No products in the cart.
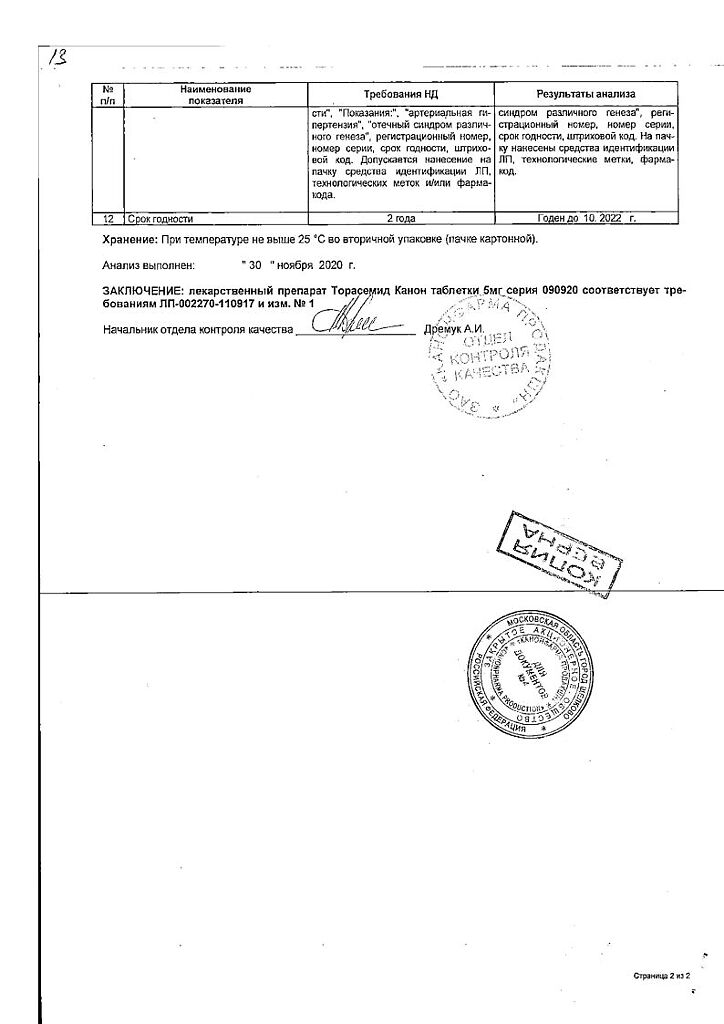
Torasemide Canon, tablets 5 mg 60 pcs
€11.91 €9.93
Description
Thoracemide is a loop diuretic; at low doses used for antihypertensive treatment, it has weak diuretic and saluretic effects. At higher doses, thoracemide increases diuresis in a dose-dependent manner.
Thorasemide shows maximum diuretic activity 2-3 h after oral administration.
Pharmacokinetics
Thoracemide is rapidly and almost completely absorbed after oral administration; Cmax in blood serum is reached 1-2 h after administration. Systemic bioavailability is 80-90%. Torasemide binding to plasma proteins is >99%, metabolites M1, M3 and M5 – 86; 95 and 97%, respectively.
The estimated volume of distribution is 16 L. Torasemide is metabolized by oxidation and hydroxylation to form three metabolites: M1, M3 and M5. M5 is pharmacologically inactive, and metabolites M1 and M3 account for approximately 10% of the drug’s pharmacological action.
The T1/2 of thorasemide and its metabolites in healthy volunteers is 3-4 hours. Total clearance of thorasemide is 40 ml/min, renal clearance is about 10 ml/min. About 80% of the dose is excreted as unchanged torasemide (24%) and its metabolites: M1 (12%), M3 (3%), M5 (41%).
In renal failure, the T1/2 of thorasemide does not change, and the T1/2 of metabolites M3 and M5 is prolonged. Torasemide and its metabolites are practically not excreted by hemodialysis or hemofiltration.
In patients with impaired liver function or heart failure, the T1/2 of thoracemide and the M5 metabolite are slightly prolonged, but cumulation of thoracemide and its metabolites is unlikely.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
1 tablet contains:
The active ingredient:
torasemide 5 mg;
Excipients:
corn starch pregelatinized,
silicon dioxide colloidal,
croscarmellose sodium,
mannitol,
magnesium stearate,
microcrystalline cellulose.
How to take, the dosage
How to take, the dosage
The drug is taken orally, at any convenient time, regardless of meals, preferably at the same time. The tablets should be taken without chewing and with water.
In case of edema syndrome in chronic heart failure, the initial dose is 10-20 mg once daily. If necessary the dose can be doubled until achieving the desired effect.
In case of edema syndrome in renal disease the initial dose is 20 mg 1 time per day. If necessary, the dose may be doubled until the desired effect is achieved.
In edematous syndrome with liver disease the initial dose is 5-10 mg once daily. If necessary, the dose may be doubled until the desired effect is achieved.
A single dose of more than 40 mg is not recommended because its effect has not been studied.
The drug Torasemide Canon is prescribed for a long period or until the edema disappears.
In arterial hypertension, the initial dose is 5 mg once daily. If there is no adequate BP reduction within 4-6 weeks, the dose is increased to 10 mg once daily. If this dose does not give the desired effect, an antihypertensive drug of another group should be added to the treatment regimen.
Patients of advanced age do not require dose adjustment.
Interaction
Interaction
In concomitant use of mineral and glucocorticosteroids, amphotericin B increases the risk of hypokalemia; with cardiac glycosides – increased risk of glycoside intoxication due to hypokalemia (for high- and low-polar) and prolongation of T1/2 (for low-polar).
The drug Toracemide Canon increases the concentration and risk of nephrotoxic and ototoxic effects of chloramphenicol, etacrynic acid, antibiotics, salicylates, platinum preparations (Pt), amphotericin B (due to competitive renal excretion).
Simultaneous or concomitant administration of Torasemide Canon with ACE inhibitors or angiotensin II receptor antagonists may lead to a sharp fall in BP. This can be avoided by reducing the initial dose of the ACE inhibitor or by reducing the dose of Toracemide Canon (or temporarily cancelling it).
The NSAIDs, sucralfate, methotrexate and probenecid reduce diuretic effect due to inhibition of prostaglandin synthesis, impaired plasma renin activity and aldosterone excretion.
Torasemide increases the hypotensive effect of antihypertensive agents, neuromuscular blockade of depolarizing myorelaxants (suxamethonium) and weakens the effect of nondepolarizing myorelaxants (tubocurarin).
Torasemide may increase the toxicity of lithium preparations and ototoxicity of etacrynic acid.
Thorasemide increases the effectiveness of diazoxide and theophylline, reduces the effectiveness of hypoglycemic agents, allopurinol.
Presor amines and the drug Torasemide Canon mutually reduce efficacy.
Drugs that block tubular secretion increase the serum concentration of Toracemide Canon.
Concomitant use of cyclosporine and the drug Toracemide Canon increases the risk of gouty arthritis because cyclosporine may cause impairment of urate excretion by kidneys, and thoracemide may cause hyperuricemia.
It has been reported that patients at high risk of nephropathy taking oral thoracemide were more likely to have impaired renal function when given radiopaque agents than patients at high risk of nephropathy who underwent IV hydration before radiopaque administration.
The bioavailability and, consequently, the effectiveness of thoracemide may be reduced when co-therapy with colestyramine.
Special Instructions
Special Instructions
The drug Toracemide Canon should be used strictly on prescription.
Patients with hypersensitivity to sulfonamides and sulfonylurea derivatives may have cross-sensitivity to the drug Toracemide Canon.
In patients receiving Toracemide Canon in high doses, it is not advisable to restrict table salt intake and potassium preparations to avoid development of hyponatremia, hypokalemia and metabolic alkalosis.
The risk of hypokalemia is greatest in patients with cirrhosis, marked diuresis, with insufficient intake of electrolytes in food, and with concomitant treatment with corticosteroids or ACTH.
A higher risk of water-electrolyte balance disorders is noted in patients with renal insufficiency. During the course of treatment with Torasemide Canon it is necessary to monitor the concentration of plasma electrolytes (including sodium, calcium, potassium, magnesium), acid-base status, residual nitrogen, creatinine, uric acid periodically and if necessary provide an appropriate therapy (with higher frequency in patients with frequent vomiting and against parenteral administration of fluids).
In patients with developed water-electrolyte disorder, hypovolemia or prerenal azotemia, laboratory findings may include: hyper- or hyponatremia, hyper- or hypochloremia, hyper- or hypokalemia, acid-base balance disorders and increased blood urea concentration.
If these disorders occur, Torasemide Canon should be discontinued until normal values are restored, and then treatment should be resumed at a lower dose.
If azotemia and oliguria appear or worsen in patients with severe progressive renal disease, it is recommended that treatment with Torasemide Canon be suspended.
The dosage regimen of patients with ascites due to liver cirrhosis should be chosen under hospital conditions (disturbances of water-electrolyte balance may lead to hepatic coma). Regular monitoring of plasma electrolytes is indicated for this category of patients.
The use of Torasemide Canon may cause an aggravation of gout.
In patients with diabetes mellitus or with reduced glucose tolerance, periodic monitoring of blood and urine glucose concentrations is required.
In patients with prostatic hyperplasia, ureteral narrowing, diuresis control is necessary due to the possibility of acute urinary retention.
In patients with cardiovascular disease, especially those taking cardiac glycosides, diuretic-induced hypokalemia may cause arrhythmias.
Impact on driving and operating machinery
Patients should refrain from driving and engaging in other potentially dangerous activities requiring increased concentration and quick psychomotor reactions during treatment with Torasemide Kanon.
Contraindications
Contraindications
Side effects
Side effects
WHO Classification of the incidence of side effects: very frequent – â¥1/10 appointments (>10%), frequent – â¥1/100 to <1/10 appointments (>1% and <10%), infrequent – â¥1/1000 to <1/100 appointments (>01% and <1%), infrequent â¥1/10,000 to <1/1000 appointments (>0.01% and <0.1%), very rare <1/10,000 appointments (<0.01%), frequency unknown – cannot be estimated from available data.
Hematopoietic system: frequency unknown – thrombocytopenia, leukopenia, agranulocytosis, aplastic or hemolytic anemia.
Mechanical and nutritional disorders: infrequent – polydipsia, hypercholesterolemia, hypertriglyceridemia; frequency unknown – decreased glucose tolerance (possible manifestation of latent diabetes).
Water-electrolyte and acid-base balance: frequency is unknown – hypokalemia, hyponatremia, hypomagnesemia, hypocalcemia, hypochloremia, metabolic alkalosis, hypovolemia, dehydration (more often in elderly patients), which may lead to hemoconcentration with a tendency to develop clots.
Nervous system disorders: frequently – dizziness, headache, somnolence; frequency is unknown – confusion, fainting, paresthesia in extremities (feeling of numbness, “creeping crawlies” and tingling).
Visual organs: frequency is unknown – visual impairment.
Hearing organ: frequency unknown – hearing impairment, tinnitus and hearing loss (usually reversible) usually in patients with renal failure or hypoproteinemia (nephrotic syndrome).
Cardiovascular system disorders: infrequent – extrasystole, arrhythmia, tachycardia.
Vascular disorders: frequency is unknown – excessive reduction of BP, orthostatic hypotension, collapse, deep vein thrombosis, thromboembolism.
Respiratory system disorders: infrequent – nasal bleeding.
The digestive system: frequent – diarrhea; infrequent – abdominal pain, flatulence; frequency unknown – dry mouth, nausea, vomiting, loss of appetite, pancreatitis, dyspeptic disorders, intrahepatic cholestasis.
Urinary system disorders: often – increased frequency of urination, polyuria, nycturia; infrequent – frequent urge to urinate; frequency unknown – oliguria, urinary retention (in patients with urinary tract obstruction), interstitial nephritis, hematuria.
Gender and mammary gland disorders: frequency unknown – decreased potency.
Skin and subcutaneous tissue disorders: frequency unknown – exfoliative dermatitis, purpura, vasculitis, photosensitization.
Muscular system: infrequent – muscle cramps of the lower extremities; frequency unknown – muscle weakness.
Allergic reactions: infrequent – severe anaphylactic reactions up to and including shock, which so far have only been described after IV administration; frequency is unknown – skin itching, rash, urticaria, erythema multiforme.
Laboratory and instrumental data: frequency unknown – hypercholesterolemia, hypertriglyceridemia, hyperuricemia, slight increase in the concentration of ALP in blood, transient increase in creatinine and urea in blood, increased activity of some liver enzymes (eg, gamma-glutamyltransferase).
Others: infrequent – fever, asthenia, weakness, increased fatigue, hyperactivity, nervousness.
If any of the side effects listed in the instructions are aggravated or any other side effects not listed in the instructions are noted, the patient should tell their physician.
Overdose
Overdose
Symptoms: increased diuresis, accompanied by decreased CBC and electrolyte imbalance, followed by excessive BP decrease, drowsiness and confusion, collapse. Gastrointestinal disorders may be observed.
Treatment: no specific antidote; provocation of vomiting, gastric lavage, activated charcoal. Symptomatic therapy, dose reduction or drug withdrawal and simultaneous repletion of the blood circulation and parameters of the water-electrolyte balance and acid-base status under control of serum concentrations of electrolytes, hematocrit.
Hemodialysis is not effective because excretion of torasemide and its metabolites is not accelerated.
Pregnancy use
Pregnancy use
Toracemide has no teratogenic effect and fetotoxicity, it penetrates the placental barrier, causing water-electrolyte metabolism disorders and thrombocytopenia in the fetus.
The drug Toracemide Canon may be used during pregnancy only when the expected benefits to the mother exceed the potential risk to the fetus, under close medical supervision and only in minimal doses.
There is no data on excretion of thoracemide with breast milk, therefore if it is necessary to use the drug Thoracemide Canon during lactation, breastfeeding should be stopped.
Similarities
Similarities
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C. |
| Manufacturer | Kanonfarma Production ZAO, Russia |
| Medication form | pills |
| Brand | Kanonfarma Production ZAO |
Related products
Buy Torasemide Canon, tablets 5 mg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.