No products in the cart.
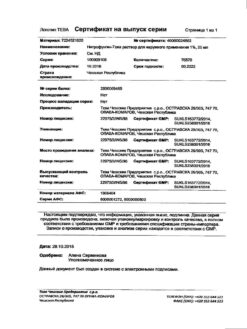
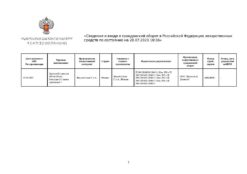
Terbinafin-Teva, tablets 250 mg 28 pcs
€30.12 €29.73
Description
Pharmacotherapeutic group: antifungal agent.
Code ATX: [D01BA02]
Pharmacological properties
Pharmacodynamics
Terbinafine belongs to the group of allilamines and has a wide spectrum of antifungal action. In low concentrations it has fungicidal activity against dermatophytes (Тгусһутон rubrum, Тгусһутон mentagrophytes, Тгусһутон tonsurans, Тгусһутон verrucosum, Тгусһутон violaceum, Microsporum canis, Epidermophyton floccosum), yeast fungi, mainly Candida albicans. Activity against yeast fungi, depending on their species, may be fungicidal or fungistatic.
Terbinafine disrupts the early stage of biosynthesis of the main component of the cell membrane of fungi (ergosterol) by inhibiting the enzyme squalene epoxidase.
In oral administration it is ineffective in the treatment of variegated herpes caused by Pityrosporum ovale, Pityrosporum orbiculare (Malassezia furfur).
Pharmacokinetics
Ingestion absorbs more than 70%. Absolute bioavailability is reduced by 40% due to the “first pass” effect. After a single oral dose of 250 mg the time to reach maximum concentration (TCmax) is about 2 hours; maximum concentration (Cmax) is 1 µg/ml. The area under the curve “concentration – time” (AUC) is 4.56 µg×h/ml; AUC increases by 20% when concomitantly taken with food. With prolonged use Cmax increases by 25%, AUC – 2.5 times. Effective elimination half-life (T1/2) is about 36 h, terminal T1/2 200-400 h (indicates prolonged excretion from skin and adipose tissue). Equilibrium concentration (Css) is independent of age. Plasma concentration of terbinafine is independent of sex.
Binding to plasma proteins is more than 99%. It is rapidly distributed in the tissues, penetrates into the dermal layer of the skin and nail plates. It penetrates into the secretion of sebaceous glands and accumulates in high concentrations in hair follicles, hair, skin and subcutaneous tissue. It is subjected to significant biotransformation, the resulting metabolites have no antifungal activity. It is excreted by the kidneys at 70%.
It does not accumulate in the body. The age of patients does not affect the pharmacokinetics of terbinafine, but elimination may be reduced with renal or hepatic damage, leading to high concentrations of terbinafine in the blood.
It is excreted with breast milk.
Indications
Indications
– Mycoses of the scalp (trichophytia, microsporia).
– Fungal diseases of the skin and nails (onychomycosis) caused by Trychophyton spp. (T. rubrum, T. mentagrophytes, T. verrucosum, T. violaceum), Microsporum spp. (M. canis, M. gypseum) and Epidermophyton floccosum.
– Severe, widespread dermatomycosis of smooth skin of the trunk and extremities, requiring systemic treatment.
– Candidiasis of the skin.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antifungal agent.
ATX code: [D01BA02]
Pharmacological properties
Pharmacodynamics
Terbinafine belongs to the group of allylamines and has a wide spectrum of antifungal action. In low concentrations, it has fungicidal activity against dermatophytes (Trychophyton rubrum, Trychophyton mentagrophytes, Trychophyton tonsurans, Trychophyton verrucosum, Trychophyton violaceum, Microsporum canis, Epidermophyton floccosum), yeast fungi, mainly Candida albicans. Activity against yeast fungi, depending on their type, can be fungicidal or fungistatic.
Terbinafine disrupts the early stage of biosynthesis of the main component of the fungal cell membrane (ergosterol) by inhibiting the enzyme squalene epoxidase.
When administered orally, it is not effective in the treatment of pityriasis versicolor caused by Pityrosporum ovale, Pityrosporum orbiculare (Malassezia furfur).
Pharmacokinetics
When taken orally, more than 70% is absorbed. Absolute bioavailability due to the “first pass” effect is reduced by 40%. After a single oral dose of 250 mg, the time to reach maximum concentration (TCmax) is about 2 hours; maximum concentration (Cmax) – 1 μg/ml. The area under the concentration-time curve (AUC) is 4.56 mcg×h/ml; when taken with food, the AUC increases by 20%. With long-term use, Cmax increases by 25%, AUC by 2.5 times. The effective half-life (T1/2) is about 36 hours, terminal T1/2 200-400 hours (indicates long-term elimination from the skin and adipose tissue). The steady-state concentration (Css) does not depend on age. The concentration of terbinafine in plasma does not depend on gender.
Communication with plasma proteins is more than 99%. It is quickly distributed in tissues, penetrates the dermal layer of the skin and nail plates. Penetrates into the secretions of the sebaceous glands and accumulates in high concentrations in the hair follicles, hair, skin and subcutaneous tissue. It undergoes significant biotransformation; the resulting metabolites do not have antifungal activity. 70% is excreted by the kidneys.
Does not accumulate in the body. The age of patients does not affect the pharmacokinetics of terbinafine, however, elimination may be reduced in case of kidney or liver damage, leading to high concentrations of terbinafine in the blood.
Excreted in breast milk.
Special instructions
Special instructions
Irregular use of terbinafine or premature cessation of treatment may lead to relapse of the disease.
If after 2 weeks of treatment of a skin infection there is no improvement in the condition, it is necessary to re-determine the causative agent of the disease and its sensitivity to the drug.
Systemic use for onychomycosis is justified only in the case of damage to the majority of nails, the presence of severe subungual hyperkeratosis, and the ineffectiveness of previous local therapy.
When treating onychomycosis, a laboratory-confirmed clinical response is usually observed several months after mycological cure and cessation of treatment, which is due to the rate of regrowth of a healthy nail. Removal of nail plates is not required when treating onychomycosis of the hands for 3 weeks and onychomycosis of the feet for 6 weeks.
In the presence of liver disease, the clearance of terbinafine may be reduced.
During treatment, it is necessary to monitor the activity of “liver” transaminases in the blood serum.
In rare cases, cholestasis and hepatitis occur after 3 months of treatment. If signs of liver dysfunction occur (weakness, persistent nausea, decreased appetite, excessive abdominal pain, jaundice, dark urine or discolored stool), the drug should be discontinued.
Prescribing terbinafine to patients with psoriasis requires caution, because in very rare cases, terbinafine can cause an exacerbation of psoriasis.
When treating with terbinafine, general hygiene rules should be observed to prevent the possibility of re-infection through underwear and shoes. During treatment (after 2 weeks) and at the end it is necessary to carry out antifungal treatment of shoes, socks and stockings.
Impact on the ability to drive vehicles and machinery
Terbinafine does not affect the ability to drive a car or operate machinery. However, it should be taken into account that dizziness may occur during treatment.
Active ingredient
Active ingredient
Terbinafine
Composition
Composition
1 tablet contains: active ingredient terbinafine hydrochloride 281.3 mg (terbinafine 250.0 mg);
excipients: microcrystalline cellulose 40.5 mg; sodium carboxymethyl starch (type A) 36.0 mg; hypromellose 7.5 mg; colloidal silicon dioxide 1.2 mg; magnesium stearate 3.5 mg
Pregnancy
Pregnancy
Taking terbinafine during pregnancy is contraindicated due to the lack of sufficient data on its safety during pregnancy. Terbinafine is excreted in breast milk, so its use is contraindicated during breastfeeding.
Contraindications
Contraindications
Hypersensitivity to the components of the drug; chronic or active liver diseases, chronic renal failure (creatinine clearance (CC) less than 50 ml/min), children under 3 years of age and weighing up to 20 kg (for this dosage form), lactation period, pregnancy.
With caution
Chronic renal failure (creatinine clearance more than 50 ml/min), alcoholism, suppression of bone marrow hematopoiesis, tumors, metabolic diseases, occlusive vascular diseases of the extremities.
Side Effects
Side Effects
The incidence of side effects is classified according to the recommendations of the World Health Organization: very often – at least 10%; often – at least 1%, but less than 10%; infrequently – not less than 0.1%, but less than 1%; rarely – not less than 0.01%, but less than 0.1%; very rare – less than 0.01%, including isolated cases.
From the digestive system: very often – a feeling of fullness in the stomach, loss of appetite, dyspepsia, nausea, abdominal pain, diarrhea; infrequently – disturbances or loss of taste (recovery occurs within a few weeks after stopping treatment), increased activity of “liver” transaminases; rarely – cholestasis, jaundice, hepatitis; in some cases – long-term disorders of taste, leading to refusal to eat and significant loss of body weight, liver failure.
From the blood and lymphatic system: very rarely – neutropenia, thrombocytopenia, agranulocytosis, lymphopenia, isolated cases of pancytopenia.
From the skin: very rarely – psoriasis-like rash, exacerbation of psoriasis, acute generalized pustular exanthema.
Allergic reactions: very often – rash, urticaria; very rarely – angioedema, malignant epidermal erythema (Stevens-Johnson syndrome), anaphylactoid reactions, toxic epidermal necrolysis (Lyell’s syndrome).
From the musculoskeletal system: very often – arthralgia, myalgia.
From the central and peripheral nervous system: often – headache; rarely – paresthesia, hypoesthesia, dizziness; very rarely – depression, anxiety.
From the organ of hearing and labyrinthine disorders: very rarely – vertigo.
Other: rarely – malaise, weakness; very rarely – systemic lupus erythematosus, including the cutaneous form.
Interaction
Interaction
Dose adjustment of terbinafine is required when used simultaneously with inhibitors and inducers of cytochrome P450 isoenzymes, which can slow down and accelerate the elimination of terbinafine from the body. Cimitidine reduces the elimination rate of terbinafine by 30%, and rifampicin increases the elimination rate of terbinafine by 100%.
In vitro and in vivo studies have shown that terbinafine, by inhibiting the CYP2P6 isoenzyme, disrupts the metabolism of tricyclic antidepressants, selective serotonin reuptake inhibitors (desipramine, fluvoxamine), beta-blockers (metoprolol, propranolol), antiarrhythmic drugs (flecainide, propafenone), monoamine oxidase B inhibitors (selegiline) and antipsychotics agents (chlorpromazine, haloperidol).
Terbinafine does not significantly affect the rate of elimination of tolbutamine, terfinadine, triazolam, and oral contraceptives that are metabolized by other cytochrome P450 isoenzymes (with the exception of the CYP2P6 isoenzyme).
Terbinafine does not affect the rate of elimination of antipyrine and digoxin.
When taking terbinafine and oral contraceptives simultaneously, menstrual irregularities may develop.
Terbinafine may enhance the effectiveness of caffeine by increasing its plasma concentration and reducing the rate of elimination from the body by 21%.
Terbinafine may reduce the elimination rate of desipramine by 82%.
Terbinafine may reduce the effectiveness of cyclosporine by reducing its plasma concentration by 15%.
When used simultaneously with warfarin, it can affect the prothrombin test indicators: blood clotting time and international normalized ratio.
When used together with ethanol or drugs that have hepatoxic effects, there is a risk of developing drug-induced liver damage.
Overdose
Overdose
Symptoms: nausea, vomiting, headache, dizziness, gastralgia, frequent urination, rash.
Treatment: gastric lavage followed by the use of activated carbon. If necessary, carry out symptomatic therapy.
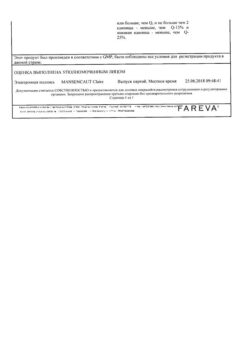
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Teva Pharmaceutical Enterprises Ltd., Israel
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Teva Pharmaceutical Enterprises Ltd, Israel |
| Medication form | pills |
| Brand | Teva Pharmaceutical Enterprises Ltd |
Related products
Buy Terbinafin-Teva, tablets 250 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.