No products in the cart.
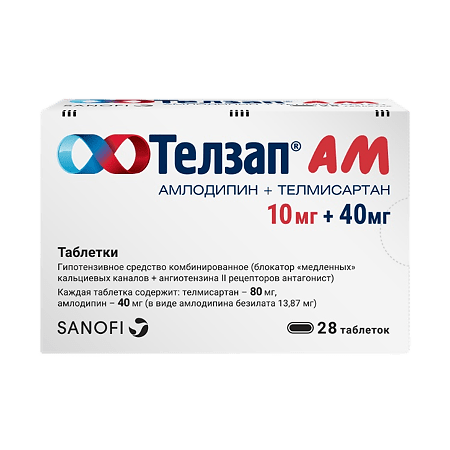
Telzap AM, tablets 10 mg+40 mg 28 pcs
€13.81 €11.51
Description
Telzap® AM contains two hypotensive agents with complementary mechanisms of action that provide blood pressure (BP) control in patients with essential hypertension; amlodipine belongs to the pharmacological group of “slow” calcium channel blockers (SCBs) and telmisartan belongs to the group of angiotensin II receptor antagonists (ARA II). The combination of these substances shows additive antihypertensive effect, causing a more pronounced BP reduction than each of the components of the drug individually.
Amlodipine
Amlodipine is a dihydropyridine derivative of BMCC class and inhibits transmembrane entry of calcium ions into cardiomyocytes and smooth muscle cells of blood vessels. The mechanism of antihypertensive action of amlodipine is associated with vasodilatory action on vascular smooth muscle. The exact mechanism by which amlodipine reduces the frequency and severity of angina attacks is not fully established, but amlodipine may reduce myocardial ischemia through the following two effects:
- amlodipine dilates peripheral arterioles and thereby reduces total peripheral vascular resistance (PPR), the so-called afterload. As heart rate (HR) when taking amlodipine practically does not increase, this reduction of heart muscle load reduces myocardial energy expenditure and myocardial oxygen demand.
- the mechanism of antianginal action of amlodipine also seems to be related to the dilation of the main coronary arteries and arterioles, both in areas of myocardium with normal blood flow and in the ischemic areas. This dilation increases myocardial oxygen delivery in patients with coronary artery spasm (in Prinzmetal or variant angina).
In patients with arterial hypertension, taking amlodipine once daily provides clinically significant reduction of BP in “lying” and “standing” position for 24 h. Orthostatic arterial hypotension is not typical during amlodipine use due to slow onset of drug action.
In patients with arterial hypertension and normal renal function amlodipine in therapeutic doses leads to decrease of renal vascular resistance, increase of glomerular filtration rate and effective renal plasma blood flow without changing filtration or proterinuria.
There have been no adverse metabolic effects or changes in plasma lipid concentrations when taking amlodipine. Amlodipine can be taken by patients with bronchial asthma, diabetes mellitus and gout. Amlodipine usage in patients with cardiac insufficiency is not accompanied with negative inotropic action (does not decrease exercise tolerance and left ventricular ejection fraction).
Telmisartan
The mechanism of action
Telmisartan is a specific ARA II (type AT1) that is effective when taken orally. Having a very high affinity for the binding center of the angiotensin II receptor subtype AT1. telmisartan displaces angiotensin II from binding to the receptor without having an agonist effect against this receptor. Telmisartan does not exhibit the properties of a partial agonist for the AT1 receptor. Telmisartan selectively binds to the AT1 receptor. Binding to the receptor is long-term.
Telmisartan shows no affinity for other receptors, including AT2 receptors and other less studied angiotensin receptors. Telmisartan reduces plasma aldosterone concentrations and does not inhibit renin or block ion channels. Telmisartan does not inhibit the activity of angiotensin-converting enzyme (ACE) (kininase II), an enzyme that also destroys bradykinin. This leads to the conclusion that the drug will not increase adverse events associated with the action of bradykinin.
The dose of telmisartan 80 mg daily will almost completely stop the increase in BP under the influence of angiotensin II.
The antihypertensive effect persists for 24 h and remains significant for 48 h.
After the first dose of telmisartan, the antihypertensive effect develops gradually over 3 h. A pronounced antihypertensive effect usually develops 4-8 weeks after regular use. The action lasts for 24 h after telmisartan administration and remains significant up to 48 h.
In patients with arterial hypertension telmisartan provides reduction of BP and BP with no effect on HR.
After abrupt withdrawal of telmisartan treatment there is a gradual (over several days) return of BP values to their values before the start of the drug without development of “withdrawal” syndrome.
The incidence of dry cough was significantly lower in patients taking telmisartan than in patients receiving ACE inhibitors. These data were obtained in clinical studies directly comparing these two types of antihypertensive therapy.
The combination of amlodipine and telmisartan, administered once daily, results in effective and sustained BP reduction within 24 hours.
Pharmacokinetics
Amlodipine
Intake
Intake
. After oral administration of amlodipine at therapeutic doses, maximum plasma concentrations are reached after 6-12 hours. Absolute bioavailability of the drug is 64-80%. Food intake has no effect on the bioavailability of amlodipine.
Distribution
The apparent volume of distribution (Vd) is approximately 21 l/kg. In vitro studies have shown that approximately 97.5% of amlodipine circulating in the blood is bound to plasma proteins.
Biotransformation
Amlodipine is largely (approximately 90%) metabolized in the liver to form inactive metabolites.
Elimation
The T1/2 of amlodipine from blood plasma is approximately 35-50 h, which confirms the possibility of its use once daily. The drug is excreted by the kidneys: 10% of the administered dose of the drug is eliminated as the parent compound and 60% as metabolites. Excretion of amlodipine from blood plasma is biphasic.
Particular patient populations
Patients with impaired hepatic function
There is very limited clinical data on the use of amlodipine in patients with impaired hepatic function. In patients with hepatic impairment, decreased clearance of amlodipine has been observed, resulting in a prolonged T1/2 and increased AUC of approximately 40-60%.
Elderly patients
The time of reaching maximum plasma concentration (tmax) of amlodipine is comparable in elderly patients and in younger patients. In elderly patients the clearance of amlodipine tends to decrease with a corresponding increase in AUC and prolongation of t1/2.
Telmisartan
Intake
Telmisartan is rapidly absorbed, but the amount absorbed may vary. The average absolute bioavailability of telmisartan is approximately 50%. When telmisartan is taken with food, there is a decrease in the area under the curve “concentration-time” (AUC) of approximately 6% (when telmisartan is taken at a dose of 40 mg per day) to 19% (at a dose of 160 mg per day). Three hours after drug administration, telmisartan plasma concentrations level off, regardless of food intake.
Distribution
Telmisartan is highly bound to plasma proteins (> 99.5%), primarily to albumin and to alpha-1-acid glycoprotein. The average apparent volume of distribution in the equilibrium state (Vdss) is approximately 500 liters.
Biotransformation
The metabolism of telmisartan consists of conjugation of the parent compound with glucuronic acid. The resulting conjugate has no pharmacological activity.
The elimination half-life (T1/2) is more than 20 hours. Maximum plasma concentration (Cmax) and, to a lesser extent, AUC increase disproportionately with increasing dose. There are no data on clinically significant accumulation of telmisartan taken at recommended doses. It is excreted unchanged in the intestine, renal excretion is less than 1%. Total plasma clearance is high (about 1000 ml/min) compared to “hepatic” blood flow (about 1500 ml/min).
Linearity/nonlinearity of pharmacokinetics
A linear relationship between the drug dose and its plasma concentration was not observed. Cmax and, to a lesser extent, AUC increase disproportionately with doses above 40 mg per day.
Particular patient populations
Patient gender
There were differences in plasma concentrations of the drug in men and women: Cmax and AUC values were approximately 3 and 2 times higher in women than in men, respectively.
Patients in the elderly
The pharmacokinetics of telmisartan did not differ between elderly patients and patients younger than 65 years of age.
Patients with renal impairment
In patients with mild, moderate and severe renal impairment, a 2-fold increase in plasma telmisartan concentrations was observed. However, in patients with renal impairment who are on hemodialysis, plasma concentrations of the drug were lower. Telmisartan is highly bound to plasma proteins and is not excreted by hemodialysis. The T1/2 was not altered in patients with impaired renal function.
Patients with impaired hepatic function
The results of pharmacokinetic studies have shown increased absolute bioavailability of telmisartan to almost 100% in patients with impaired hepatic function. The T1/2 in patients with impaired liver function was not altered.
Indications
Indications
Arterial hypertension (in patients whose blood pressure is not sufficiently controlled with telmisartan or amlodipine as monotherapy);
arterial hypertension (in patients for whom combination therapy is indicated);
arterial hypertension in patients receiving telmisartan and amlodipine as separate drugs as a replacement for this therapy.
Pharmacological effect
Pharmacological effect
The drug Telzap® AM contains two antihypertensive substances with complementary mechanisms of action that provide control of blood pressure (BP) in patients with essential arterial hypertension; amlodipine belongs to the pharmacological group of “slow” calcium channel blockers (SCBC), and telmisartan belongs to the group of angiotensin II receptor antagonists (ARA II). The combination of these substances exhibits an additive antihypertensive effect, causing a more pronounced decrease in blood pressure than each of the components of the drug individually.
Amlodipine
Amlodipine is a dihydropyridine derivative, belongs to the BMCC class, inhibits the transmembrane entry of calcium ions into cardiomyocytes and smooth muscle cells of blood vessels. The mechanism of the antihypertensive effect of amlodipine is associated with a vasodilating effect on vascular smooth muscle. The exact mechanism by which amlodipine reduces the frequency and severity of angina attacks is not fully established, but amlodipine may reduce myocardial ischemia through the following two effects:
amlodipine dilates peripheral arterioles and thereby reduces total peripheral vascular resistance (TPVR), the so-called afterload. Since the heart rate (HR) practically does not increase when taking amlodipine, this decrease in the load on the heart muscle reduces the energy consumption of the myocardium and its need for oxygen.
the mechanism of the antianginal action of amlodipine also appears to be associated with the expansion of the main coronary arteries and arterioles, both in areas of the myocardium with normal blood flow and in ischemic areas. This dilation increases oxygen delivery to the myocardium in patients with coronary artery spasm (Prinzmetal’s angina or variant angina).
In patients with arterial hypertension, taking amlodipine once a day provides a clinically significant reduction in blood pressure in the “lying” and “standing” positions within 24 hours. Orthostatic arterial hypotension is not typical during the use of amlodipine due to the slow onset of action of the drug.
In patients with arterial hypertension and normal renal function, amlodipine in therapeutic doses leads to a decrease in renal vascular resistance, an increase in glomerular filtration rate and effective plasma blood flow in the kidneys without changing filtration or proterinuria.
When taking amlodipine, no undesirable metabolic effects or changes in plasma lipid concentrations were observed. Amlodipine can be taken by patients with bronchial asthma, diabetes mellitus and gout. The use of amlodipine in patients with heart failure is not accompanied by a negative inotropic effect (exercise tolerance is not reduced, and the left ventricular ejection fraction is not reduced).
Telmisartan
Mechanism of action
Telmisartan is a specific ARA II (type AT1), effective when taken orally. Having a very high affinity for the binding site of the AT1 receptor subtype with angiotensin II. Telmisartan displaces angiotensin II from binding to the receptor without having an agonist effect on this receptor. Telmisartan does not exhibit partial AT1 receptor agonist properties. Telmisartan selectively binds to the AT1 receptor. The connection with the receptor is long-term.
Telmisartan does not show affinity for other receptors, including AT2 receptors and other less studied angiotensin receptors. Telmisartan reduces the concentration of aldosterone in the blood plasma, does not inhibit renin and does not block ion channels. Telmisartan does not inhibit the activity of angiotensin-converting enzyme (ACE) (kininase II), an enzyme that also destroys bradykinin. This allows us to conclude that the drug will not increase the adverse events associated with the action of bradykinin.
A dose of telmisartan 80 mg per day almost completely suppresses the increase in blood pressure under the influence of angiotensin II.
The antihypertensive effect lasts for 24 hours and remains significant for 48 hours.
After taking the first dose of telmisartan, the antihypertensive effect develops gradually over 3 hours. A pronounced antihypertensive effect usually develops 4-8 weeks after regular use. The effect persists for 24 hours after taking telmisartan and remains significant up to 48 hours.
In patients with arterial hypertension, telmisartan reduces SBP and DBP without affecting heart rate.
After abrupt discontinuation of treatment with telmisartan, there is a gradual (over several days) return of blood pressure values to their values before starting the drug without the development of a “withdrawal” syndrome.
In patients taking telmisartan, the incidence of dry cough was significantly lower than in patients receiving ACE inhibitors. These data were obtained from clinical studies directly comparing these two types of antihypertensive therapy.
A combined drug of amlodipine and telmisartan, used once a day, leads to an effective and sustained decrease in blood pressure within 24 hours.
Pharmacokinetics
Amlodipine
Suction
After taking amlodipine orally in therapeutic doses, maximum plasma concentrations are achieved within 6-12 hours. The absolute bioavailability of the drug is 64-80%. Food intake does not affect the bioavailability of amlodipine.
Distribution
The apparent volume of distribution (Vd) is approximately 21 l/kg. In vitro studies have shown that about 97.5% of amlodipine circulating in the blood is bound to plasma proteins.
Biotransformation
Amlodipine is largely (approximately 90%) metabolized in the liver to form inactive metabolites.
Removal
T1/2 of amlodipine from blood plasma is approximately 35-50 hours, which confirms the possibility of its use once a day. The drug is excreted by the kidneys: 10% of the administered dose of the drug is eliminated in the form of the parent compound and 60% in the form of metabolites. The elimination of amlodipine from blood plasma occurs in two phases.
Special patient populations
Patients with liver dysfunction
There is extremely limited clinical data on the use of amlodipine in patients with impaired liver function. In patients with hepatic impairment, a decrease in the clearance of amlodipine was observed, which led to a prolongation of T1/2 and an increase in AUC by approximately 40-60%.
Elderly patients
The time to reach the maximum concentration (tmax) of amlodipine in the blood plasma is comparable in elderly patients and in patients of the younger age group. In elderly patients, amlodipine clearance tends to decrease with a corresponding increase in AUC and prolongation of T1/2.
Telmisartan
Suction
Telmisartan is rapidly absorbed, but the amount of drug absorbed may vary. The average absolute bioavailability of telmisartan is approximately 50%. When taking telmisartan with food, there is a decrease in the area under the concentration-time curve (AUC) from approximately 6% (when taking telmisartan at a dose of 40 mg per day) to 19% (at a dose of 160 mg per day). 3 hours after taking the drug, the concentration of telmisartan in the blood plasma levels off, regardless of food intake.
Distribution
Telmisartan is characterized by a high degree of binding to plasma proteins (> 99.5%), mainly to albumin and alpha-1-acid glycoprotein. The average apparent volume of distribution at steady state (Vdss) is approximately 500 L.
Biotransformation
The metabolism of telmisartan involves the conjugation of the parent compound with glucuronic acid. The resulting conjugate has no pharmacological activity.
Removal
The half-life (T1/2) is more than 20 hours. The maximum plasma concentration (Cmax) and, to a lesser extent, AUC increase disproportionately with increasing dose. There are no data on clinically significant accumulation of telmisartan taken at recommended doses. Excreted through the intestines unchanged, excretion by the kidneys is less than 1%. The total plasma clearance is high (about 1000 ml/min) compared to the “hepatic” blood flow (about 1500 ml/min).
Linearity/nonlinearity of pharmacokinetics
There was no linear relationship between the dose of the drug and its plasma concentration. Cmax and, to a lesser extent, AUC increase disproportionately with doses above 40 mg per day.
Special patient populations
Patient gender
Differences in drug concentrations in blood plasma were identified between men and women: Cmax and AUC in women were approximately 3 and 2 times higher than in men, respectively.
Elderly patients
The pharmacokinetics of telmisartan did not differ between elderly patients and patients under the age of 65 years.
Patients with impaired renal function
In patients with mild, moderate and severe renal impairment, a 2-fold increase in telmisartan plasma concentrations was observed. However, in patients with renal failure on hemodialysis, plasma concentrations of the drug were lower. Telmisartan is characterized by a high degree of binding to plasma proteins and is not excreted from the body through hemodialysis. T1/2 did not change in patients with impaired renal function.
Patients with liver dysfunction
The results of pharmacokinetic studies showed an increase in the absolute bioavailability of telmisartan to almost 100% in patients with impaired liver function. T1/2 in patients with impaired liver function did not change.
Special instructions
Special instructions
Amlodipine
Patients with chronic heart failure
In a long-term placebo-controlled study (PRAISE-2) in patients with NYHA functional class III-IV CHF of non-ischemic etiology, the use of amlodipine was associated with an increase in reports of pulmonary edema, despite the lack of a significant difference in the incidence of progression of heart failure compared with placebo.
BMCC should be used with caution, incl. amlodipine in patients with CHF due to the possible risk of other cardiovascular complications and mortality.
Liver dysfunction
As with other BMCCs, T1/2 of amlodipine increases in patients with impaired liver function. Therefore, Telzap AM should be used with caution in such patients, and the dose of telmisartan should not exceed 40 mg once daily. Telzap AM is contraindicated in patients with severe liver dysfunction.
Renal dysfunction
In patients with impaired renal function, amlodipine can be used in normal doses. Changes in amlodipine plasma concentrations did not correlate with the severity of renal dysfunction. Amlodipine is not excreted from the body during dialysis.
Elderly patients
No dose adjustment of Telzap AM is required in elderly patients. Increasing the dose should be done with caution.
Children
The safety and effectiveness of Telzap AM in children have not yet been established.
Sorbitol
This medicinal product contains sorbitol (E 420). In patients with rare hereditary fructose intolerance, the use of Telzap AM is contraindicated.
Telmisartan
Liver dysfunction
The use of the combination of amlodipine + telmisartan is contraindicated in patients with cholestasis, biliary obstruction and/or severe liver dysfunction, since telmisartan is mainly excreted in the bile. There is reason to believe that the hepatic clearance of telmisartan is reduced in these patients. The drug should be used with caution in patients with mild to moderate liver dysfunction.
Renovascular hypertension
When treated with drugs acting on the RAAS, in patients with bilateral renal artery stenosis or stenosis of the artery of a single functioning kidney, the risk of a significant decrease in blood pressure and the development of acute renal failure increases.
Renal dysfunction and kidney transplantation
When using telmisartan in patients with impaired renal function, it is recommended to periodically monitor the content of potassium and creatinine in the blood plasma. There is no experience with the use of the drug in patients who shortly before use underwent a kidney transplant. Telmisartan is not eliminated by dialysis.
Decrease in circulating blood volume (CBV)
Decreased blood pressure. especially after the first dose of Telzap AM, may occur in patients with reduced blood volume and/or low sodium content in the blood plasma due to previous treatment with diuretics, restriction of salt intake, diarrhea or vomiting. Such conditions (fluid and/or sodium deficiency) must be eliminated before starting to take Telzap® AM.
Double blockade of the RAAS
Data on the simultaneous use of ACE inhibitors with ARB II or with drugs containing aliskiren confirm an increased risk of a sharp decrease in blood pressure, the development of hyperkalemia and decreased renal function (including acute renal failure).
The simultaneous use of ARA II with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m² body surface area) and is not recommended in other patients. If it is necessary to carry out double blockade of the RAAS, each case should be considered individually and carefully monitor renal function, water and electrolyte balance and blood pressure levels.
Concomitant use of ARB II with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Against the background of RAAS blockade, cases of arterial hypotension, fainting, hyperkalemia and renal dysfunction (including the development of acute renal failure) have been reported in predisposed patients, especially when taking drugs that act on the RAAS simultaneously.
In this regard, double blockade of the RAAS (in particular, with simultaneous use of telmisartan with other RAAS blockers) is not recommended. If simultaneous use of several RAAS blockers is necessary, renal function should be carefully monitored.
Other conditions associated with stimulation of the RAAS
In patients whose vascular tone and renal function depend primarily on the activity of the RAAS (for example, patients with severe chronic heart failure or existing kidney disease, including renal artery stenosis), the use of drugs acting on this system, such as telmisartan. associated with the occurrence of an acute decrease in blood pressure, hyperazotemia, oliguria, or rarely with the development of acute renal failure.
Primary hyperaldosteronism
In patients with primary hyperaldosteronism, treatment with antihypertensive drugs that act by inhibiting the RAAS is usually ineffective. In this regard, the use of Telzap AM is not recommended.
Aortic or mitral valve stenosis, obstructive hypertrophic cardiomyopathy
As with other vasodilators, patients with aortic or mitral stenosis, as well as hypertrophic obstructive cardiomyopathy, should be especially careful.
Patients with diabetes mellitus receiving insulin or other hypoglycemic drugs
In patients with diabetes mellitus taking insulin or other hypoglycemic drugs, the use of telmisartan may lead to the development of hypoglycemia and should be accompanied by monitoring of blood glucose levels. If necessary, the dose of insulin or other hypoglycemic drugs should be adjusted.
Hyperkalemia
Like other drugs acting on the RAAS, the use of telmisartan may contribute to the development of hyperkalemia.
In elderly patients, patients with renal failure or diabetes mellitus, as well as in patients who are simultaneously treated with other drugs that increase the content of potassium in the blood plasma, or have concomitant pathological conditions, hyperkalemia can be fatal.
When using drugs that act on the RAAS simultaneously, the benefit-risk ratio should be carefully assessed.
Major risk factors for developing hyperkalemia include:
• diabetes mellitus, renal impairment, old age (patients over 70 years old);
• simultaneous use with drugs acting on the RAAS and/or supplements containing potassium.
Medicines that can cause hyperkalemia. are potassium-containing salt substitutes, potassium-sparing diuretics, ACE inhibitors, ARB II, NSAIDs, including selective COX-2 inhibitors, heparin, immunosuppressants (cyclosporine and tacrolimus) and trimethoprim.
• concomitant diseases, especially dehydration, acute heart failure, metabolic acidosis, acute renal failure (for example, in infectious diseases), cytolysis syndrome (for example, acute limb ischemia, rhabdomyolysis, major trauma).
Patients at risk are advised to carefully monitor plasma potassium levels.
Ethnic differences
Like all other II receptor antagonists, telmisartan is less effective in lowering blood pressure in black patients than in other races, possibly due to a greater predisposition to decreased renin activity in these patient populations.
Coronary heart disease and cerebrovascular disease
As with any other antihypertensive drugs, an excessive decrease in blood pressure in patients with coronary heart disease or cerebrovascular disease can lead to the development of myocardial infarction or stroke.
Impact on the ability to drive vehicles and machinery
The drug Telzap® AM has a moderate effect on the ability to drive vehicles and control moving mechanisms. Due to the possible development of dizziness, headache, increased fatigue, nausea when taking the drug, caution should be exercised when driving vehicles and engaging in other activities that require concentration and speed of psychomotor functions.
If the described adverse reactions occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Amlodipine, Telmisartan
Composition
Composition
1 tablet 10 mg + 40 mg contains:
active ingredients:
amlodipine – 10,000 mg (as amlodipine besylate – 13,870 mg),
telmisartan – 40,000 mg;
excipients:
sorbitol,
sodium hydroxide,
povidone K25,
microcrystalline cellulose,
calcium hydrogen phosphate dihydrate,
meglumine,
magnesium stearate.
Contraindications
Contraindications
Hypersensitivity to active, excipients and other dihydropyridine derivatives;
pregnancy;
breastfeeding period;
obstructive diseases of the biliary tract;
severe arterial hypotension;
obstruction of the left ventricular outflow tract (including a high degree of aortic stenosis);
hemodynamically unstable heart failure after acute myocardial infarction;
severe liver dysfunction;
shock (including cardiogenic);
simultaneous use with aliskiren or drugs containing aliskiren in patients with diabetes mellitus and/or moderate or severe renal impairment (glomerular filtration rate (GFR) less than 60 ml/min/1.73 m² body surface area);
simultaneous use with ACE inhibitors in patients with diabetic nephropathy;
fructose intolerance and glucose/galactose malabsorption syndrome or sucrase/isomaltase deficiency;
age under 18 years (efficacy and safety have not been established).
With caution
Bilateral renal artery stenosis or stenosis of the artery of a single functioning kidney;
unstable angina, acute myocardial infarction (no data on use in the acute period and within one month after myocardial infarction);
impaired renal function and condition after kidney transplantation;
liver dysfunction; Recommendations regarding the dosage regimen in patients with impaired liver function have not been developed, so caution should be used in such clinical cases;
a decrease in circulating blood volume (CBV) due to previous use of diuretics, limiting the consumption of table salt, diarrhea or vomiting;
diabetes mellitus;
hyponatremia;
hyperkalemia;
aortic or mitral valve stenosis;
primary hyperaldosteronism (efficacy and safety have not been established);
age over 70 years;
coronary heart disease and/or clinically significant cerebral atherosclerosis (with an excessive decrease in blood pressure, there is a risk of increased ischemic disorders, including the development of acute myocardial infarction and/or stroke);
sick sinus syndrome (severe bradycardia, tachycardia);
chronic heart failure (CHF) of non-ischemic etiology, functional class III-IV according to the NYHA classification;
hypertrophic obstructive cardiomyopathy.
Side Effects
Side Effects
The incidence of adverse reactions was determined according to the World Health Organization (WHO) classification: very common (≥1/10); often (≥1/100 and <1/10); uncommon (≥1/1000 and <1/100); rare (≥1/10000 and <1/1000); very rare (< 1/10000), frequency unknown (cannot be calculated based on available data).
Potential adverse reactions during treatment with Telzap® AM include all adverse reactions that were previously reported during the use of individual components of the drug.
Adverse reactions expected based on experience with telmisartan
Serious adverse reactions include anaphylactic reactions and angioedema (incidence “rare”), and acute renal failure.
In controlled clinical trials in patients with arterial hypertension, the overall incidence of adverse reactions in the telmisartan group was generally similar to that in the placebo group (41.4% and 43.9%, respectively). The incidence of adverse reactions did not depend on the dose of the drug, nor on the gender, age or race of the patients.
The safety profile of telmisartan in patients receiving the drug to reduce cardiovascular morbidity was similar to that in patients with arterial hypertension.
The adverse reactions listed below were reported in controlled clinical trials in patients with arterial hypertension or were identified in the analysis of reports received in the post-marketing period.
This list also includes serious and non-serious adverse reactions that caused treatment discontinuation in three long-term clinical studies involving 21,642 patients receiving telmisartan to reduce cardiovascular morbidity over a period of up to 6 years.
Infectious and parasitic diseases: uncommon – urinary tract infections (including cystitis), upper respiratory tract infections (including pharyngitis and sinusitis); rarely – sepsis (including death).
Disorders of the blood and lymphatic system: infrequently – anemia; rarely – eosinophilia, thrombocytopenia.
Immune system disorders: rarely – anaphylactic reactions, hypersensitivity reactions.
Metabolic and nutritional disorders: infrequently – hyperkalemia; rarely – hypoglycemia (in patients with diabetes mellitus).
Mental disorders: infrequently – insomnia, depression; rarely – anxiety.
Nervous system disorders: infrequently – fainting; rarely – drowsiness.
Visual disorders: rarely – visual disturbances.
Hearing and labyrinthine disorders: uncommon – vertigo.
Cardiac disorders: uncommon – bradycardia; rarely – tachycardia.
Vascular disorders: uncommon – decreased blood pressure, orthostatic hypotension.
Disorders of the respiratory system, chest and mediastinal organs: infrequently – shortness of breath, cough; very rarely – interstitial lung disease.
Gastrointestinal disorders: uncommon – abdominal pain, diarrhea, dyspepsia, bloating, vomiting; rarely – dry mouth, discomfort in the stomach.
Disorders of the liver and biliary tract: rarely – liver dysfunction/liver damage.
Disorders of the skin and subcutaneous tissues: infrequently – itching, increased sweating, skin rash; rarely – angioedema (including fatal), eczema, erythema, urticaria, drug rash, toxicoderma.
Musculoskeletal and connective tissue disorders: uncommon – back pain (eg, sciatica), muscle spasms, myalgia; rarely – arthralgia, pain in the limbs, pain in the tendons (symptoms resembling tendinitis).
Renal and urinary tract disorders: uncommon – renal dysfunction, including acute renal failure.
General disorders and disorders at the injection site: infrequently – chest pain, asthenic syndrome (general weakness); rarely – influenza-like syndrome.
Laboratory and instrumental data: infrequently – increased concentration of creatinine in blood plasma; rarely – a decrease in the concentration of hemoglobin in the blood plasma, an increase in the concentration of uric acid in the blood plasma, an increase in the activity of liver enzymes, an increase in the concentration of creatine phosphokinase in the blood plasma.
Description of selected adverse reactions
Sepsis
In a clinical study, the incidence of sepsis in the telmisartan group was higher than in the placebo group. This may be regarded as an incidental finding or as a development of a phenomenon associated with a currently unknown mechanism.
Decreased blood pressure
This adverse reaction has often been reported in patients with controlled blood pressure while using telmisartan in combination with standard therapy to reduce cardiovascular morbidity.
Liver dysfunction/liver damage
The largest number of cases of liver dysfunction or liver damage was identified in the analysis of post-marketing case reports in patients of the Japanese ethnic group. Patients of this ethnic group are susceptible to the development of adverse reactions of this type.
Interstitial lung disease
During the post-marketing period, there have been reports of cases of interstitial lung disease that were temporarily associated with telmisartan. However, a cause-and-effect relationship between the use of telmisartan and the development of this disease has not been established.
Adverse reactions expected based on experience with amlodipine
The most common adverse reactions associated with the use of amlodipine include drowsiness, dizziness, headache, palpitations, a feeling of a “rush” of blood to the skin, abdominal pain, nausea, swelling of the ankles and other localizations, fatigue.
Disorders of the blood and lymphatic system: very rarely – leukopenia, thrombocytopenia.
Immune system disorders: very rarely – allergic reactions.
Metabolic and nutritional disorders: uncommon – weight loss, weight gain; very rarely – hyperglycemia.
Mental disorders: infrequently – insomnia, mood changes (including anxiety), depression: rarely – confusion.
Nervous system disorders: often – drowsiness, dizziness, headache (especially at the beginning of treatment); uncommon – tremor, dysgeusia, syncope, hypoesthesia, paresthesia; very rarely – hypertonicity, peripheral neuropathy; frequency unknown – extrapyramidal disorders.
Visual disorders: often – visual disturbances (including diplopia).
Hearing and labyrinthine disorders: uncommon – tinnitus.
Cardiac disorders: often – palpitations; uncommon – arrhythmia (including bradycardia, ventricular tachycardia and atrial fibrillation); very rarely – myocardial infarction.
Vascular disorders: often – a feeling of a “rush” of blood to the skin; infrequently – decreased blood pressure; very rarely – vasculitis.
Disorders of the respiratory system, chest and mediastinal organs: often – shortness of breath; infrequently – cough, rhinitis.
Gastrointestinal disorders: often – abdominal pain, nausea, irregular bowel movements (including diarrhea and constipation); uncommon – vomiting, dry oral mucosa; very rarely – pancreatitis, gastritis, gum hyperplasia.
Disorders of the liver and biliary tract: very rarely – hepatitis, jaundice, increased activity of liver enzymes (in most cases in combination with cholestasis).
Disorders of the skin and subcutaneous tissues: often – swelling of the ankles and feet; uncommon – alopecia, purpura, changes in skin pigmentation (appearance of discolored areas of the skin), increased sweating, itching, skin rash, exanthema, urticaria; very rarely – angioedema, erythema multiforme, exfoliative dermatitis, Stevens Johnson syndrome, photosensitivity; frequency unknown – toxic epidermal necrolysis.
Musculoskeletal and connective tissue disorders: often – muscle spasms; uncommon – arthralgia, myalgia, back pain.
Renal and urinary tract disorders: uncommon – frequent urination, dysuria, nocturia.
Disorders of the genital organs and breast: uncommon – erectile dysfunction, gynecomastia.
General disorders and disorders at the injection site: very often – swelling; often – increased fatigue, asthenic syndrome; uncommon – chest pain, pain, general malaise.
Adverse reactions expected based on experience with amlodipine and telmisartan
Infectious and parasitic diseases: rarely – cystitis.
Mental disorders: rarely – anxiety, insomnia, depression.
Nervous system disorders: often – dizziness, infrequently – drowsiness, migraine, headache, paresthesia; rarely – fainting, peripheral neuropathy, hypoesthesia, dysgeusia, tremor.
Hearing and labyrinthine disorders: uncommon – vertigo.
Cardiac disorders: uncommon – bradycardia, palpitations.
Vascular disorders: uncommon – hypotension, orthostatic hypotension, hot flashes.
Disorders of the respiratory system of the chest and mediastinum: infrequently – cough; very rarely – interstitial lung disease.
Gastrointestinal disorders: uncommon – abdominal pain, diarrhea, nausea; rarely – vomiting, gum hypertrophy, shortness of breath, dry mouth.
Disorders of the skin and subcutaneous tissues: infrequently – itching of the skin; rarely – eczema, erythema.
Musculoskeletal and connective tissue disorders: uncommon – arthralgia, muscle spasms (calf muscle cramps), myalgia; rarely – back pain, pain in the lower extremities (legs).
Urinary tract disorders: rarely – nocturia.
Disorders of the genital organs and breast: uncommon – erectile dysfunction.
General disorders and disorders at the injection site: often – peripheral edema; uncommon – asthenia, chest pain, fatigue, swelling.
Laboratory and instrumental data: infrequently – increased concentration of “liver” transaminases; rarely – increased concentration of uric acid in the blood.
Additional information regarding the combination of amlodipine and telmisartan:
Peripheral edema, a dose-related side effect of amlodipine, was observed in patients receiving the combination of amlodipine and telmisartan less frequently than in patients receiving amlodipine alone.
Interaction
Interaction
There were no interactions between the two active ingredients included in this drug in fixed doses in clinical studies.
No studies have been conducted to study drug interactions between Telzap® AM and other drugs.
Interaction with amlodipine
The influence of other drugs on the pharmacological properties of amlodipine
CYP3A4 isoenzyme inhibitors
Concomitant use of amlodipine with strong or moderate inhibitors of the CYP3A4 isoenzyme (HIV protease inhibitors, azole antifungals, macrolides, such as erythromycin or clarithromycin, as well as verapamil or diltiazem) may be accompanied by a significant increase in systemic exposure to amlodipine. As a result, the risk of a sharp decrease in blood pressure increases.
Clinical manifestations of these options for simultaneous use may be more pronounced in elderly patients; medical supervision is necessary for possible dose adjustment of the drugs.
Inducers of the CYP3A4 isoenzyme
With simultaneous use of inducers of the CYP3A4 isoenzyme, the concentration of amlodipine may vary. It is necessary to monitor blood pressure, and consider adjusting the dose of amlodipine during and after concomitant use, especially with strong inducers of the CYP3A4 isoenzyme (for example, rifampicin and St. John’s wort preparations).
Grapefruits and grapefruit juice
The use of amlodipine while drinking grapefruits or grapefruit juice is not recommended, as in some patients this may lead to an increase in the bioavailability of the drug and, accordingly, an increase in the antihypertensive effect.
Dantrolene (in the form of infusions)
In animals receiving verapamil in combination with intravenous dantrolene, the development of lethal ventricular fibrillation and cardiovascular collapse associated with hyperkalemia was observed. Due to the risk of hyperkalemia, it is recommended to avoid the use of BMCC. such as amlodipine, concomitantly with dantrolene in patients susceptible to developing malignant hyperthermia, as well as for the treatment of this condition.
The effect of amlodipine on the pharmacological properties of other drugs
Amlodipine enhances the effect of other antihypertensive drugs.
Atorvastatin, digoxin and warfarin
In clinical drug interaction studies, amlodipine had no effect on the pharmacokinetics of atorvastatin, digoxin and warfarin.
Cyclosporine
Interaction studies between cyclosporine and amlodipine have not been conducted in healthy volunteers or in any population other than renal transplant patients.
These patients showed an increase in residual concentrations of cyclosporine in the blood plasma (on average by 0-40%).
In patients receiving amlodipine in combination with cyclosporine after kidney transplantation, it is recommended to monitor cyclosporine concentrations and, if necessary, reduce its dose.
Simvastatin
With the simultaneous use of multiple doses of amlodipine 10 mg and simvastatin 80 mg 1 time per day, the systemic exposure of simvastatin was 77% higher than with simvastatin monotherapy. In patients taking amlodipine. The dose of simvastatin should not exceed 20 mg per day.
Tacrolimus
The combined use of tacrolimus with amlodipine is characterized by a risk of increasing the concentration of tacrolimus in the blood plasma. Patients taking amlodipine should monitor tacrolimus plasma concentrations and adjust the dose if necessary to avoid tacrolimus toxicity.
Other drugs
The safety of combined use of amlodipine with thiazide diuretics, beta-blockers, and ACE inhibitors has been established. long-acting nitrates. nitroglycerin (applied sublingually), non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics and oral hypoglycemic agents. With the simultaneous use of amlodipine and sildenafil, it was shown that each of the drugs had an independent hypotensive effect.
Interaction with telmisartan
Digoxin
With simultaneous use of telmisartan and digoxin, an increase in the median Cmax of digoxin by 49% and its residual concentration by 20% was observed. At the initial stages of taking digoxin, as well as when adjusting its dose and discontinuing treatment, it is necessary to monitor drug concentrations in the body to maintain them within the therapeutic range.
Drugs whose simultaneous use is not recommended
Potassium-sparing diuretics and potassium-containing nutritional supplements
II ARAs, such as telmisartan, reduce potassium losses caused by the action of diuretics. Potassium-sparing diuretics, in particular spironolactone, eplerenone, triamterene and amiloride. and potassium-containing food supplements or salt substitutes can cause a significant increase in potassium levels in the blood plasma.
In cases where the simultaneous use of these drugs with telmisartan is required to eliminate confirmed hypokalemia, treatment should be carried out with caution and subject to regular monitoring of potassium levels in the blood plasma.
Lithium preparations
Concomitant use of lithium preparations and ACE inhibitors or ARB II, including telmisartan. was accompanied by cases of reversible increases in plasma lithium concentrations and symptoms of toxicity. If the simultaneous use of telmisartan with a lithium drug is necessary, it is recommended to carry out enhanced monitoring of the concentration of lithium in the blood plasma.
Drugs whose simultaneous use requires caution
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs (acetylsalicylic acid in doses that provide anti-inflammatory effects, cyclooxygenase-2 (COX-2) inhibitors and non-selective NSAIDs) may weaken the antihypertensive effect of ARA II. In some patients with impaired renal function (in particular, in patients with dehydration or in elderly patients with reduced renal function), the simultaneous use of ARB II and drugs that suppress COX-2 may lead to worsening impaired renal function, and in some cases to acute renal failure, which is usually reversible.
In this regard, treatment with these drug combinations requires caution, especially in elderly patients. The patient must be adequately hydrated. Monitoring renal function is recommended before starting a combination of drugs and regularly during treatment.
Ramipril
During a clinical study with the simultaneous use of telmisartan and ramipril, an increase in AUC0-24 and Cmax of ramipril and ramiprilat was observed up to 2.5 times. The clinical significance of this observation is unclear.
Diuretics (thiazide and loop)
Previous treatment with high doses of diuretics, such as furosemide (loop diuretic) and hydrochlorothiazide (thiazide diuretic), as well as restriction of salt intake, diarrhea or vomiting may lead to a decrease in blood volume and increase the risk of an excessive decrease in blood pressure during the initial phase of telmisartan therapy.
Drugs whose simultaneous use requires increased attention
Other antihypertensive drugs
The effect of telmisartan may be enhanced by concomitant use of other antihypertensive drugs.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
Clinical studies have shown that achieving double blockade of the RAAS with the combined use of ACE inhibitors, ARB II or aliskiren was associated with an increased incidence of adverse events such as a decrease in blood pressure. hyperkalemia and impaired renal function (including acute renal failure), compared with monotherapy with a drug acting on the RAAS.
The simultaneous use of a combination of amlodipine and telmisartan with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m² body surface area) and is not recommended in other patients.
The simultaneous use of a combination of amlodipine and telmisartan with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Baclofen and amifostine
Given the pharmacological properties of some drugs (in particular, baclofen and amifostine), it can be predicted that they will potentiate the effect of all antihypertensive drugs, including telmisartan.
Alcohol, barbiturates, narcotics and antidepressants
The risk of developing orthostatic hypotension may increase with alcohol consumption, as well as the use of barbiturates, narcotic drugs or antidepressants.
Glucocorticoids (for systemic use)
Weakening the antihypertensive effect of telmisartan.
Overdose
Overdose
Symptoms
Cases of overdose of the combination amlodipine + telmisartan have not been recorded. Possible symptoms of overdose consist of symptoms from individual components of the drug.
An overdose of amlodipine can lead to excessive peripheral vasodilation and reflex tachycardia. The development of a pronounced and persistent decrease in blood pressure has been reported, incl. with the development of shock and death. The most pronounced symptoms of telmisartan overdose were decreased blood pressure and tachycardia. Clinical manifestations such as bradycardia, dizziness, increased plasma creatinine concentrations and acute renal failure were also recorded.
Treatment
The patient should be under close clinical supervision. Treatment should include symptomatic and supportive therapy. The range of treatment measures depends on the length of time since taking the drug and the severity of symptoms. Recommended measures include inducing vomiting and/or gastric lavage and taking activated charcoal.
The concentration of electrolytes and creatinine in the blood plasma should be regularly monitored. If blood pressure decreases, the patient should be placed in a supine position with the lower limbs elevated, and the administration of saline and other plasma-substituting solutions to replenish the blood volume should immediately begin.
Restoration of vascular tone and normalization of blood pressure can be achieved by administering vasoconstrictor drugs, provided there are no contraindications to their use. Intravenous administration of calcium gluconate may provide relief of symptoms associated with calcium channel blockade.
Amlodipine and telmisartan are practically not excreted from the body through hemodialysis.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C in the original packaging (blister in a cardboard box).
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Zentiva k.s., Czech Republic
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 ° C in the original package (blister in carton pack). Keep out of reach of children. |
| Manufacturer | Zentiva k.s., Czech Republic |
| Medication form | pills |
| Brand | Zentiva k.s. |
Other forms…
Related products
Buy Telzap AM, tablets 10 mg+40 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.