No products in the cart.
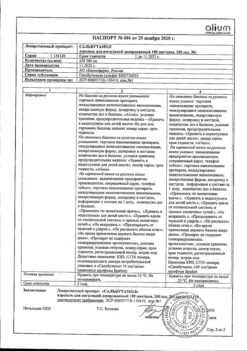
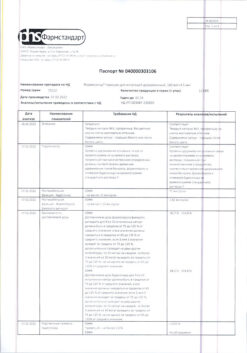
Symbicort Rapihaler, aerosol 80 mcg+4, 5 mcg/dose 120 doses
€65.63 €54.69
Description
Pharmacotherapeutic group: bronchodilator combined (beta2-adrenomimetic selective + local glucocorticosteroid)
ATX code: R03AK07
Pharmacological properties
Pharmacodynamics
Simbicort® contains budesonide and formoterol, which have different mechanisms of action and have an additive effect in reducing the frequency of exacerbations of bronchial asthma. The special properties of budesonide and formoterol make it possible to use their combination to relieve attacks/symptoms with an anti-inflammatory effect, or as maintenance therapy for bronchial asthma.
Budesonide. Budesonide is a glucocorticosteroid that has a rapid (within hours) and dose-dependent anti-inflammatory effect on the airways after inhalation, reducing the severity of symptoms and the frequency of exacerbations of bronchial asthma. When prescribing inhaled budesonide, there is a lower incidence of serious adverse effects than when using systemic glucocorticosteroids. It reduces the severity of bronchial mucosal edema, mucus production, sputum formation and airway hyperresponsiveness. The exact mechanism of anti-inflammatory action of glucocorticosteroids is unknown.
Formoterol. Formoterol is a selective b2-adrenoreceptor agonist, after inhalation of which there is rapid and prolonged relaxation of bronchial smooth muscle in patients with reversible airway obstruction. The dose-dependent bronchodilator effect occurs within 1-3 minutes after inhalation and persists for at least 12 hours after a single dose.
Symbicort® Turbuhaler®: Budesonide + Formoterol Bronchial asthma
Clinical effectiveness of Symbicort® as an anti-inflammatory attack/symptom therapy: For anti-inflammatory seizure/symptom control (therapy A) and as maintenance therapy and for anti-inflammatory seizure/symptom control (therapy B)
. A total of 7 double-blind clinical trials enrolled 20140 patients with bronchial asthma, 7831 of whom were randomized to therapy with Symbicort® for attack/symptom control with anti-inflammatory effects and with or without maintenance therapy (therapy B) (therapy A).
In two studies (SYGMA 1 and SYGMA 2) involving 8064 patients with mild bronchial asthma, 3384 patients received Symbicort® for attack/symptom control with anti-inflammatory action (therapy A) for 12 months.
In the SYGMA 2 study, Symbicort® 160/4.5 mcg when used on-demand in response to symptoms (for attack/symptom management with anti-inflammatory action – therapy A) was comparable to maintenance dose budesonide (1 inhaled 200 mcg/dose twice daily) combined with a short-acting beta2-adrenomimetic on demand with respect to the frequency of severe exacerbations. Prevention of severe exacerbations was achieved with a 75% reduction in median steroid load and without the need for adherence to maintenance therapy with inhaled glucocorticosteroids. In the SYGMA 1 trial, Symbicort® for anti-inflammatory attack/symptoms provided a statistically significant and clinically meaningful 64% reduction in the annual incidence of severe exacerbations compared to on-demand use of a short-acting beta2-adrenomimetic. The reduction in the annual incidence of moderate to severe exacerbations was 60%.
. In the SYGMA 1 study, Symbicort® 160/4.5 mcg on-demand was superior to short-acting beta2-adrenomimetic on-demand with respect to bronchial asthma symptom control, showing an average of 34.4% and 31.1% of weeks with good bronchial asthma control, respectively, but was less effective compared with maintenance dose budesonide (1 inhaled 200 mcg/dose twice daily) in combination with an on-demand short-acting beta2-adrenomimetic, with a mean of 34.4% and 44.4% weeks with good bronchial asthma control, respectively. Symbicort® for anti-inflammatory attack/symptoms was superior to the on-demand short-acting beta2-adrenomimetic in terms of improved bronchial asthma control (based on results from the Asthma Control Assessment Questionnaire of 5 items (ACQ5)). Improvement in disease control was less pronounced with Symbicort® on-demand versus maintenance dose budesonide (1 inhaled 200 mcg/dose twice daily) in combination with an on-demand short-acting beta2-adrenomimetic. The mean difference in effect of ACQ5 therapy was not clinically significant in both comparisons (assessed by a difference of 0.5 or more). These results were observed in a clinical trial setting with significantly higher adherence to budesonide maintenance therapy than in actual practice.
In the SYGMA trials, improvement in pulmonary function relative to baseline (mean prebronchodilator BEP1) was statistically significantly greater in patients receiving Symbicort® for anti-inflammatory seizure/symptoms compared with patients receiving an on-demand beta2-adrenomimetic short-acting. Statistically significantly less improvement in lung function was noted with Symbicort® on-demand compared with budesonide maintenance dose (1 inhaled 200 mcg/dose twice daily) in combination with a short-acting beta2-adrenomimetic on-demand. For both comparisons, the mean differences in therapy effect were small (approximately 30 to 55 mL, corresponding to approximately 2% of the baseline mean).
. In another clinical program involving 12076 patients in 5 studies, an observational study of 4447 patients treated with Symbicort® as maintenance therapy and for seizure/symptom control with anti-inflammatory action (therapy B) for 6 to 12 months There was a statistically and clinically significant reduction in the number of severe exacerbations and an increase in the time to first exacerbation compared to the combination of Symbicort® or budesonide as maintenance therapy and a beta2-adrenoceptor for seizure control. There was also effective control of disease symptoms, pulmonary function, and a reduction in the frequency of prescription of inhalation for seizure control. No development of tolerance to prescribed therapy was detected.
The results of 6 double-blind studies with 14385 patients with bronchial asthma (including 1847 adolescents) demonstrated comparable efficacy and safety of the drug in adolescent and adult patients. The number of adolescent patients taking more than 8 inhalations for at least one day as maintenance therapy and to control attacks/symptoms with anti-inflammatory effects was limited, and use in this regimen was infrequent.
In patients who sought care for an acute asthma attack, Symptom Control (relief of bronchospasm) was as rapid and effective after inhalation of Symbicort® as after prescription of salbutamol and formoterol.
Clinical efficacy of Symbicort® as maintenance therapy (therapy C)
Indications
Indications
80/4.5 mcg/dose
Bronchial asthma, to achieve overall disease control, including prevention and relief of symptoms, and reducing the risk of exacerbations.
160/4.5 mcg/dose
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: combined bronchodilator (selective beta2-adrenergic agonist + local glucocorticosteroid)
ATX code: R03AK07
Pharmacological properties
Pharmacodynamics
Special instructions
Special instructions
Dosage Directions
If the symptoms of bronchial asthma are controllable, the dose of Symbicort® Turbuhaler® can be gradually reduced, and it is important to constantly monitor the patient’s condition. The lowest effective dose of Symbicort® Turbuhaler® should be prescribed (see section “Dosage and Administration”).
Patients are recommended to always carry emergency medications or Symbicort® Turbuhaler® (for patients with bronchial asthma using Symbicort® Turbuhaler® for the relief of attacks/symptoms with anti-inflammatory effects – therapy A or B), or short-acting beta2-agonists (for all patients using Symbicort® Turbuhaler® only for maintenance therapy – therapy C).
When using Symbicort® as maintenance therapy, the patient’s attention should be drawn to the need for regular use of a maintenance dose of the drug in accordance with the selected therapy, even in cases where there are no symptoms of the disease.
It is recommended to instruct the patient to rinse the mouth with water after inhaling maintenance doses in order to prevent the risk of developing candidiasis of the oral and pharyngeal mucosa. It is also necessary to rinse your mouth with water after inhalation on demand in case of development of candidiasis of the oral mucosa and pharynx.
It is recommended to gradually reduce the maintenance dose of the drug before stopping treatment and it is not recommended to abruptly discontinue treatment. Inhaled glucocorticosteroids should not be completely discontinued, except in cases where temporary withdrawal is necessary to confirm the diagnosis of bronchial asthma.
Symbicort® Turbuhaler® 80/4.5 mcg/dose is not intended for patients with mild to severe bronchial asthma.
Increased symptoms of the disease
During therapy with Symbicort® Turbuhaler®, exacerbations and the development of serious adverse events associated with bronchial asthma may occur. Patients should continue treatment but seek medical attention if asthma symptoms are not controlled or if symptoms worsen after starting therapy.
If therapy is insufficiently effective or the maximum recommended doses of Symbicort® are exceeded, it is necessary to reconsider treatment tactics. Sudden and progressive deterioration in control of symptoms of asthma or COPD is a potentially life-threatening condition and requires urgent medical attention. In this situation, you should consider increasing the dose of glucocorticosteroids, for example, prescribing a course of oral glucocorticosteroids, or treatment with antibiotics in case of infection. In case of severe exacerbation, monotherapy with a combination of an inhaled glucocorticosteroid and a long-acting beta2-adrenergic agonist is not enough.
Transfer from oral therapy
If there is reason to believe that adrenal function has been impaired due to previous systemic glucocorticosteroid therapy, precautions should be taken when transferring patients to treatment with Symbicort®.
The benefits of inhaled budesonide therapy generally minimize the need for oral corticosteroids, but patients who discontinue oral corticosteroid therapy may experience long-term adrenal insufficiency. Patients who have previously required acute high-dose corticosteroids or have received long-term treatment with high-dose inhaled corticosteroids may also be at risk. It is necessary to provide additional administration of glucocorticosteroids during periods of stress or surgery. Excipients
Symbicort® Turbuhaler® contains lactose (< 1 mg/inhalation). Typically this amount does not cause problems in patients with lactose intolerance.
Precautions for specific diseases
Precautions should be taken when treating patients with a prolonged QTc interval. Taking formoterol may cause a prolongation of the QTc interval.
When beta2-agonists are used together with drugs that can cause or enhance the hypokalemic effect, for example, xanthine derivatives, steroids or diuretics, the hypokalemic effect of beta2-agonists may be enhanced. Special precautions should be taken in patients with unstable bronchial asthma who use short-acting bronchodilators to relieve attacks during exacerbation of severe bronchial asthma, since the risk of developing hypokalemia increases against the background of hypoxia and in other conditions when the likelihood of developing a hypokalemic effect increases. In such cases, it is recommended to monitor serum potassium levels.
During treatment, blood glucose concentrations should be monitored in patients with diabetes mellitus.
The need for the use and dose of inhaled glucocorticosteroids should be reconsidered in patients with active or inactive forms of pulmonary tuberculosis, fungal, viral or bacterial infections of the respiratory system.
Systemic action
Systemic effects may occur when using any inhaled glucocorticosteroids, especially when using high doses of drugs over a long period of time. Systemic effects are less likely to occur with inhaled therapy than with oral corticosteroids. Possible systemic effects include adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma.
Due to the potential effect of inhaled corticosteroids on bone mineral density, special attention should be paid to patients taking high doses of the drug for a long period with risk factors for osteoporosis. Studies of long-term use of inhaled budesonide in children at an average daily dose of 400 mcg (metered dose) or adults at a daily dose of 800 mcg (metered dose) did not show a significant effect on bone mineral density. There is no data on the effect of high doses of Symbicort® Turbuhaler® on bone mineral density.
Paradoxical bronchospasm
As with any other inhalation therapy, paradoxical bronchospasm may occur with an immediate increase in wheezing after dosing. In this regard, therapy with Symbicort® should be discontinued, treatment tactics should be reconsidered and, if necessary, alternative therapy should be prescribed.
Pediatric patient population
It is recommended to regularly monitor the growth of children receiving long-term inhaled glucocorticosteroid therapy. In case of established growth retardation, therapy should be reconsidered in order to reduce the dose of inhaled glucocorticosteroid. It is necessary to carefully evaluate the ratio of the benefits of glucocorticosteroid therapy to the possible risk of growth retardation. When choosing therapy, it is recommended to consult a pediatric pulmonologist.
Based on limited data from studies of long-term corticosteroid use, it can be assumed that most children and adolescents treated with inhaled budesonide will eventually achieve normal adult height. However, minor short-term growth retardation has been reported, mainly in the first year of treatment.
Population of patients with COPD
Data from clinical studies of the drug Symbicort® Turbuhaler® in patients with COPD with pre-bronchodilator FEV1 > 50% of predicted and with post-bronchodilator FEV1 < 70% of predicted are not available (see section “Pharmacodynamics”).
Clinical studies and meta-analyses have shown that the use of inhaled corticosteroids during maintenance treatment of COPD may lead to an increased risk of pneumonia. Clinicians should be aware of the possibility of pneumonia in patients with COPD, since the clinical signs of pneumonia and exacerbation of the disease often overlap.
Effect on the ability to drive vehicles and machines Symbicort® Turbuhaler® does not affect the ability to drive vehicles and machines. May affect the ability to drive vehicles and machinery if side effects develop.
Active ingredient
Active ingredient
Budesonide, Formoterol
Composition
Composition
Each dose delivered contains:
80/4.5 mcg/dose
Pregnancy
Pregnancy
There are no clinical data on the use of Symbicort® or the combined use of formoterol and budesonide during pregnancy.
During pregnancy, Symbicort® should be used only in cases where the benefit of the drug outweighs the potential risk to the fetus. The lowest effective dose of budesonide needed to maintain adequate control of asthma symptoms should be used.
Inhaled budesonide is excreted in breast milk, however, when used in therapeutic doses, no effects on the child were noted. It is not known whether formoterol passes into women’s breast milk. Symbicort® should only be prescribed to breastfeeding women if the expected benefit to the mother is greater than any possible risk to the baby.
Contraindications
Contraindications
• Hypersensitivity to budesonide, formoterol or inhaled lactose.
• Children under 6 years of age.
• Lactose intolerance, lactase deficiency or glucose-galactose malabsorption (see section “Special instructions”).
With caution: pulmonary tuberculosis (active or inactive form); fungal, viral or bacterial infections of the respiratory system, thyrotoxicosis, pheochromocytoma, diabetes mellitus, decreased function of the adrenal cortex, uncontrolled hypokalemia, hypertrophic obstructive cardiomyopathy, idiopathic hypertrophic subaortic stenosis, severe arterial hypertension, aneurysm of any location or other severe cardiovascular diseases (coronary heart disease, tachyarrhythmia or severe heart failure), prolongation of the QT interval (taking formoterol may cause prolongation of the QTc interval).
Side Effects
Side Effects
With the combined use of budesonide and formoterol, there was no increase in the incidence of adverse reactions. The most common adverse reactions associated with the use of the drug are such pharmacologically expected adverse events for b2-adrenergic agonists, such as tremor and palpitations; symptoms are usually of moderate severity and resolve on their own within a few days after starting treatment.
Adverse reactions associated with the use of budesonide or formoterol are listed below by organ system class and incidence. The frequency of reactions is presented in the following gradation: very often (≥1/10), often (≥1/100, <1/10), infrequently (≥1/1000, <1/100), rarely (≥1/10000, <1/1000), very rarely (<1/10000).
Infections and infestations: often – candidiasis of the oral mucosa and pharynx, pneumonia (in patients with COPD)
Immune system disorders: rarely – immediate and delayed hypersensitivity reactions (for example, dermatitis, exanthema, urticaria, pruritus, angioedema, anaphylactic reaction)
Metabolic and nutritional disorders: rarely – hypokalemia; very rarely – hyperglycemia, signs or symptoms of systemic effects of glucocorticosteroids (including adrenal hypofunction)
Mental disorders: infrequently – psychomotor agitation, anxiety, sleep disturbances; very rarely – depression, behavioral disorders (mainly in children)
Nervous system disorders: often – headache, tremor; infrequently – dizziness; very rarely – taste disturbances
Disorders of the heart and blood vessels: often – palpitations; infrequently – tachycardia; rarely – arrhythmia (for example, atrial fibrillation, supraventricular tachycardia, extrasystole); very rarely – angina pectoris, blood pressure fluctuations
Disorders of the respiratory system, chest and mediastinal organs: often – cough, hoarseness, mild irritation of the pharyngeal mucosa; rarely – bronchospasm
Gastrointestinal disorders: uncommon – nausea
Skin and subcutaneous tissue disorders: uncommon – bruising
Musculoskeletal and connective tissue disorders: uncommon – muscle cramps
Systemic effects of inhaled corticosteroids may occur when high doses are used over a long period of time.
The use of b2-adrenergic agonists can lead to an increase in the blood levels of insulin, free fatty acids, glycerol and ketone bodies.
Interaction
Interaction
Taking ketoconazole 200 mg once daily increased the plasma concentration of budesonide (single oral dose of 3 mg) when administered together by an average of 6-fold. When using ketoconazole 12 hours after taking budesonide, the plasma concentration of the latter increased, on average, 3 times. There is no information about such an interaction with inhaled budesonide, however, a noticeable increase in the concentration of the drug in the blood plasma should be expected. Since there are no data for dosage recommendations, the combination of drugs described above should be avoided. If this is not possible, the time interval between the use of ketoconazole and budesonide should be increased as much as possible. A dose reduction of budesonide should also be considered. Other strong CYP3A4 inhibitors are also likely to significantly increase budesonide plasma concentrations. Symbicort® for the relief of attacks/symptoms with anti-inflammatory effects is not recommended in patients receiving strong CYP3A4 inhibitors.
β-adrenergic receptor blockers may weaken the effect of formoterol. Symbicort® should not be prescribed simultaneously with beta-blockers (including eye drops), except in cases of emergency.
Concomitant use of Symbicort® Turbuhaler® and quinidine, disopyramide, procainamide, phenothiazines, antihistamines (terfenadine), monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants may prolong the QTc interval and increase the risk of ventricular arrhythmias.
In addition, levodopa, levothyroxine, oxytocin and alcohol can reduce the tolerance of the heart muscle to b2-agonists.
The combined use of MAO inhibitors, as well as drugs with similar properties, such as furazolidone and procarbazine, may cause an increase in blood pressure. There is an increased risk of developing arrhythmias in patients undergoing general anesthesia with halogenated hydrocarbon preparations.
When taking Symbicort® Turbuhaler® and other b-adrenergic drugs together, the side effects of formoterol may be increased.
As a result of the use of beta2-agonists, hypokalemia may occur, which may be exacerbated by concomitant treatment with xanthine derivatives, mineral derivatives of glucocorticosteroids or diuretics. Hypokalemia may increase the susceptibility to the development of arrhythmias in patients taking cardiac glycosides.
There were no interactions of budesonide and formoterol with other drugs used to treat bronchial asthma.
Overdose
Overdose
Symptoms of formoterol overdose: tremor, headache, rapid heartbeat. In isolated cases, the development of tachycardia, hyperglycemia, hypokalemia, prolongation of the QTc interval, arrhythmia, nausea and vomiting was reported. Can be assigned
supportive and symptomatic treatment. The use of formoterol at a dose of 90 mcg for 3 hours in patients with acute bronchial obstruction was safe.
If it is necessary to discontinue the drug Symbicort® Turbuhaler® due to an overdose of formoterol, which is part of the combination drug, you should consider prescribing an appropriate glucocorticosteroid.
In case of acute overdose of budesonide, even in significant doses, no clinically significant effects are expected. With chronic use of excessive doses, systemic effects of glucocorticosteroids, such as hypercortisolism and suppression of adrenal function, may occur.
Storage conditions
Storage conditions
At temperatures below 30 C, in places inaccessible to children.
Shelf life
Shelf life
3 years. Do not use after expiration date.
Manufacturer
Manufacturer
AstraZeneca Dunkirk Production, France
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At temperatures below 30 C, out of the reach of children. |
| Manufacturer | AstraZeneca Dunkirk Production, France |
| Medication form | metered aerosol for inhalation |
| Brand | AstraZeneca Dunkirk Production |
Other forms…
Bronchial asthma
Symbicort Rapihaler, 160 mcg+4, 5 mcg/dose aerosol 120 doses
Related products
Buy Symbicort Rapihaler, aerosol 80 mcg+4, 5 mcg/dose 120 doses with delivery to USA, UK, Europe and over 120 other countries.