No products in the cart.
Tavanic, 500 mg 10 pcs
€18.01 €15.01
Description
Infectious diseases, Sinusitis, Prostatitis, Respiratory tract infections, Inflammation of the female genitalia, Tuberculosis, Lung inflammation (pneumonia), Skin infections, Guaymorrhitis, Bronchitis, Urinary tract infections
Levofloxacin for oral and IV administration is indicated for treatment of infections and inflammatory diseases caused by agents sensitive to levofloxacin, in adults, including: Community-acquired pneumonia; uncomplicated urinary tract infections; complicated urinary tract infections (including pyelonephritis); chronic bacterial prostatitis; skin and soft tissue infections; in complex therapy of drug-resistant forms of tuberculosis; prevention and treatment of anthrax with airborne infection; acute sinusitis (tablets); exacerbation of chronic bronchitis (tablets); hospital pneumonia (for dosage of 750 mg tablets).
When using levofloxacin, official national recommendations for the appropriate use of antibacterial agents as well as the sensitivity of pathogens in a particular country should be considered (see “Special Instructions”).
Levofloxacin 0.5% eye drops are indicated for the treatment of superficial bacterial eye infections caused by susceptible microorganisms in adults and children over 1 year of age; for prevention of complications after ocular surgery and laser operations.
Indications
Indications
Levofloxacin for oral and intravenous administration is indicated for the treatment of infectious and inflammatory diseases caused by pathogens sensitive to levofloxacin in adults, including: community-acquired pneumonia; uncomplicated urinary tract infections; complicated urinary tract infections (including pyelonephritis); chronic bacterial prostatitis; infections of the skin and soft tissues; as part of complex therapy of drug-resistant forms of tuberculosis; prevention and treatment of anthrax during airborne infection; acute sinusitis (tablets); exacerbation of chronic bronchitis (tablets); hospital pneumonia (for a dosage of 750 mg tablets).
When using levofloxacin, official national recommendations for the proper use of antibacterial agents, as well as the sensitivity of pathogenic microorganisms in a particular country, should be taken into account (see “Special Instructions”).
Levofloxacin 0.5% eye drops is indicated for the treatment of superficial bacterial eye infections caused by susceptible microorganisms in adults and children over 1 year of age; for the prevention of complications after surgical and laser operations on the eye.
Pharmacological effect
Pharmacological effect
Pharmacological group: Quinolones/fluoroquinolones
Special instructions
Special instructions
Tendinopathy and tendon rupture
Fluoroquinolones, including levofloxacin, are associated with an increased risk of tendinitis and tendon rupture at any age. This side effect most commonly affects the Achilles tendon, and if the Achilles tendon ruptures, surgery may be required. Tendinitis and rupture of the rotator cuff tendon, hand, biceps, thumb, and other tendons have also been reported. The risk of developing fluoroquinolone-associated tendonitis and tendon rupture increases in older patients, usually over 60 years of age, in patients taking corticosteroids, and in patients with kidney, heart, or lung transplants. Factors in addition to age and corticosteroid use that may independently increase the risk of tendon rupture include increased physical activity, kidney failure, and pre-existing conditions such as rheumatoid arthritis. Tendinitis and tendon rupture have been reported in patients taking fluoroquinolones who did not have the above risk factors. Tendon rupture may occur during or after completion of therapy; some cases have been reported up to several months after completion of treatment. If pain, swelling, inflammation or tendon rupture occurs, levofloxacin therapy should be discontinued. Patients should be advised to rest and avoid strenuous activity at the first signs of tendinitis or tendon rupture, and to consult their physician for the prescription of other non-quinolone antimicrobial drugs.
Exacerbation of pseudoparalytic myasthenia gravis (myasthenia gravis)
Fluoroquinolones, including levofloxacin, have neuromuscular blocking activity and may increase muscle weakness in patients with myasthenia gravis. In post-marketing experience, serious adverse reactions, including pulmonary failure requiring mechanical ventilation and death, have been associated with the use of fluoroquinolones in patients with myasthenia gravis. The use of levofloxacin in patients with an established diagnosis of pseudoparalytic myasthenia gravis is contraindicated (see “Contraindications”, “Side effects”).
Hypersensitivity reactions
Severe and fatal hypersensitivity reactions and/or anaphylactic reactions have been reported while taking fluoroquinolones, incl. levofloxacin, often developing after the first dose. Some reactions were accompanied by cardiovascular collapse, hypotension, shock, convulsions, loss of consciousness, tingling sensation, angioedema (including tongue, pharynx, glottis or facial swelling), airway obstruction (bronchospasm, shortness of breath, acute respiratory distress syndrome), shortness of breath, urticaria, pruritus and other severe skin symptoms. reactions. At the first manifestations of skin rash or other hypersensitivity reactions, levofloxacin should be discontinued immediately. Serious acute hypersensitivity reactions may require administration of epinephrine and other resuscitation measures, including oxygen, IV fluids, antihistamines, corticosteroids, pressor amines, and airway management (as clinically indicated) (see Adverse Reactions).
Other serious and sometimes fatal reactions
Rarely, other severe and sometimes fatal reactions have been reported in patients taking fluoroquinolones, incl. levofloxacin, due to both hypersensitivity reactions and unknown causes. These reactions occurred predominantly after repeated doses and included the following: fever, rash or severe dermatological reactions (eg acute epidermal necrolysis, Stevens-Johnson syndrome), vasculitis, arthralgia, myalgia, serum sickness, hypersensitivity pneumonitis, interstitial nephritis, acute renal failure, hepatitis, jaundice, acute liver necrosis or liver failure, anemia (in including hemolytic and hypoplastic), thrombocytopenia (including thrombocytopenic purpura), leukopenia, agranulocytosis, pancytopenia and/or other blood changes.
At the first manifestations of skin rash, jaundice or any other manifestations of hypersensitivity, levofloxacin should be immediately discontinued and the necessary measures taken.
Hepatotoxicity
There was no evidence of severe levofloxacin-associated hepatotoxicity in clinical studies of more than 7000 patients. Severe hepatotoxic reactions recorded in post-marketing surveillance (including acute hepatitis and fatal outcome) usually occurred within the first 14 days of treatment, most cases within 6 days, and most cases of severe hepatotoxicity were not associated with hypersensitivity. The most common cases of fatal hepatotoxicity were observed in patients aged 65 years and older and were not associated with hypersensitivity. Levofloxacin should be discontinued immediately if the patient develops signs and symptoms of hepatitis (see Side Effects).
Effect on the central nervous system
The occurrence of seizures, toxic psychoses, increased intracranial pressure (including pseudotumor cerebri) has been reported in patients receiving fluoroquinolones, incl. Levofloxacin. Fluoroquinolones can also cause stimulation of the central nervous system with the appearance of tremor, restlessness, anxiety, dizziness, confusion, hallucinations, paranoia, depression, insomnia, nightmares, and rarely, suicidal thoughts and actions; these phenomena may occur after taking the first dose. If these reactions are observed in patients receiving levofloxacin, treatment should be discontinued and appropriate measures taken. As with other fluoroquinolones, levofloxacin should be used with caution in patients with known or suspected central nervous system diseases that predispose them to the development of seizures or a decreased seizure threshold (e.g., severe cerebral arteriosclerosis, epilepsy), or in the presence of other risk factors that may predispose to seizures or a decreased seizure threshold (e.g., certain drugs, renal dysfunction) (see “Side Effects”). actions”, “interaction”).
Diarrhea associated with Clostridium difficile
Clostridium difficile-associated diarrhea has been reported with almost all antibacterial agents, including levofloxacin, and can range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents leads to modification of the normal flora of the large intestine and increased growth of C. difficile. C. difficile strains that produce toxins A and B, which cause diarrhea, are associated with an increased risk of mortality because these infections may be resistant to antimicrobial therapy and may require colectomy. The possibility of C. difficile-associated diarrhea should be considered in all patients who complain of diarrhea after using antibacterial agents. A thorough medical history is necessary, because the development of C. difficile-associated diarrhea is possible within two months after the use of antibacterial drugs. If C. difficile-associated diarrhea is suspected or confirmed, discontinue levofloxacin and initiate appropriate treatment (including fluids and electrolytes, protein supplements, antibiotics to which C. difficile strains are susceptible), and surgical evaluation if clinically indicated (see Adverse Reactions).
Peripheral neuropathy
Cases of sensory or sensorimotor axonal polyneuropathy, manifested by paresthesia, hypoesthesia, dysesthesia and weakness, have been reported in patients receiving fluoroquinolones, including levofloxacin. Symptoms may occur soon after starting levofloxacin therapy and may be irreversible. The use of levofloxacin should be discontinued immediately if the patient develops symptoms of neuropathy, which include pain, burning, tingling, numbness and/or weakness or other sensory disturbances, including disturbances of touch, pain, pyrexia, loss of position sense, changes in vibration sensitivity (see “Side Effects”).
QT prolongation
Against the background of the use of fluoroquinolones, incl. levofloxacin, there was an increase in the QT interval on the ECG and infrequent cases of arrhythmia. In post-marketing studies, rare cases of torsade de pointes have been reported in patients receiving fluoroquinolones, including levofloxacin. The use of levofloxacin should be avoided if the patient has risk factors for QT interval prolongation, such as a history of QT interval prolongation, uncorrected hypokalemia, concomitant use with class IA (quinidine, procainamide) and class III antiarrhythmic drugs (amiodarone, sotalol). Elderly patients may be more sensitive to drug-associated effects on the QT interval.
Changes in blood glucose levels
As with other fluoroquinolones, changes in blood glucose levels, including symptomatic hyper- and hypoglycemia, have been reported, most cases observed in diabetic patients concomitantly receiving oral hypoglycemic agents (eg glibenclamide) or insulin. Close monitoring of blood glucose levels in these patients is recommended. If a hypoglycemic reaction develops against the background of levofloxacin, levofloxacin should be immediately discontinued and appropriate therapy should be started (see “Side effects”, “Interaction”).
Photosensitivity/phototoxicity
Patients exposed to direct sunlight or UV irradiation during treatment with fluoroquinolones may experience moderate to severe photosensitivity/phototoxicity reactions, the latter of which may manifest as excessive tanning reactions (e.g., burning, erythema, exudation, blistering, blistering, swelling) in areas exposed to direct sunlight (typically the face, décolleté of the neck, extensor surfaces forearms, backs of hands). Therefore, excessive exposure to these light sources should be avoided. Drug therapy should be discontinued if photosensitivity/phototoxicity reactions develop (see “Side Effects”).
Application in geriatrics
In the phase III clinical trial, 1945 patients receiving levofloxacin were aged ≥65 years (26%). Of these, 1081 patients (14%) were aged 65 to 74 years and 864 patients (12%) were aged ≥75 years. There were no differences in safety and effectiveness between these patients and younger patients, but greater sensitivity in some older people cannot be ruled out.
The patient should be warned:
– about the advisability of drinking plenty of water;
– that levofloxacin can cause neurological side effects (for example, dizziness of varying severity), in this regard, the patient should know how he reacts to levofloxacin before engaging in activities that require quick reactions and associated with increased concentration;
– during treatment, strong solar or artificial ultraviolet irradiation should be avoided; If phototoxic reactions (for example, skin rash) occur, treatment should be stopped.
During treatment with levofloxacin in the form of 0.5% eye drops, wearing soft contact lenses is not recommended.
Special instructions
The prevalence of acquired resistance in cultured strains of microorganisms may vary by geographic region and over time. Therefore, country-specific information on levofloxacin resistance is required.
Before starting therapy, appropriate tests should be performed to identify the causative agent of the disease and assess sensitivity to levofloxacin. Treatment with levofloxacin may be started pending the results of these tests. Once test results are obtained, appropriate therapy should be selected. Culture testing carried out periodically during levofloxacin therapy provides information about the continued sensitivity of the pathogenic microorganism to levofloxacin and the possible emergence of bacterial resistance.
Active ingredient
Active ingredient
Levofloxacin
Composition
Composition
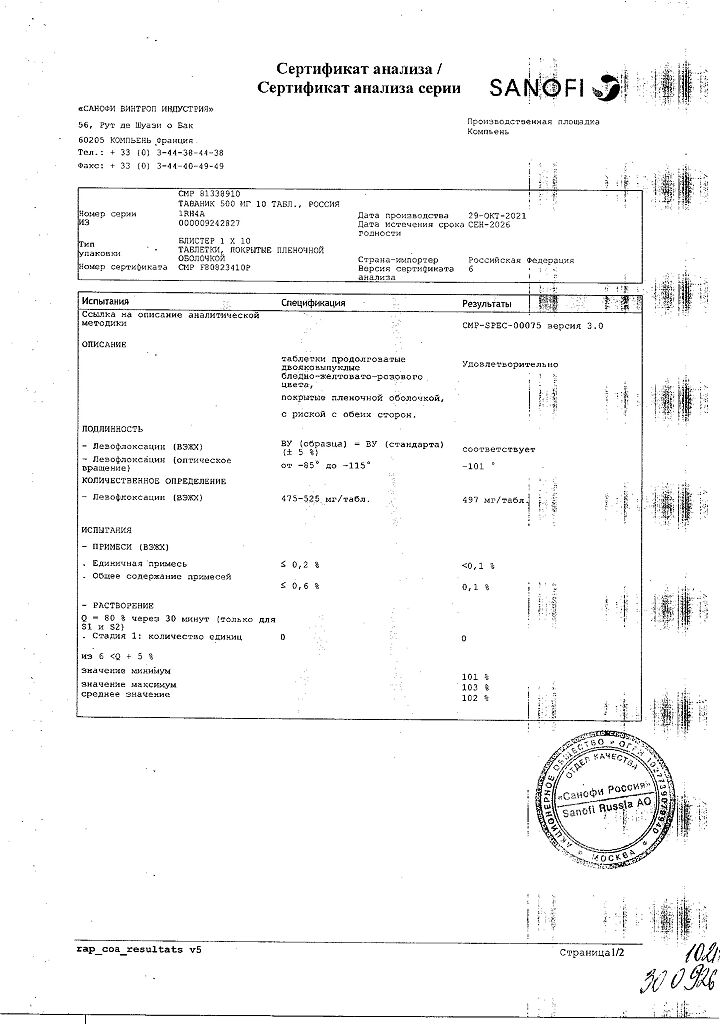
1 tablet contains:
Active ingredient:
levofloxacin 500 mg;
Excipients:
crospovidone;
methylhydroxypropylcellulose;
MCC;
sodium stearyl fumarate;
macrogol 8000;
talc;
titanium dioxide (E171);
iron oxide red (E172);
iron oxide yellow (E172).
Pregnancy
Pregnancy
Use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus (adequate, strictly controlled studies of the safety of use in pregnant women have not been conducted).
Levofloxacin did not have a teratogenic effect in rats when administered orally at a dose of 810 mg/kg/day (9.4 times the MRDC in terms of body surface area) or intravenously administered at a dose of 160 mg/kg/day (1.9 times the MRDC in terms of body surface area). Oral administration to pregnant rats at a dose of 810 mg/kg/day led to an increase in the frequency of intrauterine death and a decrease in fetal body weight. In experiments on rabbits, no teratogenic effect was detected with oral administration at a dose of 50 mg/kg/day (1.1 times the MRDC in terms of body surface area) or intravenous administration at a dose of 25 mg/kg/day, which corresponds to 0.5 MRDC in terms of body surface area.
FDA category of effect on the fetus is C.
Given the results of studies with other fluoroquinolones and the very limited data regarding levofloxacin, it can be assumed that levofloxacin may pass into the breast milk of nursing women. Due to the potential for serious adverse reactions in breastfed infants, nursing women should discontinue either breastfeeding or systemic use of levofloxacin (given the importance of the drug to the mother).
Caution must be exercised when using levofloxacin eye drops.
Contraindications
Contraindications
For systemic use: hypersensitivity to levofloxacin or other quinolones; epilepsy; pseudoparalytic myasthenia gravis (myasthenia gravis) (see “Side effects”, “Precautions”); history of tendon damage when taking fluoroquinolones; childhood and adolescence up to 18 years of age (due to incomplete growth of the skeleton, since the risk of damage to cartilaginous growth points cannot be completely excluded); pregnancy (the risk of damage to cartilaginous growth points in the fetus cannot be completely excluded); period of breastfeeding (the risk of damage to the cartilaginous growth points of bones in a child cannot be completely eliminated).
Eye drops: hypersensitivity to levofloxacin or other quinolones.
Restrictions on use
For systemic use:
– in patients predisposed to the development of seizures (in patients with previous lesions of the central nervous system, in patients simultaneously taking drugs that reduce the threshold of convulsive readiness of the brain, such as fenbufen, theophylline) (see “Interaction”);
– in patients with latent or manifest deficiency of glucose-6-phosphate dehydrogenase (increased risk of hemolytic reactions when treated with quinolones);
– in patients with impaired renal function (mandatory monitoring of renal function is required, as well as correction of the dosage regimen);
– in patients with known risk factors for QT interval prolongation: advanced age; female gender, uncorrected electrolyte disturbances (hypokalemia, hypomagnesemia); congenital long QT syndrome; heart disease (heart failure, myocardial infarction, bradycardia); simultaneous use of drugs that can prolong the QT interval (antiarrhythmic drugs of class IA and III, tricyclic antidepressants, macrolides, antipsychotics) (see “Overdose”, “Interaction”, “Precautions”);
– in patients with diabetes mellitus receiving treatment with oral hypoglycemic drugs, such as glibenclamide or insulin preparations (the risk of hypoglycemia increases);
– in patients with severe adverse reactions to other fluoroquinolones, such as severe neurological reactions (increased risk of similar adverse reactions when using levofloxacin);
– in patients with psychosis or in patients with a history of mental illness (see “Precautions”).
Eye drops: children (safety and effectiveness have not been determined).
Side Effects
Side Effects
Serious and clinically important adverse drug reactions that are discussed in more detail in the Precautions section include:
– influence on tendons;
– exacerbation of pseudoparalytic myasthenia gravis (myasthenia gravis);
– hypersensitivity reactions;
– other serious and sometimes fatal reactions;
– hepatotoxicity;
– effect on the central nervous system;
– Clostridium difficile-associated diarrhea;
– peripheral neuropathy, which may be irreversible;
– prolongation of the QT interval;
– fluctuations in blood glucose levels;
– photosensitivity/phototoxicity;
– development of drug resistance in bacteria.
Hypotension has been associated with rapid or intravenous bolus administration of levofloxacin. Levofloxacin should be administered slowly over 60 to 90 minutes.
Crystalluria and cylindruria have been reported with fluoroquinolones, including levofloxacin. Therefore, during treatment with levofloxacin, it is necessary to maintain adequate hydration in patients to avoid the formation of excessively concentrated urine.
Clinical research experience
Because clinical trials are conducted with a different set of conditions, the incidence of adverse reactions observed in these studies cannot be directly compared with the incidence of other clinical trials and cannot predict the occurrence of adverse effects in clinical practice.
Data from 29 pooled phase 3 clinical trials (n=7537) are presented. The average age of patients is 50 years (approximately 74% of patients are younger than 65 years), 50% are male, 71% are Caucasian, and 19% are black. Patients received levofloxacin for the treatment of various infections at a dose of 750 mg once daily, 250 mg once daily, or 500 mg twice daily. The duration of therapy was usually 3–14 days (average 10 days).
The overall incidence, type, and distribution of adverse reactions were similar in patients receiving levofloxacin 750 mg once daily compared with patients receiving 250 mg once daily or 500 mg twice daily. Therapy was discontinued due to drug-related adverse events in 4.3% of patients overall, 3.8% of patients taking the 250 and 500 mg doses, and 5.4% of patients taking the 750 mg dose. The most common side effects leading to discontinuation of the drug at doses of 250 and 500 mg were gastrointestinal complaints (1.4%), nausea (0.6%), vomiting (0.4%), dizziness (0.3%), headache (0.2%). The most common side effects leading to discontinuation of the drug at a dose of 750 mg were gastrointestinal disturbances (1.2%), nausea (0.6%), vomiting (0.5%), dizziness (0.3%), headache (0.3%).
The following are side effects noted in clinical trials and observed with a frequency of >0.1% in patients receiving levofloxacin (N=7537). The most common adverse reactions (≥3%) were nausea, headache, diarrhea, insomnia, constipation and dizziness.
From the nervous system and sensory organs: headache (6%), dizziness (3%), insomnia1 (4%); 0.1–1% – anxiety, agitation, confusion, depression, hallucinations, nightmares1, sleep disturbance1, anorexia, unusual dreams1, tremors, convulsions, paresthesia, vertigo, hypertension, hyperkinesis, impaired coordination of movements, drowsiness1, fainting.
From the cardiovascular system and blood: 0.1–1% – anemia, arrhythmia, palpitations, cardiac arrest, supraventricular tachycardia, phlebitis, epistaxis, thrombocytopenia, granulocytopenia.
From the respiratory system: shortness of breath (1%).
From the gastrointestinal tract: nausea (7%), diarrhea (5%), constipation (3%), abdominal pain (2%), dyspepsia (2%), vomiting (2%); 0.1–1% – gastritis, stomatitis, pancreatitis, esophagitis, gastroenteritis, glossitis, pseudomembranous colitis, liver dysfunction, increased levels of liver enzymes, increased alkaline phosphatase.
From the genitourinary system: vaginitis2 (1%); 0.1–1%: impaired renal function, acute renal failure, genital candidiasis.
From the musculoskeletal system: 0.1–1% – arthralgia, tendinitis, myalgia, pain in skeletal muscles.
From the skin: rash (2%), itching (1%); 0.1–1% – allergic reactions, edema (1%), urticaria.
Other: candidiasis (1%), reaction at the IV injection site (1%), chest pain (1%); 0.1–1%: hyperglycemia/hypoglycemia, hyperkalemia.
In repeated-dose clinical trials, ophthalmic abnormalities, including cataracts and multiple focal lens opacities, were observed in patients treated with fluoroquinolones, including levofloxacin. The relationship between these phenomena and drug intake has not been established.
1 N=7274.
2 N=3758 (women).
Post-marketing studies
It is impossible to reliably assess the frequency of development of these phenomena and the cause-and-effect relationship with taking drugs, since the reports were received spontaneously, from a population of unknown size.
From the nervous system and sensory organs: isolated reports of encephalopathy, EEG abnormalities, peripheral neuropathy (may be irreversible), psychosis, paranoia, isolated reports of suicide attempts and suicidal thoughts, uveitis, visual impairment (including diplopia, decreased visual acuity, blurred vision, scotoma), hearing loss, tinnitus, parosmia, anosmia, loss taste sensations, taste perversion, dysphonia, exacerbation of myasthenia gravis, pseudotumor of the brain.
From the cardiovascular system and blood: isolated reports of torsade de pointes, prolongation of the QT interval, tachycardia, vasodilation, increased INR, prolongation of PT, pancytopenia, aplastic anemia, leukopenia, hemolytic anemia, eosinophilia.
From the gastrointestinal tract: liver failure (including fatal cases), hepatitis, jaundice.
From the musculoskeletal system: tendon rupture, muscle damage, including rupture, rhabdomyolysis.
From the skin: bullous rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, photosensitivity/phototoxicity reactions.
Allergic reactions: hypersensitivity reactions (sometimes fatal), incl. anaphylactic/anaphylactoid reactions, anaphylactic shock, angioedema, serum sickness; isolated reports of allergic pneumonitis.
Other: leukocytoclastic vasculitis, increased activity of muscle enzymes, hyperthermia, multiorgan failure, interstitial nephritis.
When using levofloxacin in the form of 0.5% eye drops, the most frequently observed effects were: 1-3% – transient decreased vision, transient burning, pain or discomfort in the eye, sensation of a foreign body in the eye, fever, headache, pharyngitis, photophobia; <1% - allergic reactions, swelling of the eyelids, dry eyes, itching in the eye.
Interaction
Interaction
Chelated compounds: antacids, sucralfate, metal cations, multivitamins
Levofloxacin for oral administration. Magnesium- and aluminum-containing antacids, sucralfate; Drugs containing metal cations (such as iron), zinc-containing multivitamins, didanosine (dose containing aluminum and magnesium) when taken orally simultaneously with levofloxacin can significantly affect the absorption of the latter in the gastrointestinal tract, leading to a decrease in its systemic level. The above drugs must be taken at least 2 hours before or 2 hours after oral administration of devofloxacin.
Levofloxacin for injection. There are no data regarding the interactions of IV fluoroquinolones with oral antacids, sucralfate, multivitamins, didanosine, or metal cations. However, none of the fluoroquinolones should be administered, incl. levofloxacin, together with any solution containing polyvalent cations, such as magnesium, through the same system for intravenous administration.
Warfarin
In a clinical study in healthy volunteers, there was no significant effect of levofloxacin on Cmax, AUC and other pharmacokinetic parameters of the R- or S-isomers of warfarin. There was also no apparent effect of warfarin on the absorption and other pharmacokinetic parameters of levofloxacin. However, post-marketing studies have reported cases of increased effect of warfarin when used concomitantly with levofloxacin, with an increase in PT accompanied by episodes of bleeding. When levofloxacin and warfarin are used simultaneously, careful monitoring of INR, PT and other coagulation parameters is required, as well as monitoring for possible signs of bleeding.
Antidiabetic drugs
Fluctuations in blood glucose levels, including hyperglycemia and hypoglycemia, have been reported in patients receiving fluoroquinolones and antidiabetic drugs concomitantly. Careful monitoring of blood glucose levels is recommended when these drugs are used together.
NSAIDs
Concomitant use of NSAIDs with fluoroquinolones, including levofloxacin, may increase the risk of CNS stimulation and seizures.
Theophylline
In a clinical study in healthy volunteers, there was no significant effect of levofloxacin on plasma concentrations, AUC and other pharmacokinetic parameters of theophylline. There was also no visible effect of theophylline on the absorption and other pharmacokinetic parameters of levofloxacin. However, concomitant use of theophylline with other fluoroquinolones was accompanied by an increase in T1/2 and serum concentrations of theophylline and a subsequent increase in the risk of theophylline-related adverse reactions. In this regard, careful monitoring of theophylline levels and appropriate dose adjustment are necessary during concomitant use of levofloxacin. Adverse reactions, incl. convulsions may occur regardless of an increase in serum theophylline concentration.
Cyclosporine
In a study in healthy volunteers, no clinically significant effects of levofloxacin on plasma concentrations, AUC, or other pharmacokinetic parameters of cyclosporine were observed. However, increased plasma levels of cyclosporine have been reported with other fluoroquinolones. The Cmax of levofloxacin was slightly lower, whereas the Tmax and T1/2 were slightly longer in the presence of cyclosporine than those observed in other studies without concomitant treatment. The differences, however, are not considered clinically significant. In this regard, dose adjustment of levofloxacin or cyclosporine is not required when used simultaneously.
Digoxin
In a clinical study involving healthy volunteers, no significant effect of levofloxacin on Cmax, AUC and other pharmacokinetic parameters of digoxin was found. Absorption and other pharmacokinetic parameters of levofloxacin were similar in the presence or absence of digoxin. Therefore, no dose adjustment of levofloxacin or digoxin is required when used concomitantly.
Probenecid and cimetidine
In a clinical study in healthy volunteers, no significant effect of probenecid or cimetidine on the Cmax of levofloxacin was observed. AUC and T1/2 values of levofloxacin were higher, while clearance values were lower during concomitant treatment of levofloxacin with probenecid or cimetidine compared with treatment with levofloxacin alone. However, these changes are not a basis for adjusting the dose of levofloxacin when used in combination with probenecid or cimetidine.
Interactions related to laboratory or diagnostic testing
Some fluoroquinolones, including levofloxacin, may cause false-positive urine opiate test results when using commercially available immunoassay kits (more specific methods for opiate detection may be needed).
Overdose
Overdose
In mice, rats, dogs and monkeys, after administration of a single high dose of levofloxacin, the following symptoms were observed: ataxia, ptosis, decreased locomotor activity, shortness of breath, prostration, tremor, convulsions. Doses exceeding 1500 mg/kg PO and 250 mg/kg IV significantly increased mortality in rodents.
Treatment of acute overdose: gastric lavage, adequate hydration. Not excreted by hemodialysis and peritoneal dialysis.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
5 years
Manufacturer
Manufacturer
Opella Healthcare International CAC, France
Additional information
| Shelf life | 5 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Opella Healthcare International SAS, France |
| Medication form | pills |
| Brand | Opella Healthcare International SAS |
Other forms…
Related products
Buy Tavanic, 500 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.