No products in the cart.
Sumatriptan-Teva, 50 mg 2 pcs
€6.78 €5.93
Description
Pharmacotherapeutic group: antimigraine medicine
ATX code: N02CC01
Pharmacological properties
Pharmacodynamics
Mechanism of action. Sumatriptan is a selective agonist of vascular 5-hydroxytryptamine-1 receptors (5-HT1D) and does not affect other 5-HT receptor subtypes (5-HT2-5-HT7). The 5-HT1D receptors are located mainly in the cranial blood vessels of the brain, and their stimulation leads to narrowing of these vessels.
In animals, sumatriptan acts selectively on vasoconstriction of carotid artery branches without affecting blood flow in cerebral vessels. The carotid artery vasculature supplies blood to the extracranial and intracranial tissues (including meningeal membranes), and dilation of these vessels and/or swelling of their walls is thought to be the primary mechanism of migraine in humans.
In addition, experimental data suggest that sumatriptan reduces trigeminal nerve sensitivity. Both of these effects may underlie the antimigraine action of sumatriptan.
The clinical effect is usually noted 30 minutes after oral administration of 100 mg of the drug.
While the recommended oral dose is 50 mg, migraine attacks vary in severity from patient to patient. Doses from 25 mg to 100 mg have shown greater efficacy than placebo in clinical trials, but the 25 mg dose is statistically significantly less effective than 50 mg and 100 mg.
Sumatriptan has demonstrated efficacy in the treatment of migraine attacks, including menstrual-associated migraine.
Pharmacokinetics
Migraine attacks have no significant effect on the pharmacokinetics of sumatriptan taken orally.
Extraction. After oral administration, sumatriptan is rapidly absorbed, with 70% of maximum plasma concentration reached after 45 min. After a dose of 100 mg, the mean value of maximum plasma concentration is 54 ng/ml. The mean value of absolute bioavailability is 14 %, partly due to presystemic metabolism, partly due to incomplete absorption.
Distribution. Sumatriptan binds to plasma proteins to a negligible extent (14-21%), the average total volume of distribution is 170 liters.
Metabolism. The major metabolite, the indoleucetic analogue of sumatriptan, is excreted primarily with the urine, as free acid and glucuronide conjugate. This metabolite has no activity toward 5-HT1 and 5-HT2 – serotonin receptors. Secondary metabolites of sumatriptan have not been detected.
Evolution. The elimination half-life is approximately 2 h. Mean total plasma clearance is approximately 1,160 mL/min, mean renal clearance is approximately 260 mL/min, and extrarenal clearance is approximately 80% of total clearance.
Sumatriptan is metabolized by monoamine oxidase A.
Special patient groups
Patients with impaired liver function.
Indications
Indications
Relief of migraine attacks with or without aura, including attacks of menstrually associated migraine.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antimigraine drug
ATX code: N02CC01
Pharmacological properties
Pharmacodynamics
Mechanism of action. Sumatriptan is a selective agonist of vascular 5-hydroxytryptamine-1 receptors (5-HT1D), does not affect other subtypes of 5-HT receptors (5-HT2-5-HT7). 5-HT1D receptors are located primarily in the cranial blood vessels of the brain, and their stimulation causes these vessels to constrict.
In animals, sumatriptan selectively acts on vasoconstriction of the branches of the carotid artery without affecting blood flow in the vessels of the brain. The carotid artery vasculature supplies extracranial and intracranial tissues (including the meningeal membranes), and dilation of these vessels and/or swelling of their walls is believed to be the primary mechanism of migraine in humans.
In addition, experimental data suggest that sumatriptan reduces the sensitivity of the trigeminal nerve. Both of these effects may underlie the antimigraine action of sumatriptan.
The clinical effect is usually observed 30 minutes after oral administration of 100 mg of the drug.
Although the recommended oral dose is 50 mg, migraine attacks vary in severity within and between patients. Doses of 25 mg to 100 mg have been shown to be more effective than placebo in clinical studies, but the 25 mg dose is statistically significantly less effective than 50 mg and 100 mg.
Sumatriptan has demonstrated effectiveness in the treatment of migraine attacks, including menstrually associated migraine.
Pharmacokinetics
Migraine attacks do not have a significant effect on the pharmacokinetics of sumatriptan taken orally.
Suction. After oral administration, sumatriptan is rapidly absorbed, 70% of the maximum plasma concentration is achieved after 45 minutes. After taking a dose of 100 mg, the average maximum plasma concentration is 54 ng/ml. The average absolute bioavailability is 14%, partly due to first-pass metabolism and partly due to incomplete absorption.
Distribution. Sumatriptan binds to plasma proteins to a small extent (14-21%), the average total volume of distribution is 170 L.
Metabolism. The main metabolite, the indoleacetic analogue of sumatriptan, is excreted primarily in the urine as the free acid and glucuronide conjugate. This metabolite has no activity towards 5-HT1 and 5-HT2 – serotonin receptors. No minor metabolites of sumatriptan were detected.
Excretion. The half-life is approximately 2 hours. The average total plasma clearance is approximately 1160 ml/min, the average renal clearance is approximately 260 ml/min, and extrarenal clearance is approximately 80% of the total clearance.
Sumatriptan is metabolized by monoamine oxidase A.
Special patient groups
Patients with impaired liver function. Due to a decrease in the presystemic clearance of sumatriptan in patients with impaired liver function, the content of sumatriptan in the blood plasma increases.
Special instructions
Special instructions
Sumatriptan should only be prescribed if the diagnosis of migraine is beyond doubt.
Sumatriptan should not be used for prophylactic purposes.
Sumatriptan is contraindicated for use in hemiplegic, basilar and ophthalmoplegic forms of migraine. As with other drugs used to treat acute migraine attacks, other types of neurological pathology must be excluded before treating a headache attack in patients with previously undiagnosed migraine or in patients with atypical migraine. It should be noted that patients with migraine have an increased risk of developing certain cerebrovascular events (eg, stroke or transient ischemic attack).
Taking sumatriptan may be associated with transient symptoms such as pain and tightness in the chest, spreading to the neck; symptoms may be intense. If there is reason to believe that these symptoms are a manifestation of coronary artery disease, it is necessary to conduct an appropriate diagnostic examination.
Sumatriptan should not be used in patients at risk of cardiovascular pathology without prior examination to exclude it (such patients include postmenopausal women, men over the age of 40 years and patients with risk factors for coronary artery disease). However, the examination does not always reveal heart disease in every patient. In very rare cases, serious cardiovascular adverse reactions may occur in patients without a history of cardiovascular disease.
Sumatriptan should be used with caution in patients with controlled hypertension, as transient increases in blood pressure and peripheral vascular resistance have been observed in a small number of patients.
There are rare reports from post-marketing surveillance of the development of serotonin syndrome (including mental disorders, autonomic lability and neuromuscular disorders) as a result of simultaneous use of SSRIs and sumatriptan. The development of serotonin syndrome has also been reported during concomitant use of triptans with SNRIs.
If a patient is indicated for simultaneous use of SSRIs and/or SNRIs, the patient’s condition should be carefully monitored.
Concomitant use of any triptan (5-HT1 agonist) with sumatriptan is not recommended.
Sumatriptan should be used with caution in patients in whom the absorption, metabolism, or elimination of sumatriptan may be significantly altered (for example, patients with impaired renal or hepatic function).
Sumatriptan should be used with caution in patients with a history of seizures or other risk factors for lowering the seizure threshold.
In patients with known hypersensitivity to sulfonamides, taking sumatriptan may cause allergic reactions that range from skin manifestations of hypersensitivity to anaphylaxis. Cross-sensitivity data are limited, but caution should be exercised when using sumatriptan in these patients.
Overuse of medications intended to treat migraine attacks is associated with increased headaches in sensitive patients (drug overuse headache). In this case, the possibility of discontinuing the drug should be considered.
Do not exceed the recommended dose of sumatriptan.
Impact on the ability to drive vehicles and machinery
Patients with migraine may experience drowsiness associated with both the disease itself and the use of sumatriptan. Patients should be especially careful when driving and operating moving machinery.
Active ingredient
Active ingredient
Sumatriptan
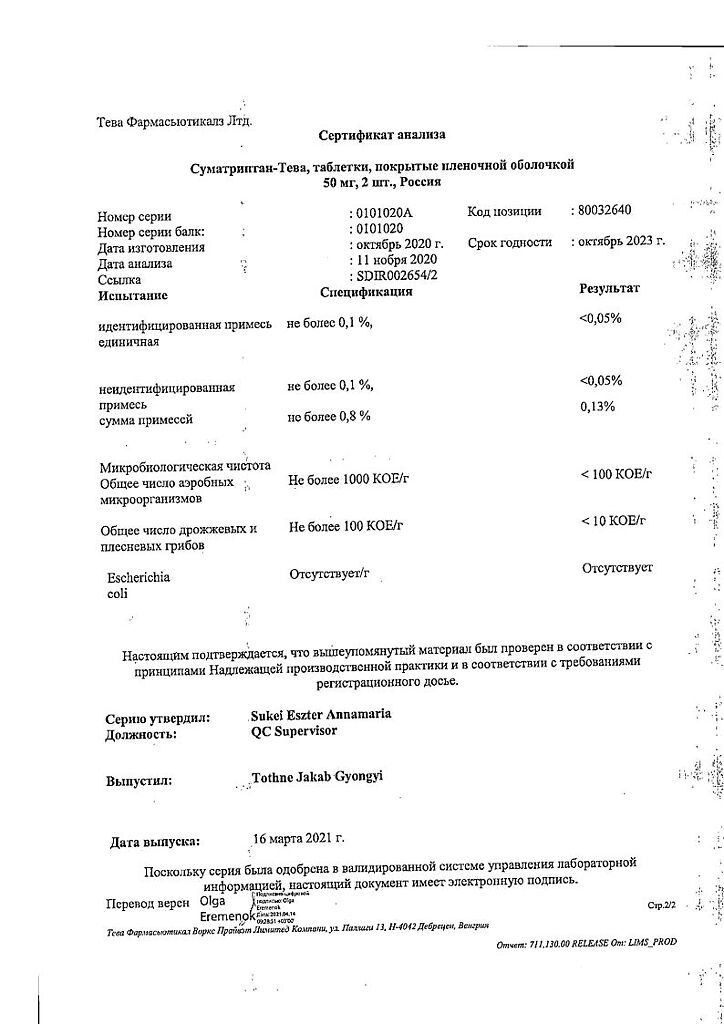
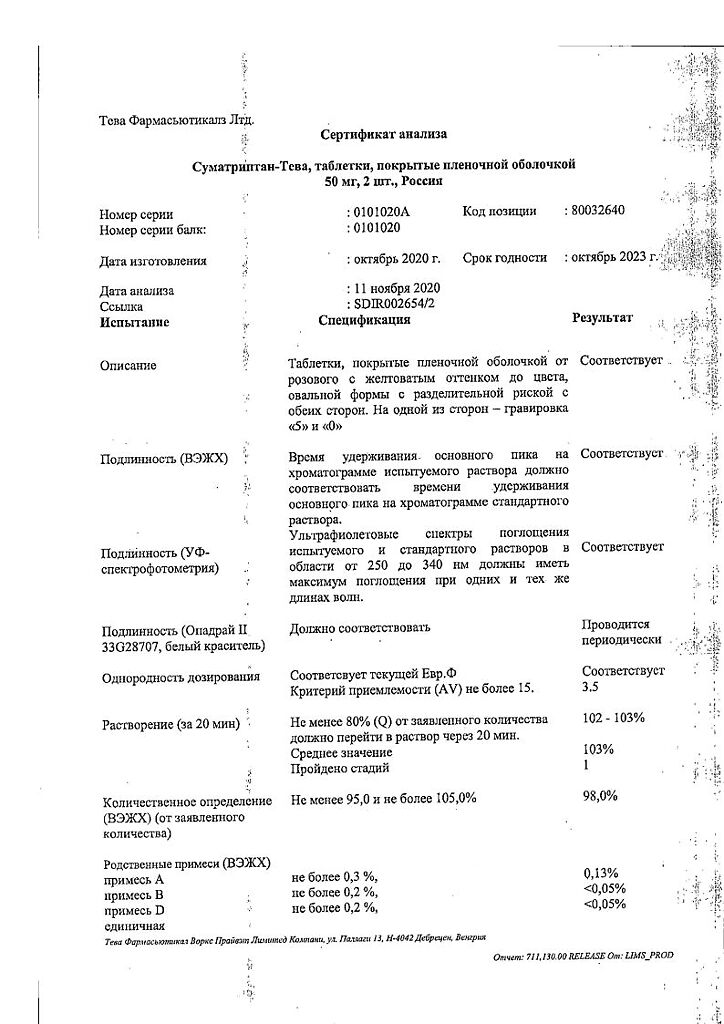
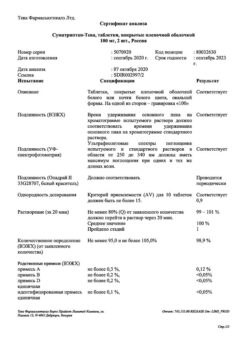
Composition
Composition
1 tablet 50 mg contains: active ingredient sumatriptan (sumatriptan succinate) 50.00 mg (70.00 mg); excipients: lactose monohydrate 70.00 mg, croscarmellose sodium 1.50 mg, microcrystalline cellulose 6.75 mg, colloidal silicon dioxide 0.25 mg, magnesium stearate 1.50 mg; shell Opadry II 33G23092 peach (hypromellose (E 464) 2.0000 mg, titanium dioxide (E 171) 1.1725 mg, lactose monohydrate 1.1000 mg, macrogol-3000 0.4000 mg, triacetin 0.3000 mg, iron dye red oxide (E 172) 0.0180 mg, yellow iron oxide dye (E 172) 0.0090 mg, black iron oxide dye (E 172) 0.0005 mg).
Pregnancy
Pregnancy
Pregnancy
Caution should be exercised when using the drug during pregnancy, it is necessary to evaluate the potential benefits to the mother and possible risks to the fetus.
Post-registration follow-up data are available from more than 1000 women who took sumatriptan during the first trimester of pregnancy. Due to insufficient information, it is premature to draw final conclusions about the increased risk of birth defects. Experience with the use of the drug in women in the second and third trimesters of pregnancy is limited.
An evaluation of experimental animal studies did not show a direct teratogenic or adverse effect of the drug on prenatal and postnatal development. However, effects on embryonic and fetal viability have been observed in rabbits.
Breastfeeding period
Following subcutaneous administration, sumatriptan has been shown to be excreted into breast milk. Exposure to the newborn can be minimized by avoiding breastfeeding for 12 hours after taking the drug.
Contraindications
Contraindications
Hypersensitivity to any of the components included in the drug;
hemiplegic, basilar and ophthalmoplegic forms of migraine;
coronary heart disease (CHD) (including myocardial infarction, post-infarction cardiosclerosis, Prinzmetal’s angina), as well as symptoms suggesting the presence of CHD;
occlusive diseases of peripheral vessels;
stroke or transient ischemic attack (including a history);
uncontrolled arterial hypertension;
concomitant use with ergotamine or its derivatives (including methysergide) or other triptans/5-HT1 receptor agonists;
use while taking monoamine oxidase inhibitors (MAOIs) or earlier than 2 weeks after discontinuation of these drugs;
severe impairment of liver and/or kidney function;
lactase deficiency, galactose intolerance and glucose-galactose malabsorption (the drug contains lactose).
age under 18 years and over 65 years (safety and effectiveness have not been established).
With caution
Controlled arterial hypertension;
diseases that may alter the absorption, metabolism, or elimination of this drug (for example, impaired renal or hepatic function);
epilepsy (including any conditions with a decrease in the seizure threshold);
in patients with hypersensitivity to sulfonamides (taking sumatriptan can cause allergic reactions, the severity of which varies from skin manifestations of hypersensitivity to anaphylaxis). Cross-sensitivity data are limited, but caution should be exercised when using sumatriptan in such patients.
Side Effects
Side Effects
The adverse reactions presented below are listed according to organ system involvement and frequency of occurrence. Frequency is defined as follows: very common (> 1/10); often (> 1/100 and < 1/10); uncommon (> 1/1000 and 1/10,000 and < 1/1000); very rare (<1/10,000); unknown (frequency cannot be estimated from available data).
Clinical trial data
Nervous system disorders: often – dizziness, drowsiness, sensory disturbances (including paresthesia and decreased sensitivity).
Vascular disorders: often – transient increase in blood pressure (shortly after taking the drug), hot flashes.
Disorders of the respiratory system, chest and mediastinal organs: often – shortness of breath.
Gastrointestinal disorders: often – nausea, vomiting (the cause-and-effect relationship between the occurrence of adverse reactions and the use of the drug has not been proven).
Musculoskeletal and connective tissue disorders: often – a feeling of heaviness (usually transient, can be intense and occur in any part of the body, including the chest and throat).
General disorders and disorders at the injection site: often – pain, a feeling of cold or heat, a feeling of pressure or tightness (usually transient, can be intense and occur in any part of the body, including the chest and throat), weakness, fatigue (usually mild or moderate, transient).
Laboratory and instrumental data: very rarely – minor deviations in liver test parameters.
Post-registration observation data
Immune system disorders: unknown – hypersensitivity reactions, which range from skin manifestations of hypersensitivity to anaphylaxis.
Nervous system disorders: unknown – seizures (in some cases observed in patients with a history of seizures or with concomitant conditions predisposing to seizures; in some patients no risk factors were identified), tremor, dystonia, nystagmus, scotoma.
Visual disturbances: unknown – flickering, diplopia, decreased visual acuity. Loss of vision (usually transient). However, visual disturbances can be caused by the migraine attack itself.
Cardiac disorders: unknown – bradycardia, tachycardia, palpitations, arrhythmias, ECG signs of transient myocardial ischemia, coronary vasospasm, angina pectoris, myocardial infarction.
Vascular disorders: unknown – decreased blood pressure, Raynaud’s syndrome.
Gastrointestinal disorders: unknown – ischemic colitis, diarrhea.
Musculoskeletal and connective tissue disorders: often – myalgia; unknown – neck stiffness, arthralgia.
Mental disorders: unknown – anxiety.
Skin and subcutaneous tissue disorders: unknown – hyperhidrosis.
Interaction
Interaction
There was no interaction of sumatriptan with propranolol, flunarizine, pizotifen and ethyl alcohol.
When taken simultaneously with ergotamine, prolonged vasospasm was observed.
There is limited data on interactions with drugs containing ergotamine or other triptans/5-HT1 receptor agonists, there is a theoretical possibility of increased risk of coronary vasospasm, and concomitant use of these drugs is contraindicated.
The period of time that should elapse between the use of sumatriptan and ergotamine-containing drugs or another triptan/5-HT1 receptor agonist is unknown. It will depend, among other things, on the dose and type of drugs prescribed. The effect may be additive. It is recommended to wait at least 24 hours after taking medications containing ergotamine or another triptan/5-HT1 receptor agonist before using sumatriptan. Conversely, it is recommended to wait at least 6 hours after using sumatriptan before using drugs containing ergotamine, and at least 24 hours before using another triptan/5-HT1 receptor agonist.
Interaction between sumatriptan and MAO inhibitors is possible; their simultaneous use is contraindicated.
There are rare reports from post-marketing surveillance of the development of serotonin syndrome (including mental disorders, autonomic lability and neuromuscular disorders) as a result of the simultaneous use of selective serotonin reuptake inhibitors (SSRIs) and sumatriptan. The development of serotonin syndrome has also been reported during concomitant use of triptans with selective serotonin norepinephrine reuptake inhibitors (SNRIs).
Adverse reactions may occur more frequently during the simultaneous use of triptans and herbal preparations containing St. John’s wort.
Overdose
Overdose
Symptoms. Taking sumatriptan orally at a dose of more than 400 mg did not cause any adverse reactions other than those listed above.
Treatment. In case of overdose, patients should be monitored for at least 10 hours and, if necessary, symptomatic therapy should be provided. There are no data on the effect of hemodialysis or peritoneal dialysis on plasma concentrations of sumatriptan.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25º C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Teva Pharmaceutical Works Private Limited Company, Hungary
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25º C. Keep out of reach of children. |
| Manufacturer | Teva Pharmaceutical Works Production Limited Company, Hungary |
| Medication form | pills |
| Brand | Teva Pharmaceutical Works Production Limited Company |
Other forms…
Related products
Buy Sumatriptan-Teva, 50 mg 2 pcs with delivery to USA, UK, Europe and over 120 other countries.