No products in the cart.
Description
Pharmacodynamics
Antitumor drug, protein tyrosine kinase inhibitor.
Dazatinib inhibits BCR-ABL and SRC family tyrosine kinase as well as many other oncogenic kinases, including c-KIT, ephrin receptor kinase (ERN) and PDGFβ receptor. Dasatinib binds to active and inactive forms of the BCR-ABL enzyme and inhibits it at subnanomolar concentrations (0.6-0.8 nmol/mL).
Dazatinib is active under in vitro conditions in leukemia cell models against both imatinib-sensitive and imatinib-resistant cells. Dasatinib overcomes resistance to imatinib associated with hyperexpression of BCR-ABL, mutations of BCR-ABL kinase domain, activation of alternative mechanisms inducing SRC family kinases (LYN, ISK) and hyperexpression of multiple drug resistance gene.
Pharmacokinetics
After oral administration, absorption is rapid. Cmax of dasatinib is reached in 0.5-3 hours. AUC and excretion are dose-dependent over a dose range of 25 to 120 mg 2 times/day. When a single dose of 100 mg of dasatinib is taken 30 min after a high-fat meal, there is a 14% increase in the average AUC; after a low-fat meal, there is a 21% increase. Food intake has no significant effect on absorption.
The apparent Vd of dasatinib is 2505 L, indicating significant distribution in the extravascular space. The binding of dasatinib is 96%.
Dazatinib is metabolized primarily with the participation of the CYP3A4 isoenzyme. After oral administration of 100 mg [14C]- dasatinib by healthy volunteers, unchanged dasatinib accounted for 29% of plasma radioactivity. Based on plasma concentrations and in vitro activity, we can assume that metabolites do not play a major role in the pharmacological effects of dasatinib.
Extracted mainly by the intestine, mainly as metabolites. After a single oral administration of [14C]-dazatinib, 4% and 85% are excreted by the kidneys and intestine, respectively, within 10 days. Unchanged dasatinib is 0.1% and 19% of the dose excreted by the kidneys and intestine, respectively; the rest of the dose is represented by metabolites.
The mean total terminal T1/2 of dasatinib in patients is 5-6 h.
The pharmacokinetics of dasatinib were studied in 8 patients with moderate hepatic impairment after a single dose of 50 mg and in 5 patients with severe hepatic impairment after a single dose of 20 mg compared with pharmacokinetics in healthy volunteers after a dose of 70 mg. The Cmax and AUC values for dasatinib were 47% and 8% lower, respectively, for moderate hepatic impairment compared to values in healthy volunteers. In patients with severe hepatic impairment, reductions in Cmax and AUC values for dasatinib were as low as 43% and 28%, respectively.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Filmed film-coated tablets
1 tablet contains:
The active ingredients: dasatinib 50 mg.
Auxiliary substances: lactose monohydrate, microcrystalline cellulose, hyprolose, croscarmellose sodium, magnesium stearate, opadray white (titanium dioxide, hypromellose-6cP, macrogol 400).
There are 60 tablets in a polyethylene bottle. In a carton pack of 1 vial.
How to take, the dosage
How to take, the dosage
It is taken orally. The initial dose is 100 mg once a day. Further the dose is adjusted depending on the indication, the therapy regimen, the effectiveness of treatment, the degree of toxicity of side effects.
Interaction
Interaction
Dazatinib is a substrate of the CYP3A4 isoenzyme. CYP3A4 isoenzyme inhibitors (e.g., ketoconazole, itraconazole, erythromycin, clarithromycin, ritonavir, atazanavir, indinavir, nelfinavir, saquinavir, telithromycin, grapefruit juice) may increase the plasma concentration of dasatinib, so their co-administration with dasatinib should be avoided. Patients in whom systemic administration of a potent CYP3A4 isoenzyme inhibitor cannot be avoided should be closely monitored for timely signs of toxicity.
CYP3A4 isoenzyme inducers can decrease the plasma concentration of dasatinib. Co-administration of potent CYP3A4 isoenzyme inducers with dasatinib should be avoided. Patients taking CYP3A4 isoenzyme inducers (e.g., dexamethasone, phenytoin, carbamazepine; rifampicin, phenobarbital or preparations of St. John’s wort) should be treated with drugs that have no (or only minimal) ability to induce this isoenzyme instead.
Long-term inhibition of gastric acid secretion by histamine H2 receptor blockers and proton pump inhibitors (e.g., famotidine and omeprazole) may reduce dasatinib concentrations. Co-administration of these drugs and dasatinib is not recommended. Antacids can be used as an alternative.
Dazatinib is an inhibitor of CYP3A4 isoenzyme, therefore its co-administration with CYP3A4 isoenzyme substrates may increase the effect of this substrate. CYP3A4 substrates with a narrow therapeutic range, such as alfentanil, astemizole, terfenadine, cisapride, cyclosporine, fentanyl, pimozide, quinidine, sirolimus, tacrolimus and ergot alkaloids (ergotamine, dihydroergotamine) should be used with caution in patients receiving dasatinib.
Special Instructions
Special Instructions
With caution, use with hepatic insufficiency, concomitantly with anticoagulants and drugs affecting platelet function; with prolongation of the QT interval or risk of its prolongation (also with concomitant use of QT interval prolonging drugs); concomitantly with CYP3A4 isoenzyme substrates, concomitant use with inhibitors or inducers of CYP3A4 isoenzyme with a narrow therapeutic range.
During treatment, a complete clinical blood count should be performed weekly for the first 2 months of treatment and then monthly or more frequently, as clinically indicated. The inhibition of medullary hematopoiesis is usually reversible and resolves with temporary withdrawal or reduction of the dosage of dasatinib.
Most cases of bleeding during dasatinib use have been associated with severe thrombocytopenia. Severe cerebral hemorrhage, including fatal, has been reported in less than 1% of patients receiving dasatinib; severe gastrointestinal bleeding has been reported in 4% of patients. Other severe bleeding has been reported in 2% of patients.
In case of dyspnea or dry cough, chest radiological monitoring is necessary.
If a patient has any treatment-related symptoms, such as dizziness or visual disturbances, which may affect his or her ability to concentrate and react quickly, it is recommended that the patient not drive or perform potentially hazardous activities that require increased concentration and quick psychomotor reactions.
Contraindications
Contraindications
Side effects
Side effects
Most common ( > 20%): fluid retention, diarrhea, headache, skin rash, nausea, hemorrhage, fatigue, dyspnea, myalgia, infectious complications, vomiting, cough, abdominal pain, fever, febrile neutropenia due to dasatinib (5%).
Infections and invasions: very often – infections (including bacterial, viral and fungal), pneumonia (including bacterial, viral and fungal), upper respiratory tract infections, herpetic infections, enterocolitis, sepsis (including fatal).
Hematopoietic system: frequently – febrile neutropenia, pancytopenia; rarely – erythroblastopenia.
With the blood coagulation system: very common – bleeding.
Immune system disorders: infrequent hypersensitivity reactions (including erythema nodosum).
Nervous system disorders: very common – headache; common – insomnia, depression, neuropathy (including peripheral neuropathy), dizziness, perversion of taste, somnolence; infrequent – anxiety, emotional lability, psychosis, decreased libido, brain hemorrhage, tremor, fainting, amnesia; rare – seizures, cerebral circulatory disorders (stroke), transient brain circulatory disorders.
An organ of vision: often – visual impairment, dry eyes; infrequently – conjunctivitis.
Hearing organ: often – tinnitus; infrequent – vertigo.
Cardiovascular system disorders: frequent – flushes, increased BP, pericardial effusion, arrhythmia (including tachycardia), congestive heart failure/myocardial dysfunction, palpitations; infrequent – prolongation of QT interval on ECG, angina pectoris, cardiomegaly, decreased BP, thrombophlebitis, pericarditis, ventricular arrhythmia (including ventricular tachycardia), myocardial infarction; rare – pulmonary heart, myocarditis, acute coronary syndrome, skin marbling.
Respiratory system: very common – pleural effusion, dyspnea, cough; common – pulmonary infiltrates, pulmonary edema, pneumonitis, pulmonary hypertension; infrequent – bronchial asthma, bronchospasm; rare – acute respiratory distress syndrome.
Digestive system disorders: very common – diarrhea, nausea, vomiting, abdominal pain; common – disorder, appetite, mucous membrane inflammation (including mucositis/stomatitis), gastrointestinal bleeding, dyspepsia, abdominal bloating, constipation, gastritis, oral mucosa lesions, colitis (including neutropenic colitis), anorexia; infrequent – dysphagia, ascites, anal fissures, upper gastrointestinal ulcers, pancreatitis, esophagitis, cholestasis, cholecystitis, hepatitis.
Skin disorders: very common – skin rash; common – itching, acne, alopecia, dry skin, hyperhidrosis, urticaria, dermatitis (including eczema); infrequent – skin ulcers, bullous dermatosis, pigmentation disorders, nail lesions, photosensitization, acute Febrial neutrophilic dermatosis, panniculitis, palmar and plantar erythrodisesthesia syndrome.
Muscular system disorders: very common – musculoskeletal pain; common – arthralgia, myositis, muscle weakness, musculoskeletal stiffness; infrequent – increase of CPK activity in blood, rhabdomyolysis; rare – tendinitis.
Arenal system disorders: infrequent – renal failure, rapid urination, proteinuria.
Reproductive system disorders: infrequent – gynecomastia, menstrual disorders.
Others: very frequently – fluid retention, localized edema of subcutaneous fat of different localization, edema of the tongue, edema of the lips, edema of the conjunctiva, fatigue, fever; frequently – asthenia, pain, pain in the chest, disseminated edema, chills, hyperuricemia; rarely – malaise, intolerance of high and low temperatures, tumor lysis syndrome, hypoalbuminemia.
Overdose
Overdose
An overdose of Sprycel® has been reported in 2 patients who took 280 mg of the drug daily for a week, which resulted in a significant decrease in platelet count.
In case of overdose close monitoring of patients is required to control the degree of myelosuppression; symptomatic therapy is indicated if necessary.
Pregnancy use
Pregnancy use
The use is contraindicated in pregnancy and during lactation (breastfeeding).
Patients should use reliable contraception during treatment and for at least 3 months after.
Additional information
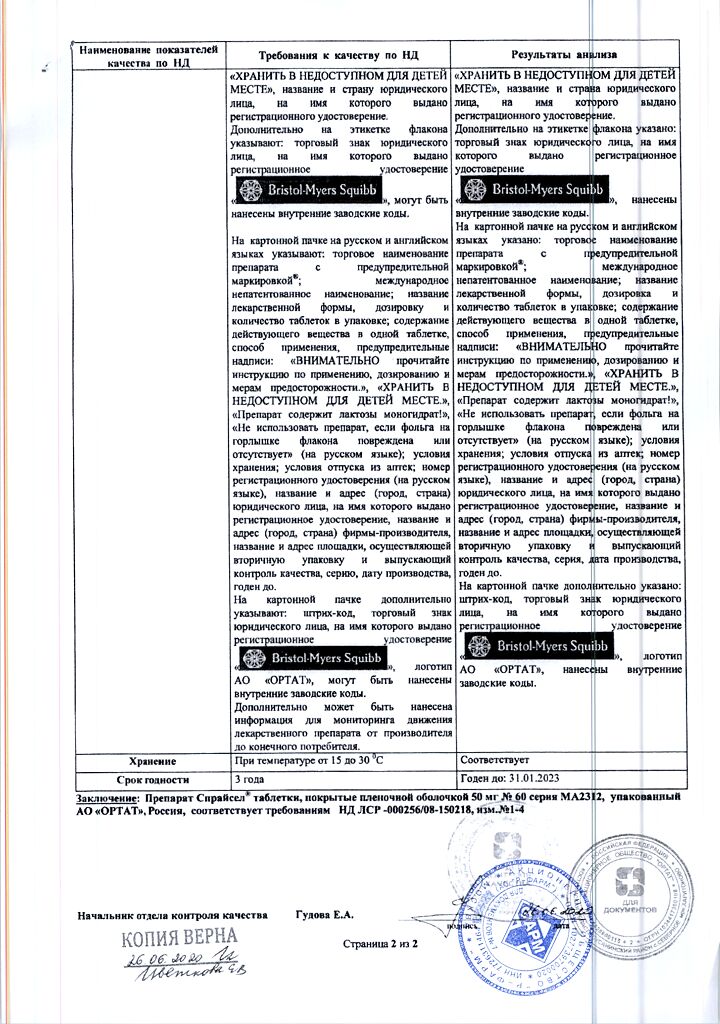
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At 15-30 °C |
| Manufacturer | AstraZeneca Pharmaceuticals LP, USA |
| Medication form | pills |
| Brand | AstraZeneca Pharmaceuticals LP |
Related products
Buy Spraysel, 50 mg 60 pcs. with delivery to USA, UK, Europe and over 120 other countries.