No products in the cart.
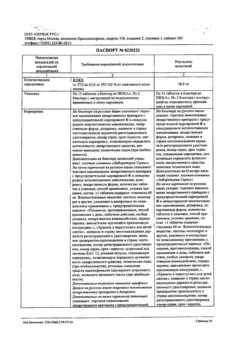
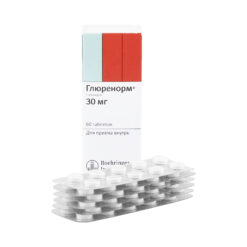
Statiglin, tablets 1,75mg 120 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Glibenclamide has pancreatic and extrapancreatic effects. It stimulates insulin secretion by reducing the threshold of glucose irritation of pancreatic beta cells, increases insulin sensitivity and the degree of its binding to target cells, increases insulin release, increases the effect of insulin on glucose absorption by muscle and liver, inhibits lipolysis in adipose tissue (extrapancreatic effects). It acts in the second stage of insulin secretion.
It has hypolipidemic effect, reduces blood thrombogenic properties. Hypoglycemic effect develops after 2 hours, reaches its maximum after 7-8 hours and lasts 12 hours. The drug provides smooth increase of insulin concentration and smooth decrease of plasma glucose concentration, which reduces the risk of hypoglycemic states. The activity of glibenclamide occurs with preserved endocrine function of the pancreas.
Pharmacokinetics:
Absorption
Absorption from the gastrointestinal tract is 48-84% when ingested. Time of reaching maximum concentration in blood (Tmax) is 1-2 hours. Bioavailability of glibenclamide is 100%. Concomitant intake of food has no significant effect on the absorption of glibenclamide.
Distribution
The volume of distribution (Vd) is 9-10 liters. The binding to plasma proteins is 95-99%. The placental barrier passes poorly.
Metabolism
Glibenclamide is almost completely metabolized in the liver to form two inactive metabolites.
Excretion
One of the inactive metabolites is excreted by the kidneys, the other is excreted through the intestine in approximately equal proportions. The elimination half-life (T1/2) is from 3 to 10-16 hours.
Pharmacokinetics in patients with hepatic impairment
The excretion of the active substance from the blood plasma is delayed in patients with hepatic impairment.
Pharmacokinetics in renal failure
In patients with renal failure the excretion of metabolites through the intestine is compensatory increased. When creatinine clearance ≥ 30 ml/min total excretion rate of glibenclamide remains unchanged, in severe renal failure cumulation is possible.
.
Indications
Indications
Type 2 diabetes mellitus, in addition to diet therapy and exercise, as monotherapy or as part of combination therapy with metformin or other oral hypoglycemic drugs, except sulfonylureas and glinides.
Pharmacological effect
Pharmacological effect
Glibenclamide has pancreatic and extrapancreatic effects. Stimulates insulin secretion by lowering the threshold for irritation of pancreatic beta cells by glucose, increases sensitivity to insulin and the degree of its binding to target cells, increases insulin release, enhances the effect of insulin on glucose uptake by muscles and liver, inhibits lipolysis in adipose tissue (extrapancreatic effects). Acts in the second stage of insulin secretion.
It has a hypolipidemic effect, reduces the thrombogenic properties of blood. The hypoglycemic effect develops after 2 hours, reaches a maximum after 7-8 hours and lasts 12 hours. The drug provides a smooth increase in insulin concentration and a smooth decrease in the concentration of glucose in the blood plasma, which reduces the risk of hypoglycemic conditions. The activity of glibenclamide occurs when the endocrine function of the pancreas is preserved.
Pharmacokinetics:
Absorption
When taken orally, absorption from the gastrointestinal tract is 48-84%. The time to reach maximum concentration in the blood (Tmax) is 1-2 hours. The bioavailability of glibenclamide is 100%. Concomitant food intake does not have a significant effect on the absorption of glibenclamide.
Distribution
Volume of distribution (Vd) 9-10 l. Communication with plasma proteins is 95-99%. The placental barrier does not pass well.
Metabolism
Glibenclamide is almost completely metabolized in the liver to form two inactive metabolites.
Removal
One of the inactive metabolites is excreted by the kidneys, the other through the intestines in approximately equal proportions. The half-life (T1/2) is from 3 to 10-16 hours.
Pharmacokinetics in patients with impaired liver function
In patients with impaired liver function, the removal of the active substance from the blood plasma is slowed down.
Pharmacokinetics in renal failure
In patients with renal failure, the excretion of metabolites through the intestines compensatory increases. When creatinine clearance is ≥ 30 ml/min, the overall rate of excretion of glibenclamide from the body remains unchanged; in severe renal failure, cumulation is possible.
Special instructions
Special instructions
The drug should be taken regularly and, if possible, at the same time. It is necessary to carefully follow the drug intake regimen and diet. The physician should carefully consider prescribing glibenclamide to patients with impaired liver and kidney function, as well as hypofunction of the thyroid gland, anterior pituitary gland or adrenal cortex. It is necessary to adjust the dose of glibenclamide in case of physical and emotional stress, or changes in diet.
Factors that contribute to the risk of developing hypoglycemia include:
– reluctance or inability of the patient (more often observed in elderly patients) to cooperate with the doctor;
– malnutrition, irregular eating or skipping meals;
– imbalance between physical activity and carbohydrate consumption;
– diet change;
– alcohol consumption, especially in combination with skipping meals;
– severe renal dysfunction;
– severe liver dysfunction;
– overdose of glibenclamide;
– diarrhea, vomiting;
– some decompensated endocrine disorders that impair carbohydrate metabolism or adrenergic counterregulation in response to hypoglycemia (for example, some dysfunctions of the thyroid gland and anterior pituitary gland, adrenal insufficiency);
– simultaneous use of certain medications.
Major surgical interventions and injuries, extensive burns, infectious diseases with febrile syndrome may require the abolition of oral hypoglycemic drugs and the prescription of insulin.
During treatment, it is not recommended to stay in the sun for a long time.
The use of sulfonylurea derivatives, which include glibenclamide, in patients with glucose-6-phosphate dehydrogenase deficiency can lead to the development of hemolytic anemia, therefore hypoglycemic agents that are not sulfonylurea derivatives should be used.
Concomitant use of medications that act on the central nervous system and lower blood pressure (including beta-blockers), as well as autonomic neuropathy, can mask the symptoms of hypoglycemia.
In elderly patients, the risk of developing hypoglycemia is slightly higher, so more careful selection of the dose of the drug and regular monitoring of fasting and postprandial blood glucose concentrations are necessary, especially at the beginning of treatment.
Alcohol can provoke the development of hypoglycemia, as well as the development of a disulfiram-like reaction (nausea, vomiting, abdominal pain, a feeling of heat on the face and upper body, tachycardia, dizziness, headache), so you should refrain from drinking alcohol during treatment with glibenclamide.
With each change of doctor (for example, when hospitalized in a hospital, when sick on vacation), the patient must inform the attending physician about this. that he has diabetes.
Fertility
There are no data on the effect of glibenclamide on fertility.
Impact on the ability to drive vehicles. Wed and fur.:
When taking glibenclamide, hypoglycemia may develop, and, as a result, a decrease in reaction and the ability to concentrate, therefore, during treatment with the drug, care must be taken when driving and engaging in other potentially hazardous activities that require concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Glibenclamide
Composition
Composition
Composition per tablet:
Active ingredient:
glibenclamide 1.75 mg
Excipient:
lactose monohydrate – 46.5 mg;
povidone K30 – 1.75 mg;
low-substituted hyprolose – 11.5 mg;
microcrystalline cellulose – 23.5 mg;
sodium carboxymethyl starch – 4.0 mg;
colloidal silicon dioxide – 0.5 mg;
sodium stearyl fumarate – 0.5 mg.
Contraindications
Contraindications
– Hypersensitivity to glibenclamide and/or any excipient of the drug;
– hypersensitivity to other sulfonylurea derivatives; sulfonamides; diuretics containing a sulfonamide group in the molecule; probenecid, because cross-reactions may occur;
– diabetes mellitus type 1;
– diabetic ketoacidosis, diabetic precoma and coma;
– condition after resection of the pancreas;
– severe liver failure;
– severe renal failure (creatinine clearance <30 ml/min);
– severe adrenal insufficiency;
– decompensation of carbohydrate metabolism in infectious diseases, burns, injuries or after major surgical operations, when insulin therapy is indicated;
– intestinal obstruction, gastric paresis;
– hereditary lactose intolerance, lactase deficiency or glucose and lactose malabsorption syndrome;
– pregnancy and breastfeeding;
– children under 18 years of age (efficacy and safety have not been studied);
– porphyria;
– simultaneous use with bosentan.
With caution:
Glibenclamide should be used with caution in febrile syndrome; diseases of the thyroid gland (with decreased function); insufficiency of the function of the anterior pituitary gland or adrenal cortex; glucose-6-dehydrogenase deficiency; chronic alcoholism, acute alcohol intoxication; conditions accompanied by malabsorption of food and the risk of hypoglycemia (prolonged fasting, insufficient intake of carbohydrates from food, excessive exercise, diarrhea or vomiting); mild to moderate renal failure (creatinine clearance ≥ 30 ml/min); liver failure of mild to moderate severity; cerebral atherosclerosis; in elderly patients over 65 years of age due to the risk of hypoglycemia.
Side Effects
Side Effects
Classification of adverse reactions by frequency of development: often (> 1/100, 1/1000, 1/10000, <1/1000), very rare (<1/10000), including isolated reports.
Metabolic and nutritional disorders: often: hypoglycemia, weight gain.
Visual disorders: very rarely: visual impairment and accommodation disorders.
Disorders of the blood and lymphatic system: rarely: thrombocytopenia, thrombocytopenic purpura, leukocytopenia; very rare: leukopenia, agranulocytosis, erythropenia, hemolytic anemia or pancytopenia, aplastic anemia, bone marrow aplasia, eosinophilia and bleeding disorders.
Gastrointestinal disorders: uncommon: nausea, heartburn, anorexia, belching, vomiting, metallic taste in the mouth, feeling of heaviness and fullness in the stomach, abdominal pain and diarrhea; rarely – pancreatitis.
Disorders of the liver and biliary tract: very rarely: increased activity of liver enzymes (AST, ALT), cholestasis, cholestatic hepatitis, granulomatous hepatitis and bilirubinemia. In some cases, hepatitis, elevated liver enzymes and/or cholestasis and jaundice may lead to life-threatening liver failure, but may resolve after discontinuation of glibenclamide.
Renal and urinary tract disorders: very rarely: increased diuresis, transient proteinuria.
Disorders of the skin and subcutaneous tissues: rarely: skin itching; hives; erythema nodosum; erythematous, maculopapular or bullous rash; psoriasis-like skin reactions.
Immune system disorders: very rarely, reactions in the form of urticaria can initiate the development of severe conditions, accompanied by shortness of breath and a decrease in blood pressure until life-threatening shock occurs. Isolated cases of severe generalized allergic reactions with skin rash, joint pain, fever, protein in the urine and jaundice have been described. If symptoms of hives appear, you should consult a doctor immediately. Cross-allergy with other sulfonylurea derivatives and sulfonamides is possible.
In some cases, it is possible to develop allergic vasculitis, in some cases life-threatening.
Other side effects observed in isolated cases; include photosensitivity; hyponatremia; porphyria cutanea tarda; pellagra-like symptoms. It is possible to develop an acute reaction of alcohol intolerance after drinking it, which is expressed by complications from the circulatory and respiratory organs (disulfiram-like reaction: vomiting, feeling of heat in the face and upper body, tachycardia, dizziness, headache).
Interaction
Interaction
Glibenclamide is metabolized by CYP2C9, which should be taken into account when used concomitantly with CYP2C9 inducers or inhibitors.
An increase in the hypoglycemic effect of glibenclamide is observed with the simultaneous use of angiotensin-converting enzyme inhibitors, anabolic agents and male sex hormones, other oral hypoglycemic drugs (for example, acarbose, biguanides) and insulin, non-steroidal anti-inflammatory drugs (NSAIDs), azapropazone. beta-blockers, guanethidine, quinine, quinolone derivatives, chloramphenicol, clofibrate, coumarin derivatives, disopyramide, fenfluramine, pheniramidol, fluoxetine, monoamine oxidase inhibitors. antifungals (miconazole, fluconazole), para-aminosalicylic acid, pentoxifylline (in large doses administered parenterally), perhexiline, pyrazolones derivatives, phenylbutazones, phosphamides (for example, cyclophosphamide, ifosfamide, trofosfamide), probenecid, salicylates, sulfinpyrazone, sulfonamides, tetracyclines, clarithromycin and tritoqualine.
Urine acidifying agents (ammonium chloride, calcium chloride) enhance the effect of glibenclamide by reducing the degree of its dissociation and increasing its reabsorption. The hypoglycemic effect of glibenclamide may be reduced with simultaneous use of barbiturates, isoniazid, cyclosporine, diazoxide, glucocorticosteroids, glucagon, epinephrine, nicotinates (in large doses), phenytoin, phenothiazines, rifampicin, ritordin, clonidine, thiazide diuretics, acetazole amide, estrogens (for example, oral hormonal contraceptives), iodine-containing thyroid hormone preparations, slow calcium channel blockers, sympathomimetic agents and lithium salts.
When used simultaneously with pentamidine, in isolated cases a pronounced decrease or increase in the concentration of glucose in the blood is possible.
H2-histamine receptor blockers, clonidine and reserpine can both enhance and weaken the hypoglycemic effect of glibenclamide.
Under the influence of sympatholytic agents such as beta-blockers, clonidine, guanethidine and reserpine, signs of adrenergic counterregulation in response to hypoglycemia may be reduced or absent.
Single or chronic alcohol consumption can either enhance or weaken the hypoglycemic effect of glibenclamide.
Glibenclamide can enhance or weaken the effects of coumarin derivatives. Glibenclamide may increase plasma concentrations of cyclosporine and potentially lead to increased toxicity; therefore, concentration monitoring and dose adjustment of cyclosporine is recommended when used concomitantly with glibenclamide.
When using glibenclamide simultaneously with bosentan, an increase in cases of increased activity of liver enzymes was noted, because Glibenclamide and bosentan inhibit the transfer of bile acids from liver cells, which leads to their intracellular accumulation and increased cytotoxic effect. In this regard, the simultaneous use of glibenclamide and bosentan is contraindicated.
Medicines that inhibit bone marrow hematopoiesis increase the risk of myelosuppression.
Overdose
Overdose
In case of overdose, hypoglycemia may develop. This condition can be protracted and contribute to the development of severe conditions, including comatose, life-threatening or fatal. In diabetic polyneuropathy or with concomitant treatment with sympatholytic drugs (see section “Interaction with other drugs”), typical precursors of hypoglycemia may be mild or absent altogether.
Symptoms of hypoglycemia: severe hunger, sudden profuse sweating, palpitations, pallor and decreased skin temperature, paresthesia of the oral mucosa, trembling, general anxiety, headache, pathological drowsiness, sleep disorders, feelings of fear, impaired coordination of movements, temporary neurological disorders (for example, visual and speech disorders, manifestations of paresis and paralysis, or altered perception of sensations). As hypoglycemia progresses, loss of self-control and consciousness is possible, and a predisposition to seizures develops.
Treatment: For mild or moderate hypoglycemia, it is necessary to take dextrose (glucose) or a sugar solution orally.
In case of severe hypoglycemia, accompanied by loss of consciousness, a 40% dextrose solution or glucagon is administered intravenously, intramuscularly, or subcutaneously. After regaining consciousness, the patient should be given food rich in carbohydrates to avoid the recurrence of hypoglycemia.
Storage conditions
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 ° C.
Keep out of the reach of children.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
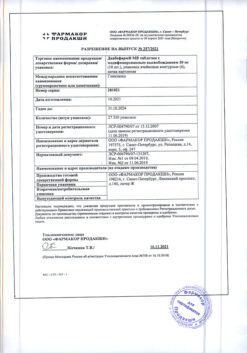
Farmasintez-Tyumen, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 ° C. Store out of the reach of children. |
| Manufacturer | Pharmasintez-Tyumen, Russia |
| Medication form | pills |
| Brand | Pharmasintez-Tyumen |
Related products
Buy Statiglin, tablets 1,75mg 120 pcs with delivery to USA, UK, Europe and over 120 other countries.