No products in the cart.
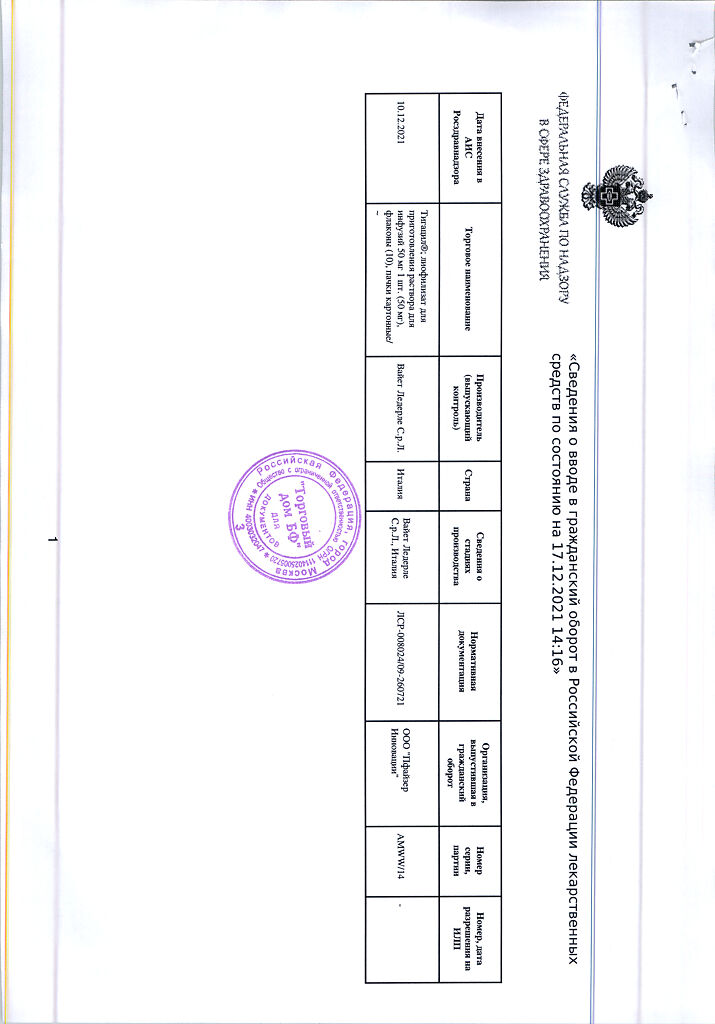
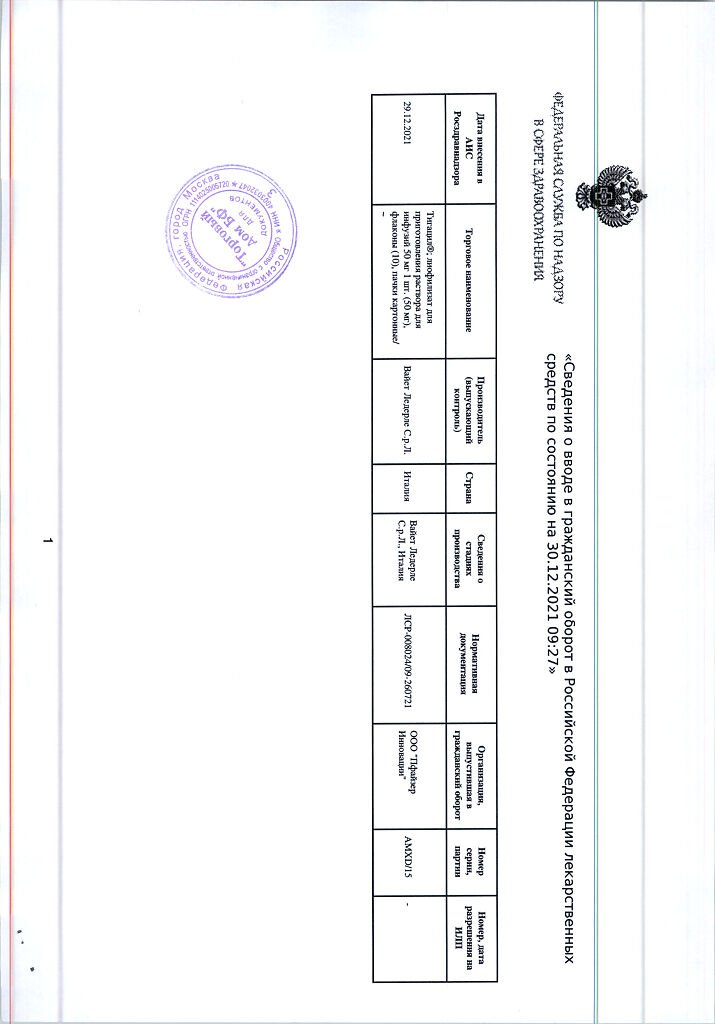
Tigacil, lyophilizate 50 mg 10 pcs
€496.51 €413.75
Description
Tigacil is an antibiotic of the glycylcycline group, structurally similar to tetracyclines. It inhibits protein translation in bacteria by binding to the 30S-subunit of ribosomes and blocking penetration of aminoacyl-tRNA molecules to the A-site of the ribosome, which prevents the incorporation of amino acid residues into growing peptide chains.
Tigecycline is believed to have bacteriostatic properties. A 4-fold MPC of tigecycline resulted in a two orders of magnitude decrease in the number of colonies of Enterococcus spp., Staphylococcus aureus and Escherichia coli.
The bactericidal effect of tigecycline was observed against Streptococcus pneumoniae, Haemophilus influenzae and Legionella pneumophila.
The mechanism of resistance development
Tigecycline can overcome the two main mechanisms of resistance of microorganisms observed against tetracyclines: ribosomal protection and active excretion.
In addition, tigecycline activity is not inhibited by the action of β-lactamases (including extended spectrum β-lactamases), nor by modification of bacterial membrane sites sensitive to the antibiotic, nor by active excretion of the antibiotic from the bacterial cell or by modification of the target of action (e.g. gyrase/topoisomerase).
Tigecycline thus has a broad spectrum of antibacterial activity. However, tigecycline lacks protection against the microbial resistance mechanism in the form of active excretion from the cell encoded by Proteeae and Pseudomonas aeruginosa chromosomes (MexXY-OprM efflux system).
There is no cross-resistance between tigecycline and most classes of antibiotics.
In general, microorganisms belonging to Proteus spp., Providencia spp. and Morganella spp. are less sensitive to tigecycline than other Enterobacteriaceae. In addition, some acquired resistance was found in Klebsiella pneumoniae, Enterobacter aerogenes and Enterobacter cloacae.
Decreased sensitivity of representatives of both groups to tigecycline is caused by overexpression of the gene of nonspecific active excretion of AsgAV, which provides resistance to many drugs. Acinetobacter baumannii has also been described to be hypersensitive to tigecycline.
The IPC reference values
The following are the IPC reference values established by the European Working Group on Antibiotic Susceptibility Testing (EUCAST).
| Pathogens | Sensitive | Resistant |
| Staphylococcus spp. | ≤ 0.5 mg/L | > 0.5 mg/L |
| Streptococcus spp, except S. pneumoniae | ≤ 0.25 mg/L | > 0.5 mg/L |
| Enterococcus spp. | ≤ 0.25 mg/L | > 0.5 mg/L |
| Enterobacteriaceae | ≤ 1 mg/L* | > 2 mg/l |
| Regardless of the pathogen species | ≤ 0.25 mg/L | > 0.5 mg/L |
* Reduced in vitro activity of tigecycline against Proteus spp, Providencia spp. and Morganella spp.
To Acinetobacter spp., Streptococcus pneumoniae, other streptococci, Haemophilus influenzae, Moraxella catarrhalis, Neisseria gonorrhoea and Neisseria meningitidis, there is no conclusive evidence of tigecycline effectiveness.
The efficacy of tigecycline for the treatment of intraabdominal infections caused by anaerobic bacteria has been established regardless of MPC, pharmacokinetic/pharmacodynamic parameters. Therefore, control MPK values are not presented.
We should note the wide range of MPC of tigecycline for Bacteroides spp. and Clostridium spp., in some cases exceeding 2 mg/L.
There are only limited data on the clinical efficacy of tigecycline in enterococcal infections. Nevertheless, a positive response to treatment with tigecycline for polymicrobial intra-abdominal infections has been shown.
The prevalence of acquired resistance in individual bacterial species may vary with time and geographic location.
The Gram-positive aerobic microorganisms are sensitive to the drug:
Enterococcus avium, Enterococcus casseliflavus, Enterococcus faecalis1,2 (including vancomycin-sensitive strains), Enterococcus faecalis (including vancomycin-resistant strains), Enterococcus gallinarum, Staphylococcus aureus1,2 (including methicillin-sensitive and resistant strains), Staphylococcus epidermidis (including methicillin-sensitive and resistant strains), Staphylococcus haemolyticus, Streptococcus agalactiae1,Streptococcus anginosus group1,2 (including S.anginosus, S.intermedius, and S.constellatus), Streptococcus pyogenes1,Streptococcus pneumoniae3 (penicillin-sensitive strains), Streptococcus pneumoniae (penicillin-resistant strains), Streptococci viridans group;
Gram-negative aerobic microorganisms: Aeromonas hydrophilia, Citrobacter freundii2, Citrobacter koseri, Enterobacter aerogenes, Enterobacter cloacae2, Escherichia coli1,2 (including broad-spectrum beta-lactamase-producing strains), Haemophilus influenzae3, Haemophilus parainfluenzae, Klebsiella oxytoca2, Klebsiella pneumoniae1,2 (including strains producing broad-spectrum β-lactamase), Legionella pneumophila3,Moraxella catarrhalis, Serratia marcescens, Bacteroides fragilis group1,2,Clostridium perfringens2,Peptostreptococcus spp.2,Peptostreptococcus micros, Prevotella spp.; atypical microorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae.
Species with possible development of acquired resistance: Acinetobacter baumannii, Burkholderia cepacia, Morganella morganii, Providencia spp., Proteus spp., Stenotrophomonas maltophilia.
Microorganisms with intrinsic resistance: Pseudomonas aeruginosa.
1,2,3 -species against which satisfactory activity has been demonstrated in clinical trials.
Pharmacokinetics
Intake
Since tigecycline is administered intravenously, it has 100% bioavailability.
Distribution
At concentrations of 0.1 to 1 µg/ml, the binding of tigecycline to plasma proteinsin vitro ranges from approximately 71% to 89%. In pharmacokinetic studies in animals and humans it has been shown that tigecycline is rapidly distributed in tissues.
In humans, the equilibrium Vd tigecycline is 500-700 L (7-9 L/kg), confirming the extensive distribution of tigecycline outside the plasma and its accumulation in tissues.
There are no data on the ability of tigecycline to penetrate through the BBB in humans.
The Cssmax tigecycline in serum was 866±233 ng/mL with 30-minute infusions and 634±97 ng/mL with 60-minute infusions. The AUC0-12 h was 2349±850 ng×hour/mL.
Metabolism
On average, less than 20% of tigecycline is metabolized. The major substance detected in urine and feces was unchanged tigecycline, but glucuronide, N-acetyl metabolite, and epimer of tigecycline were also detected.
Tigecycline does not inhibit metabolism mediated by the following six CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6 and CYP3A4 isoenzymes. It is neither a competitive inhibitor nor an irreversible inhibitor of cytochrome P450.
Elimation
It has been observed that 59% of the administered dose is excreted through the intestine (with most of the unchanged tigecycline entering the bile), and 33% is excreted by the kidneys. Additional routes of excretion are glucuronidation and renal excretion of unchanged tigecycline.
The total clearance of tigecycline after intravenous infusion is 24 l/h. Renal clearance accounts for approximately 13% of total clearance.
Tigecycline is characterized by polyexponential excretion from serum; the mean terminal T1/2 from serum after repeated doses is 42 hours, but significant individual differences are observed.
Pharmacokinetics in Special Clinical Cases
The pharmacokinetic profile of single-dose tigecycline is not altered in patients with mild hepatic impairment.
However, in patients with moderate to severe hepatic impairment (Child-Pugh class B and C), total clearance of tigecycline was decreased by 25% and 55%, and T1/2 increased by 23% and 43%, respectively.
In patients with renal impairment (QC)
The pharmacokinetics of tigecycline in elderly patients were generally not different from other age groups.
The pharmacokinetics of tigecycline in patients younger than 18 years have not been studied.
Clinically significant differences in the clearance of tigecycline in men and women have not been established.
The clearance of tigecycline is independent of race.
Clearance, including normalized by body weight, and AUC did not differ markedly in patients with different body weights, including those exceeding 125 kg. In patients with body weight more than 125 kg the AUC value was 25% lower. No data were available for patients with a body weight greater than 140 kg.
Indications
Indications
Complicated infections of the skin and soft tissues;
complicated intra-abdominal infections;
community-acquired pneumonia.
Pharmacological effect
Pharmacological effect
Tigacil is an antibiotic of the glycylcycline group, structurally similar to tetracyclines. Inhibits protein translation in bacteria by binding to the 30S subunit of ribosomes and blocking the penetration of aminoacyl-tRNA molecules into the A-site of the ribosome, which prevents the inclusion of amino acid residues in growing peptide chains.
Tigecycline is believed to have bacteriostatic properties. At 4 times the MIC of tigecycline, a two orders of magnitude decrease in the number of colonies of Enterococcus spp., Staphylococcus aureus and Escherichia coli was observed.
The bactericidal effect of tigecycline was noted against Streptococcus pneumoniae, Haemophilus influenzae and Legionella pneumophila.
Mechanism for developing resilience
Tigecycline can overcome the two main mechanisms of microbial resistance observed with tetracyclines: ribosomal protection and active clearance.
In addition, the activity of tigecycline is not inhibited by the action of β-lactamases (including extended-spectrum β-lactamases), or by modification of antibiotic-sensitive sites of the bacterial membrane, or by active removal of the antibiotic from the bacterial cell or by modification of the target of action (for example, gyrase/topoisomerase).
Thus, tigecycline has a broad spectrum of antibacterial activity. However, tigecycline lacks protection against the resistance mechanism of microorganisms in the form of active clearance from the cell, encoded by the chromosomes of Proteeae and Pseudomonas aeruginosa (MexXY-OprM efflux system).
There is no cross-resistance between tigecycline and most classes of antibiotics.
In general, microorganisms belonging to Proteus spp., Providencia spp. and Morganella spp., are less sensitive to tigecycline than other members of Enterobacteriaceae. In addition, some acquired resistance has been found in Klebsiella pneumoniae, Enterobacter aerogenes and Enterobacter cloacae.
The reduced sensitivity of representatives of both groups to tigecycline is due to overexpression of the gene for nonspecific active elimination of Ac-AB, which provides resistance to many drugs. Reduced sensitivity to tigecycline and Acinetobacter baumannii has been described.
MIC reference values
The MIC reference values established by the European Working Group on Antimicrobial Susceptibility Testing (EUCAST) are listed below.
Pathogens
Sensitive
Resistant
Staphylococcus spp.
≤ 0.5 mg/l
> 0.5 mg/l
Streptococcus spp., except S. pneumoniae
≤ 0.25 mg/l
> 0.5 mg/l
Enterococcus spp.
≤ 0.25 mg/l
> 0.5 mg/l
Enterobacteriaceae
≤ 1 mg/l*
> 2 mg/l
Regardless of the type of pathogen
≤ 0.25 mg/l
> 0.5 mg/l
* Decreased activity of tigecycline in vitro against Proteus spp., Providencia spp. was noted. and Morganella spp.
For Acinetobacter spp., Streptococcus pneumoniae, other streptococci, Haemophilus influenzae, Moraxella catarrhalis, Neisseria gonorrhoea and Neisseria meningitidis, there is no convincing evidence of the effectiveness of tigecycline.
The effectiveness of tigecycline for the treatment of intra-abdominal infections caused by anaerobic bacteria has been established, regardless of MIC and pharmacokinetic/pharmacodynamic parameters. Therefore, reference MIC values are not presented.
It should be noted that tigecycline has a wide range of MICs for Bacteroides spp. and Clostridium spp., in some cases exceeding 2 mg/l.
There are only limited data on the clinical effectiveness of tigecycline for enterococcal infections. However, a positive response to tigecycline treatment for polymicrobial intra-abdominal infections has been shown.
The prevalence of acquired resistance in individual bacterial species may vary over time and geographical location.
Gram-positive aerobic microorganisms are sensitive to the drug:
Enterococcus avium, Enterococcus casseliflavus, Enterococcus faecalis1,2 (including vancomycin-sensitive strains), Enterococcus faecalis (including vancomycin-resistant strains), Enterococcus gallinarum, Staphylococcus aureus1,2 (including methicillin-sensitive and resistant strains), Staphylococcus epidermidis (including methicillin-sensitive and resistant strains), Staphylococcus haemolyticus, Streptococcus agalactiae1, Streptococcus anginosus group1,2 (including S.anginosus, S.intermedius and S.constellatus), Streptococcus pyogenes1, Streptococcus pneumoniae3 (penicillin-sensitive strains), Streptococcus pneumoniae (penicillin-resistant strains strains), Streptococci viridans group;
gram-negative aerobic microorganisms: Aeromonas hydrophilia, Citrobacter freundii2, Citrobacter koseri, Enterobacter aerogenes, Enterobacter cloacae2, Escherichia coli1,2 (including strains producing broad-spectrum beta-lactamase), Haemophilus influenzae3, Haemophilus parainfluenzae, Klebsiella oxytoca2, Klebsiella pneumoniae1,2 (including strains producing broad-spectrum β-lactamase), Legionella pneumophila3, Moraxella catarrhalis, Serratia marcescens, Bacteroides fragilis group1,2, Clostridium perfringens2, Peptostreptococcus spp.2, Peptostreptococcus micros, Prevotella spp.; atypical microorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae.
Species that may develop acquired resistance: Acinetobacter baumannii, Burkholderia cepacia, Morganella morganii, Providencia spp., Proteus spp., Stenotrophomonas maltophilia.
Microorganisms with their own resistance: Pseudomonas aeruginosa.
1,2,3 – species for which satisfactory activity has been demonstrated in clinical studies.
Pharmacokinetics
Suction
Since tigecycline is administered intravenously, it is characterized by 100% bioavailability.
Distribution
At concentrations from 0.1 to 1 μg/ml, the binding of tigecycline to plasma proteins in vitro varies from approximately 71% to 89%. Pharmacokinetic studies in animals and humans have shown that tigecycline is rapidly distributed into tissues.
In the human body, the equilibrium Vd of tigecycline is 500-700 l (7-9 l/kg), which confirms the extensive distribution of tigecycline outside the plasma and its accumulation in tissues.
There are no data on the ability of tigecycline to penetrate the BBB in the human body.
Tigecycline serum Cssmax was 866±233 ng/ml for 30-minute infusions and 634±97 ng/ml for 60-minute infusions. AUC0-12 hours was 2349±850 ng×hour/ml.
Metabolism
On average, less than 20% of tigecycline is metabolized. The main substance found in urine and feces was unchanged tigecycline, but a glucuronide, an N-acetyl metabolite, and an epimer of tigecycline were also detected.
Tigecycline does not suppress metabolism mediated by the following six isoenzymes CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6 and CYP3A4. It is neither a competitive inhibitor nor an irreversible inhibitor of cytochrome P450.
Removal
It was noted that 59% of the prescribed dose is excreted through the intestines (with most of the unchanged tigecycline entering the bile), and 33% is excreted by the kidneys. Additional routes of elimination are glucuronidation and excretion of unchanged tigecycline by the kidneys.
The total clearance of tigecycline after intravenous infusion is 24 l/h. Renal clearance accounts for approximately 13% of total clearance.
Tigecycline has a polyexponential serum clearance, with a mean serum terminal T1/2 after repeated doses of 42 hours, but significant individual differences are observed.
Pharmacokinetics in special clinical situations
In patients with mild hepatic impairment, the pharmacokinetic profile of a single dose of tigecycline does not change.
However, in patients with moderate to severe hepatic impairment (Child-Pugh class B and C), the total clearance of tigecycline was reduced by 25% and 55%, and T1/2 was increased by 23% and 43%, respectively.
In patients with renal failure (KR
The pharmacokinetics of tigecycline in elderly patients were generally no different from other age groups.
The pharmacokinetics of tigecycline in patients under 18 years of age have not been studied.
Clinically significant differences in the clearance of tigecycline between men and women have not been established.
Tigecycline clearance does not vary by race.
Clearance, incl. normalized by body weight, and AUC did not differ significantly in patients with different body weights, including those exceeding 125 kg. In patients weighing more than 125 kg, the AUC value was 25% lower. There are no data on patients weighing more than 140 kg.
Special instructions
Special instructions
To reduce the development of resistance and ensure the effectiveness of therapy, it is necessary to use Tigacil only for the treatment and prevention of infectious diseases caused by sensitive microorganisms.
To select and adjust antibacterial therapy, if possible, microbiological identification of the pathogen should be carried out and its sensitivity to tigecycline should be determined. Tigacil can be used for empirical antibacterial monotherapy until the results of microbiological tests are obtained.
Antibiotics belonging to the glycylcycline class are structurally similar to antibiotics from the tetracycline class. Tigacil can cause adverse reactions similar to adverse reactions to antibiotics of the tetracycline class.
Such reactions may include increased photosensitivity, intracranial hypertension, pancreatitis and anti-anabolic effects leading to increased blood urea nitrogen, azotemia, acidosis and hypophosphatemia.
Therefore, Tigacil should be used with caution in patients with known sensitivity to tetracycline antibiotics.
Anaphylactic/anaphylactoid reactions, incl. anaphylactic shock is observed with the use of almost all antibacterial agents, including Tigacil.
Patients who experience changes in liver test results during treatment with Tigacil should be observed to promptly identify signs of liver dysfunction (single cases of significant liver dysfunction and liver failure have been reported) and to assess the benefit-risk ratio of continuing Tigacil therapy.
The development of undesirable reactions is possible after therapy has been completed.
The effectiveness and safety of Tigacil in patients with hospital-acquired pneumonia has not been confirmed by the results of clinical studies.
Diarrhea associated with Clostridium difficile has been reported when taking almost all antibacterial drugs, including Tigacil.
If Clostridium difficile-associated diarrhea is suspected or confirmed, it may be necessary to discontinue use of antibiotics other than those prescribed to treat Clostridium difficile infection.
When using tigecycline, the development of pseudomembranous colitis of varying severity is possible. The possibility of such a diagnosis should be considered if diarrhea occurs during or after completion of treatment.
When prescribing Tigacil to patients with complicated intra-abdominal infections due to intestinal perforation, or patients with incipient sepsis or septic shock, the advisability of using combination antibacterial therapy should be considered.
The use of Tigacil, like any other antibiotic, can promote excessive growth of non-susceptible microorganisms, including fungi. Patients should be closely monitored during treatment. When superinfection is diagnosed, appropriate measures should be taken.
The effect of cholestasis on the pharmacokinetics of tigecycline has not been established. Excretion in bile accounts for approximately 50% of the total excretion of tigecycline. Therefore, patients with cholestasis should be under medical supervision.
Experience with the use of Tigacil for the treatment of infections in patients with severe concomitant diseases is limited.
The use of Tigacil during the formation of teeth can lead to a change in the color of the teeth to yellow, gray, or brown. Tigacil should not be used during tooth development unless other drugs are ineffective or contraindicated.
Use in pediatrics
The effectiveness and safety of the drug in children and adolescents under 18 years of age have not been established.
Impact on the ability to drive vehicles and operate machinery
Studies of the effect of tigecycline on the ability to drive vehicles and operate machinery have not been conducted. Patients receiving tigecycline may experience dizziness, which may affect the ability to drive and use machines.
Active ingredient
Active ingredient
Tigecycline
Composition
Composition
1 bottle of lyophilisate for preparing a solution for infusion contains:
active ingredient:
tigecycline 50 mg,
excipients:
lactose monohydrate,
hydrochloric acid q.s to pH,
sodium hydroxide q.s to pH.
Pregnancy
Pregnancy
During pregnancy, the use of Tigacil is permissible only in cases of extreme necessity, when the benefit to the mother outweighs the possible risk to the fetus.
There are no data on the excretion of tigecycline into breast milk in humans.
If it is necessary to prescribe tigecycline during lactation, breastfeeding should be stopped. There is no experience with the use of the drug Tigacil during childbirth.
Contraindications
Contraindications
Hypersensitivity to the components of the drug Tigacil; hypersensitivity to tetracycline antibiotics.
The drug should be used with caution in severe liver failure.
Side Effects
Side Effects
The most commonly observed symptoms are nausea (29.9%) and vomiting (19.9%), which usually occur at the beginning of treatment (on the first or second day of treatment) and, in most cases, have a mild or moderate course. The most common reasons for discontinuation of therapy with Tigacil® were nausea (1.6%) and vomiting (1.3%).
Side effects are presented by organs and systems in the classification: very often (≥1/10); often (from ≥1/100 to <1/10); uncommon (from ≥1/1000 to <1/100); rare (from ≥1/10000 to <1/1000); very rare (≤1/10000), isolated cases (spontaneous post-marketing reports).
From the blood system and hematopoietic organs:
Common: increased activated partial thromboplastin time (aPTT), increased prothrombin time (PT), anemia, thrombocytopenia.
Uncommon: eosinophilia, increased international normalized ratio (INR).
From the immune system:
Isolated cases: anaphylactic/anaphylactoid reactions.
From the nervous system:
Common: dizziness, headache.
Uncommon: taste disturbance.
From the cardiovascular system:
Common: phlebitis.
Uncommon: thrombophlebitis.
From the gastrointestinal tract:
Very common: nausea, vomiting, diarrhea.
Common: abdominal pain, dyspepsia, anorexia.
Uncommon: acute pancreatitis.
From the hepatobiliary system:
Often: increased aspartate aminotransferase (AST) activity in blood plasma*, increased alanine aminotransferase (ALT) activity in blood plasma*, hyperbilirubinemia.
Uncommon: jaundice.
Isolated cases: severe liver dysfunction and liver failure, cholestasis.
From the skin and subcutaneous fat
Common: itching, rash.
Isolated cases: severe skin reactions, including Stevens-Johnson syndrome.
From the genitourinary system:
Uncommon: vaginal candidiasis, vaginitis, leukorrhea.
General reactions and reactions at the injection site:
Common: asthenia, delayed wound healing, abscess, infection, injection site reactions, sepsis.
Uncommon: inflammation, pain, swelling and phlebitis at the injection site, chills, septic shock, allergic reactions.
Laboratory indicators:
Often: increased blood urea nitrogen, increased alkaline phosphatase activity in the blood plasma, increased amylase activity in the blood plasma, hypoproteinemia.
Uncommon: increased blood creatinine, hypocalcemia, hyponatremia, hypoglycemia.
From the respiratory system:
Common: pneumonia.
Reactions characteristic of antibiotics: pseudomembranous colitis.
*increased activity of ALT and AST was noted more often after the end of therapy with Tigacil®.
A pooled analysis of clinical data from 13 phase 3 and 4 studies of the use of Tigacil® for registered and unregistered indications revealed higher overall mortality (i.e., death from any cause, including those unrelated to treatment) in patients with severe infections receiving Tigacil®.
Overall mortality in patients receiving Tigacil® was 4% (150/3788), comparator drugs – 3% (110/3646), the difference in the relative risk of death was 0.6% (confidence interval (CI): 0.1 – 1.2).
The reasons for the increase in overall mortality in patients receiving Tigacil® have not been established. In general, deaths were the result of worsening infection, complications of infection, or comorbidities.
Children
Data on the use of tigecycline in children are limited to two pharmacokinetic studies and one open-label clinical trial in a small group of children. No new or unexpected data on the safety of the drug were identified in these studies.
In an open-label, single-dose escalation pharmacokinetic study, the safety of tigecycline was examined in 25 pediatric patients (8 to 16 years) who had recently experienced an infectious disease.
The side effect profile in children was generally similar to that in adults.
The safety of tigecycline was also studied in 58 pediatric patients (8-11 years), with complicated skin and soft tissue infections (15 patients), complicated intra-abdominal infections (24 patients), or community-acquired pneumonia (19 patients).
The side effect profile in these 58 patients was similar to that in adults, with the exception of nausea (48.3%), vomiting (46.6%) and increased plasma lipase levels (6.9%), which were observed more often in children than in adults.
Interaction
Interaction
Compatibility/incompatibility with drugs and solvents when administered simultaneously
Compatibility
Tigacil® is compatible with 0.9% sodium chloride solution, 5% dextrose injection or lactated Ringer’s solution.
When administered through a T-shaped catheter, Tigacil® dissolved in 0.9% sodium chloride solution or 5% dextrose solution for injection is compatible with amikacin, dobutamine, dopamine, gentamicin, haloperidol, lactated Ringer’s solution, lidocaine, metoclopramide, morphine, norepinephrine, piperacillin/tazobactam (a dosage form containing ethylenediaminetetraacetate – EDTA), potassium chloride, propofol, ranitidine, theophylline and tobramycin.
Incompatibility
When used through a T-shaped catheter, Tigacil® is incompatible with amphotericin B, amphotericin B liposomal, diazepam, esomeprazole and omeprazole.
Warfarin
With the concomitant use of Tigacil® and warfarin (single dose 25 mg), a decrease in the clearance of R-warfarin and S-warfarin by 40% and 23%, and an increase in the AUC of warfarin by 68% and 29%, respectively, are observed.
The mechanism of such interaction has not yet been established. Since tigecycline can prolong both PT/INR and aPTT, when using the drug Tigacil® simultaneously with anticoagulants, it is necessary to carefully monitor the results of appropriate coagulation tests.
Warfarin does not change the pharmacokinetic profile of tigecycline.
Inhibitors or inducers of isoenzymes of the cytochrome P450 system
Tigecycline is not metabolized by isoenzymes of the cytochrome P450 system. Therefore, it is expected that active substances that inhibit or induce the activity of cytochrome P450 isoenzymes will not alter the clearance of tigecycline.
In turn, Tigacil® is unlikely to affect the metabolism of these groups of medicinal compounds.
In vitro studies have shown that tigecycline does not inhibit metabolism mediated by the following six cytochrome CYP isoenzymes: 1A2, 2C8, 2C9, 2C19, 2D6 and 3A4.
Digoxin
Tigacil® at the recommended dose does not affect the rate and extent of absorption or clearance of digoxin (0.5 mg followed by a daily dose of 0.25 mg).
Digoxin does not change the pharmacokinetic profile of tigecycline. Therefore, when using Tigacil® together with digoxin, no dose adjustment is required.
Concomitant use of P-glycoprotein inhibitors (eg, ketoconazole or cyclosporine) or P-glycoprotein inducers (eg, rifampicin) may affect the pharmacokinetics of tigecycline.
Oral contraceptives
When antibiotics are used concomitantly with oral contraceptives, the effectiveness of the contraceptives may be reduced.
In in vitro studies, antagonism was not observed between tigecycline and other commonly used classes of antibiotics.
Overdose
Overdose
Not described.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
1.5 years
Manufacturer
Manufacturer
Vayet Lederle S.r.L., Italy
Additional information
| Shelf life | 1.5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Wyeth Lederle S.r.l., Italy |
| Medication form | lyophilizate |
| Brand | Wyeth Lederle S.r.l. |
Related products
Buy Tigacil, lyophilizate 50 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.