No products in the cart.
Thyrozole,10 mg 50 pcs
€9.75 €8.53
Description
Irozole has an antithyroid effect.
Pharmacodynamics
The antithyroid drug disrupts the synthesis of thyroid hormones by blocking the enzyme peroxidase involved in thyronine iodination in the thyroid gland to form triiodine and tetraiodothyronine. This property allows for symptomatic therapy of thyrotoxicosis, except in cases of thyrotoxicosis due to release of hormones after destruction of thyroid cells (after treatment with radioactive iodine or in thyroiditis). Thyrozole does not affect the process of release of synthesized thyronines from thyroid follicles. This explains the latent period of varying duration, which may precede the normalization of plasma levels of T3 and T4, i.e. improvement of the clinical picture.
Decreases basic metabolism, accelerates iodide excretion from the thyroid gland, increases reciprocal activation of thyroid hormone synthesis and secretion by the pituitary gland, which may be accompanied by some thyroid hyperplasia.
The duration of action of a single dose is almost 24 hours.
Pharmacokinetics
Tyrosol is quickly and almost completely absorbed when taken orally. Cmax in plasma is reached within 0.4-1.2 hours. It is practically not bound to blood plasma proteins. Thyrozole cumulates in the thyroid gland, where it is slowly metabolized. Small amounts of thiamazole are detected in breast milk. T1/2 is about 3-6 hours; in hepatic insufficiency it increases. No dependence of kinetics on the functional state of the thyroid gland has been revealed. Metabolism of Thyrozole is carried out in kidneys and liver, excretion is carried out by kidneys and with bile. The kidneys excrete 70% of Thyrozole within 24 hours, and 7-12% – in unchanged form.
Indications
Indications
thyrotoxicosis;
preparation for surgical treatment of thyrotoxicosis;
preparation for treatment of thyrotoxicosis with radioactive iodine;
therapy during the latent period of radioactive iodine action (carried out before the onset of radioactive iodine action – for 4–6 months);
in exceptional cases – long-term maintenance therapy for thyrotoxicosis, when due to the general condition or for individual reasons it is impossible to perform radical treatment;
prevention of thyrotoxicosis when prescribing iodine preparations (including cases of use of iodine-containing radiocontrast agents), in the presence of latent thyrotoxicosis, autonomous adenomas or a history of thyrotoxicosis.
Pharmacological effect
Pharmacological effect
Irosol has an antithyroid effect.
Pharmacodynamics
An antithyroid drug disrupts the synthesis of thyroid hormones by blocking the enzyme peroxidase, which is involved in the iodination of thyronine in the thyroid gland with the formation of triiodo- and tetraiodothyronine. This property allows for symptomatic treatment of thyrotoxicosis, with the exception of cases of development of thyrotoxicosis due to the release of hormones after the destruction of thyroid cells (after treatment with radioactive iodine or with thyroiditis). Tyrosol does not affect the process of release of synthesized thyronines from the thyroid follicles. This explains the latent period of varying duration, which may precede the normalization of T3 and T4 levels in the blood plasma, i.e. improvement of the clinical picture.
Reduces basal metabolism, accelerates the removal of iodides from the thyroid gland, increases reciprocal activation of the synthesis and release of thyroid-stimulating hormone by the pituitary gland, which may be accompanied by some hyperplasia of the thyroid gland.
The duration of action of a single dose is almost 24 hours.
Pharmacokinetics
When taken orally, tyrosol is rapidly and almost completely absorbed. Cmax in plasma is achieved within 0.4–1.2 hours. It practically does not bind to blood plasma proteins. Tyrosol accumulates in the thyroid gland, where it is slowly metabolized. Small amounts of thiamazole are found in breast milk. T1/2 – about 3-6 hours, with liver failure it increases. No dependence of kinetics on the functional state of the thyroid gland was revealed. Metabolism of the drug Tyrosol occurs in the kidneys and liver, and the drug is excreted through the kidneys and bile. 70% of Tyrosol is excreted by the kidneys within 24 hours, with 7–12% unchanged.
Special instructions
Special instructions
For patients with a significant enlargement of the thyroid gland, narrowing the lumen of the trachea, Tyrozol is prescribed for a short time in combination with levothyroxine sodium, because with prolonged use, an increase in goiter and even greater compression of the trachea is possible. It is necessary to carefully monitor the patient (monitoring TSH levels, tracheal lumen). During treatment with the drug, regular monitoring of peripheral blood patterns is necessary.
Thiamazole and thiourea derivatives may reduce the sensitivity of thyroid tissue to radiation therapy. If during treatment with the drug a sore throat, difficulty swallowing, increased body temperature, signs of stomatitis or furunculosis (possible symptoms of agranulocytosis) suddenly appear, you should stop taking the drug and consult a doctor immediately.
If subcutaneous hemorrhages or bleeding of unknown origin, generalized skin rash and itching, persistent nausea or vomiting, jaundice, severe epigastric pain and severe weakness appear during treatment, discontinuation of the drug is required. If treatment is stopped early, a relapse of the disease is possible. The appearance or worsening of endocrine ophthalmopathy is not a side effect of treatment with Tyrozol, carried out properly. In rare cases, after completion of treatment, late hypothyroidism may occur, which is not a side effect of the drug, but is associated with inflammatory and destructive processes in the thyroid tissue that occur as part of the underlying disease.
Impact on the ability to drive vehicles and machinery. Thiamazole does not affect the ability to drive vehicles and machinery.
Active ingredient
Active ingredient
Thiamazole
Composition
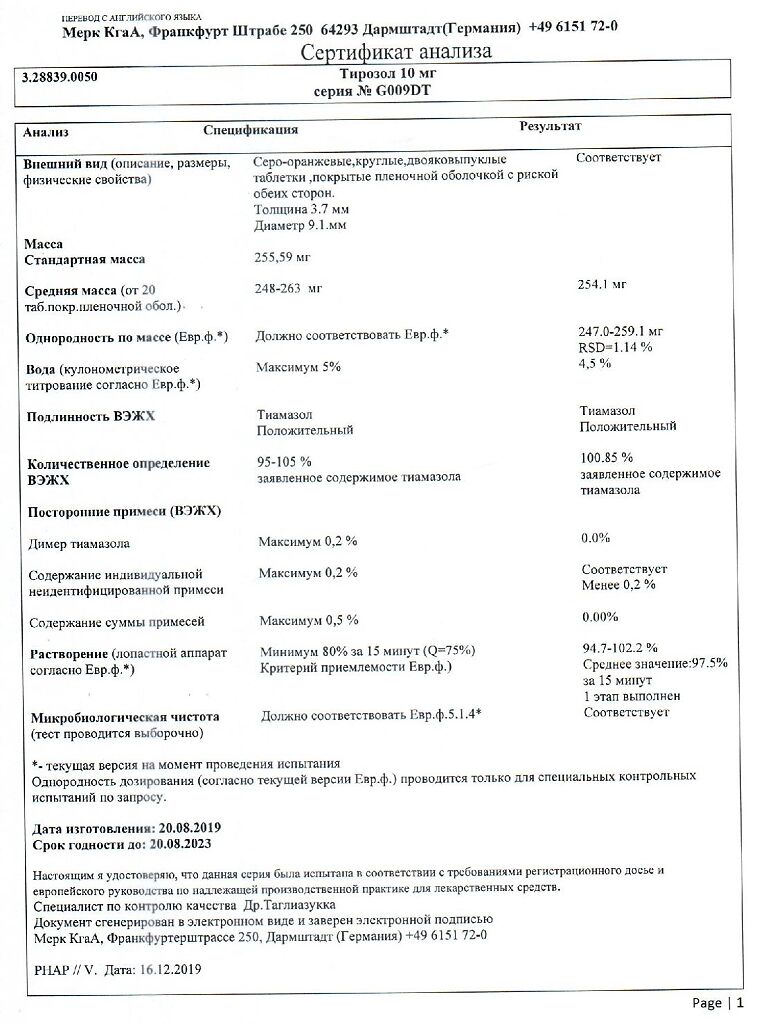
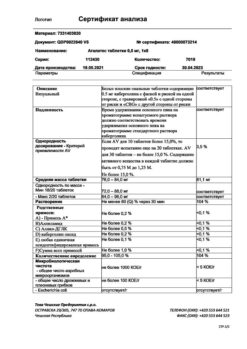
Composition
Each tablet contains:
Core:
Active ingredient: thiamazole 10 mg.
Excipients: colloidal silicon dioxide – 2 mg, sodium carboxymethyl starch – 2 mg, magnesium stearate – 2 mg, hypromellose 2910/15 – 3 mg, talc – 6 mg, cellulose powder – 10 mg, corn starch – 20 mg, lactose monohydrate – 195 mg.
Film casing:
Pregnancy
Pregnancy
Untreated hyperfunction of the thyroid gland during pregnancy can lead to serious complications such as premature birth and fetal malformations. Thiamazole penetrates the placental barrier and can reach the same concentration in the fetal blood as in the mother. Due to the fact that the effect of thiamazole on the fetus cannot be completely excluded, during pregnancy the drug should be prescribed after a full assessment of the benefits and risks of its use in the minimum effective dose without additional use of levothyroxine.
Doses of thiamazole significantly higher than recommended can cause goiter and hypothyroidism in the fetus, as well as low birth weight.
During lactation, treatment of thyrotoxicosis with Tyrozol can be continued if necessary. Since thiamazole passes into breast milk and can reach a concentration in it corresponding to its level in the mother’s blood, the newborn may develop hypothyroidism. Therefore, if it is necessary to continue treatment of thyrotoxicosis during breastfeeding, Tyrozol should be taken in low doses (up to 10 mg/day) without additional levothyroxine.
Contraindications
Contraindications
hypersensitivity to thiamazole and thiourea derivatives or any other component of the drug;
agranulocytosis during previous therapy with carbimazole or thiamazole;
granulocytopenia (including history);
cholestasis before starting treatment;
therapy with thiamazole in combination with levothyroxine sodium during pregnancy;
patients with rare hereditary diseases associated with galactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome (contains lactose);
children’s age from 0 to 3 years.
With caution: should be used in patients with very large goiters, narrowing of the trachea (only short-term treatment during preparation for surgery), and liver failure.
Side Effects
Side Effects
The frequency of side effects of the drug is assessed as follows: very frequent (≥1/10), frequent (≥1/100,
From the circulatory and lymphatic system: infrequently – agranulocytosis (its symptoms (see “Special Instructions”) may appear even weeks and months after the start of treatment and lead to the need to discontinue the drug); very rarely – generalized lymphadenopathy, thrombocytopenia, pancytopenia.
From the endocrine system: very rarely – insulin autoimmune syndrome with hypoglycemia.
From the nervous system: rarely – reversible changes in taste sensations, dizziness; very rarely – neuritis, polyneuropathy.
From the gastrointestinal tract: very rarely – enlargement of the salivary glands, vomiting.
From the liver and biliary tract: very rarely – cholestatic jaundice and toxic hepatitis.
From the skin and subcutaneous tissues: very often – allergic skin reactions (itching, redness, rash); very rarely – generalized skin rashes, alopecia, lupus-like syndrome.
From the musculoskeletal and connective tissue: often – slowly progressive arthralgia without clinical signs of arthritis.
General complications and reactions at the injection site: rarely – fever, weakness, weight gain.
Interaction
Interaction
When prescribing thiamazole after using iodine-containing radiocontrast agents in a high dose, the effect of thiamazole may be weakened.
Lack of iodine increases the effect of thiamazole.
In patients taking thiamazole for the treatment of thyrotoxicosis, after achieving a euthyroid state, i.e. normalization of the content of thyroid hormones in the blood serum, it may be necessary to reduce the doses of cardiac glycosides (digoxin and digitoxin), aminophylline, as well as increase the doses of warfarin and other anticoagulants – derivatives of coumarin and indanedione (pharmacodynamic interaction).
Lithium preparations, beta-blockers, reserpine, amiodarone increase the effect of thiamazole (dose adjustment required).
When used simultaneously with sulfonamides, metamizole sodium and myelotoxic drugs, the risk of developing leukopenia increases.
Leukogen and folic acid, when used simultaneously with thiamazole, reduce the risk of developing leukopenia.
Gentamicin enhances the antithyroid effect of thiamazole.
There is no data on the effect of other drugs on the pharmacokinetics and pharmacodynamics of the drug. However, it should be borne in mind that with thyrotoxicosis, the metabolism and elimination of substances is accelerated. Therefore, in some cases it is necessary to adjust the dose of other drugs.
Overdose
Overdose
With long-term use of high doses of the drug, the development of subclinical and clinical hypothyroidism, as well as an increase in the size of the thyroid gland due to an increase in TSH levels, is possible. This can be avoided by reducing the dose of the drug until a state of euthyroidism is achieved or, if necessary, by additionally prescribing levothyroxine sodium. As a rule, after discontinuation of the drug Tyrozol, spontaneous restoration of thyroid function is observed. Taking very high doses of thiamazole (about 120 mg per day) can lead to the development of myelotoxic effects. Such doses of the drug should be used only for special indications (severe forms of the disease, thyrotoxic crisis).
Treatment: discontinuation of the drug, gastric lavage, symptomatic therapy, if necessary, transfer to an antithyroid drug of another group.
Storage conditions
Storage conditions
In a dry place, at a temperature not exceeding 25 °C
Shelf life
Shelf life
4 years
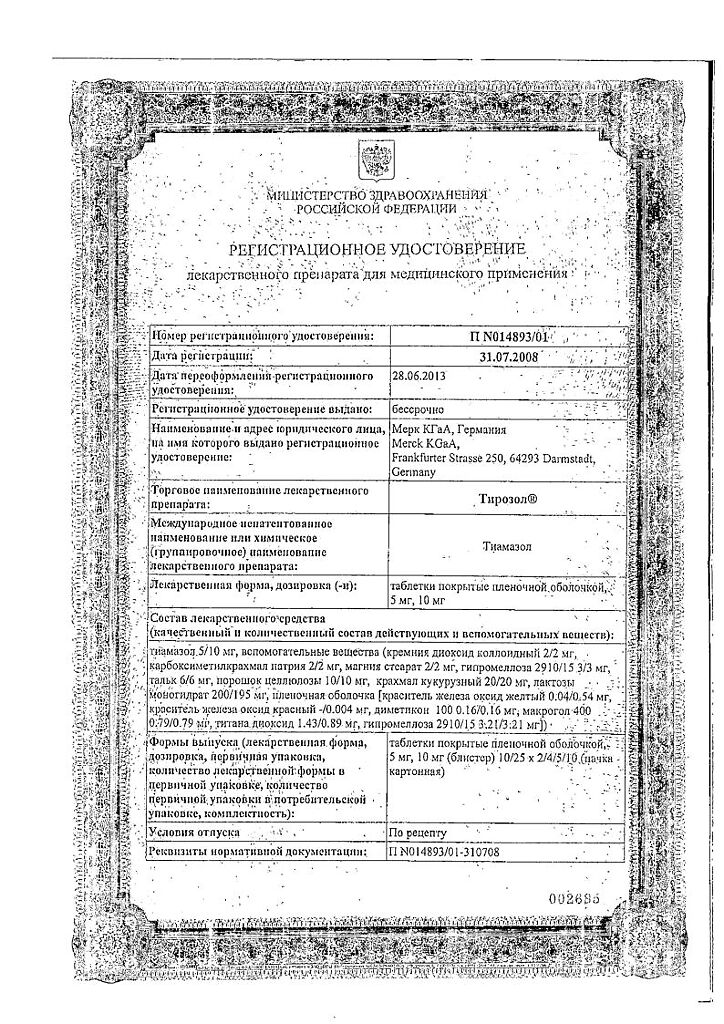
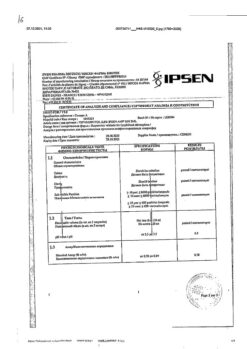
Manufacturer
Manufacturer
Merck Healthcare KGaA, Germany
Additional information
| Shelf life | 4 years |
|---|---|
| Conditions of storage | In a dry place, at a temperature not exceeding 25 °C |
| Manufacturer | Merck Healthcare KGaA, Germany |
| Medication form | pills |
| Brand | Merck Healthcare KGaA |
Related products
Buy Thyrozole,10 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.