastatin did not have a clinically significant effect on plasma concentrations of terfenadine, which is metabolized primarily by CYP3A4; therefore, it is unlikely that atorvastatin will significantly affect the pharmacokinetic parameters of other CYP3A4 substrates.
When atorvastatin was coadministered with an oral contraceptive containing norethindrone and ethinyl estradiol, significant increases in the AUC of norethindrone and ethinyl estradiol by approximately 30% and 20%, respectively, were observed. This effect should be taken into account when choosing an oral contraceptive for a woman receiving atorvastatin.
When studying the interaction of atorvastatin with warfarin and cimetidine, no signs of clinically significant interaction were found.
With simultaneous use of atorvastatin 80 mg and amlodipine 10 mg, the pharmacokinetics of atorvastatin at steady state did not change.
The simultaneous use of atorvastatin with protease inhibitors, known as inhibitors of the CYP3A4 isoenzyme, was accompanied by an increase in the concentration of atorvastatin in the blood plasma.
There were no clinically significant adverse interactions between atorvastatin and antihypertensive drugs, or with estrogens. Interaction studies with all specific drugs have not been conducted.
No pharmaceutical incompatibilities known.
Overdose
Overdose
Symptoms: possible arterial hypotension.
Treatment: symptomatic therapy. There is no specific antidote. Hemodialysis is ineffective.
Storage conditions
Storage conditions
At 10–30 °C
Shelf life
Shelf life
2 years
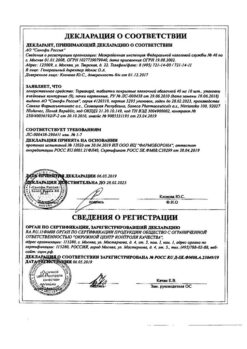
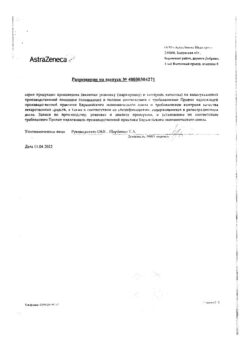
Manufacturer
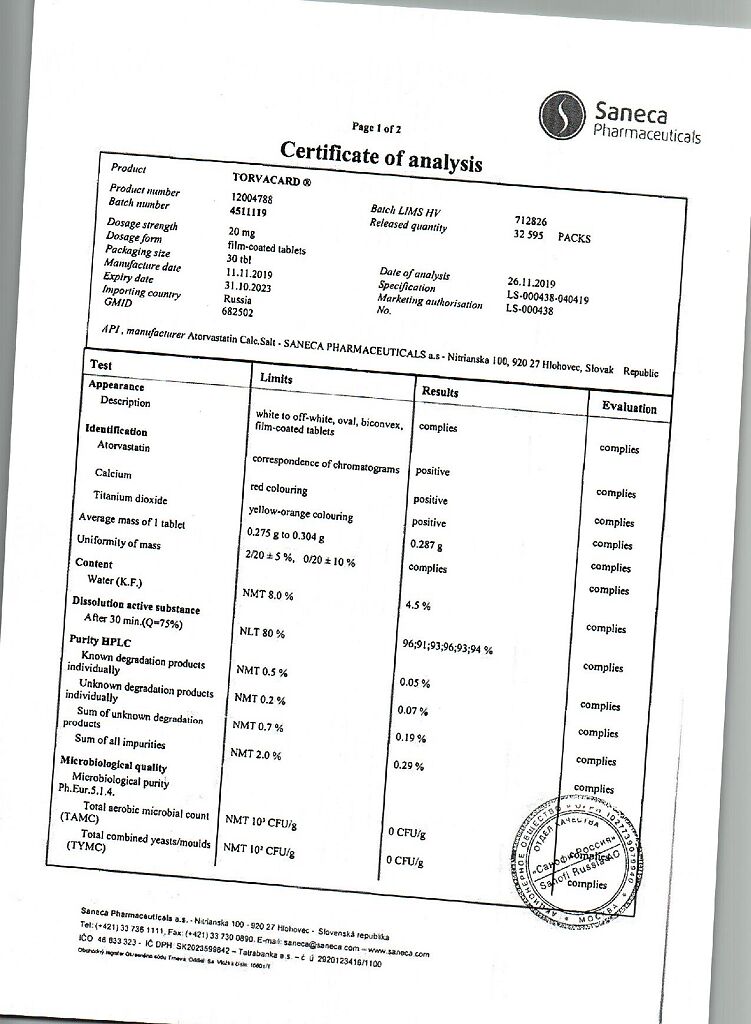
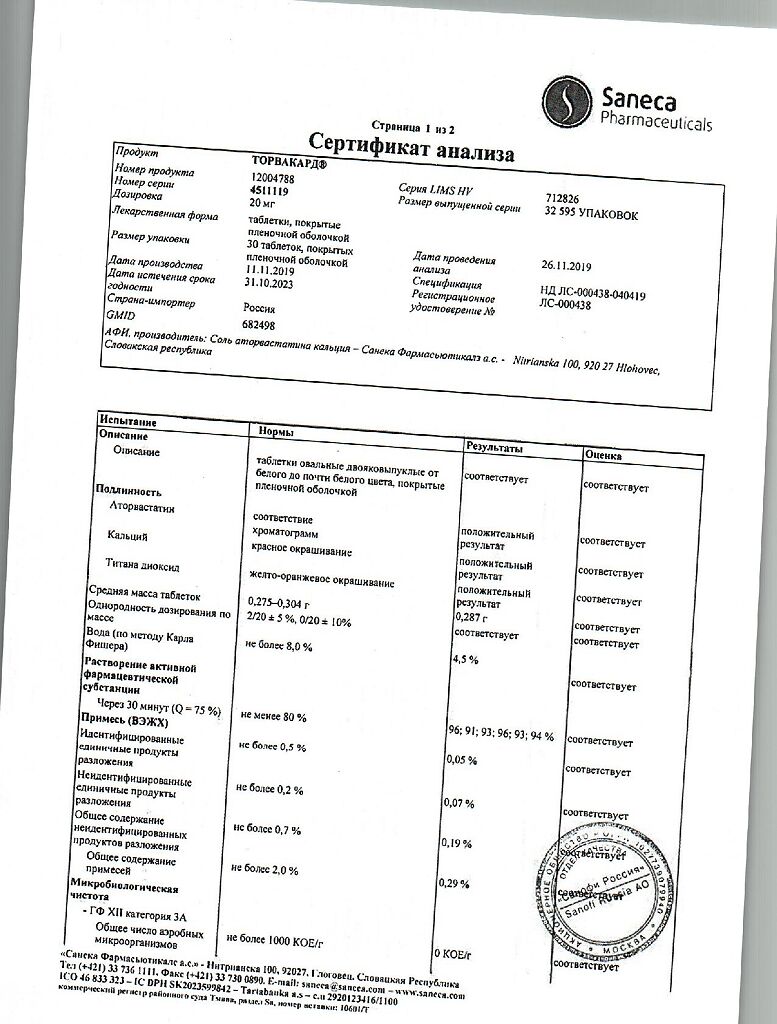
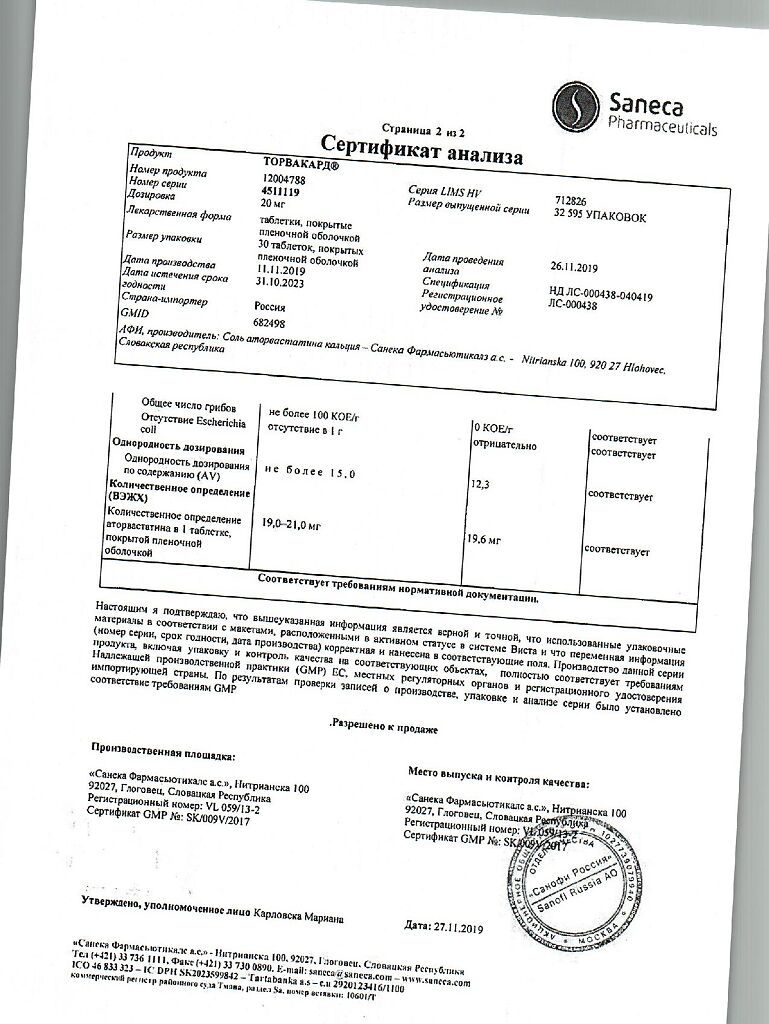
Manufacturer
Saneka Pharmaceuticals a.s., Slovakia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At 10-30 °C |
| Manufacturer | Saneka Pharmaceuticals a.s., Slovakia |
| Medication form | pills |
| Brand | Saneka Pharmaceuticals a.s. |
Other forms…
Related products
Buy Torvacard, 20 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.