No products in the cart.
Spiriva, 2.5 mcg/dose 4 ml (60 doses) cartridges complete with inhaler
€61.07 €50.89
Description
Tiotropium bromide is a long-acting m-cholinoblocker. The drug has equal affinity for M 1 -M 5 muscarinic receptor subtypes. The result of inhibition of M 3 -receptors in the airways is relaxation of the smooth muscles. The bronchodilator effect is dose-dependent and lasts for at least 24 hours. The considerable duration of action is probably due to very slow dissociation of the drug from M 3 -receptors; the half-dissociation period is significantly longer than that of ipratropium bromide.
When administered by inhalation, tiotropium bromide, as an N-quaternary ammonium derivative, has a local selective effect (on the bronchi), while at therapeutic doses does not cause systemic m-cholinoblocking side effects. Dissociation from M 2 -receptors is faster than from M 3 -receptors, indicating a predominance of selectivity for M 3 receptor subtype over M 2 -receptors. High affinity to the receptors and slow dissociation of the drug from binding to the receptors are responsible for the pronounced and prolonged bronchodilator effect in patients with chronic obstructive pulmonary disease (COPD).
The bronchodilation that develops after inhalation of tiotropium bromide is due primarily to local (airway) rather than systemic action.
In clinical studies, Spiriva Respimat once daily has been shown to significantly improve (compared to placebo) lung function (1-second forced expiratory volume SPE1 and forced vital capacity FEL) within 30 minutes of the first dose. The improvement in lung function persists for 24 h at equilibrium concentration.
Pharmacodynamic equilibrium was achieved within one week. Spiriva Respimat significantly improved morning and evening peak expiratory volume velocity (PEFV) measured by patients. Use of Spiriva Respimat led to a decrease (compared with placebo) in the use of a bronchodilator as an emergency aid. The bronchodilator effect of the drug persisted for 48 weeks of use of the drug; no signs of habituation were noted.
A combined data analysis of two randomized, placebo-controlled, crossover clinical trials showed that the bronchodilator effect of Spiriva Respimat (5 mcg) after a 4-week treatment period was quantitatively greater than that of Spiriva (18 mcg).
In long-term (12-month) studies, Spiriva Respimat was found to significantly reduce shortness of breath; improve quality of life; reduce the psychosocial impact of COPD and increase activity.
Spiriva Respimat significantly improved overall health (overall score) compared to placebo at the end of two 12-month studies, and this difference was maintained throughout the treatment period; Spiriva Respimat significantly reduced the number of COPD exacerbations, and increased the time to first exacerbation compared to placebo.
Spiriva Respimat has been shown to reduce the risk of COPD exacerbations and significantly reduce hospitalizations.
In a retrospective analysis of selected clinical trials, a statistically non-significant increase, compared to placebo, in the number of deaths in patients with cardiac rhythm disturbances was observed. However, these findings are not statistically confirmed and may be related to heart disease.
Pharmacokinetics
Tiotropium bromide is a quaternary ammonium derivative that is moderately water soluble. Tiotropium bromide is available as an inhalation solution, which is used with the Respimat inhaler. Approximately 40% of the inhaled dose is deposited in the lungs and the remainder enters the gastrointestinal tract. Some of the pharmacokinetic data described below have been obtained using doses in excess of those recommended for treatment.
Absorption
After inhalation of the solution in young healthy volunteers, approximately 33% of the inhaled dose was found to enter the systemic circulation. Food intake does not affect absorption of tiotropium bromide, due to the fact that it is poorly absorbed from the gastrointestinal tract. Absolute bioavailability when oral administration is 2-3%. C max in plasma is observed 5 min after inhalation.
Distribution
The drug’s binding to plasma proteins is 72%; V d is 32 l/kg. At the stage of dynamic equilibrium the peak plasma concentration of tiotropium bromide in patients with COPD is 10.5-11.7 pg/ml in 10 min after the use of the drug in a dose of 5 mcg using Respimat inhaler. At the dynamic equilibrium stage, the lowest plasma concentration was 1.49-1.68 pg/ml. Studies have shown that tiotropium bromide does not penetrate through the HEB.
Metabolism
The degree of biotransformation is insignificant. This is confirmed by the fact that after intravenous administration of the drug in young healthy volunteers, 74% of the substance tiotropium bromide is found unchanged in the urine. Tiotropium bromide is an ester that is cleaved to ethanol-N-methylscopene, and dithienylglycolic acid; these compounds do not bind to muscarinic receptors.
In in vitro studies it has been shown that some portion of the drug (< 20% of the dose after IV administration) is metabolized by cytochrome P450 oxidation followed by conjugation with glutathione to form various metabolites. This mechanism can be inhibited by inhibitors of CYP 2D6 and 3A4 isoenzymes (quinidine, ketoconazole and gestoden). Thus, CYP2D6 and 3A4 are involved in the metabolism of the drug. Tiotropium bromide does not inhibit cytochrome P450 1A1, 1A2, 2B6, 2C9, 2C19, 2D6, 2E1 or 3A in human liver microsomes even in supertherapeutic concentrations.
Elimination
The terminal T 1/2 of tiotropium bromide after inhalation is 5-6 days. Total clearance after IV administration to young healthy volunteers was 880 mL/min, with an individual variability of 22%. Tiotropium bromide after IV administration is mainly excreted unchanged by the kidneys (74%). After inhalation of the solution renal excretion is 20.1-29.4%, the remaining unabsorbed part is excreted through the intestine. Renal clearance of tiotropium bromide exceeds creatinine clearance, indicating its tubular secretion. After long-term inhaled administration of the drug once daily in patients with COPD, pharmacokinetic equilibrium is reached on day 7; no further cumulation is observed.
Tiotropium bromide has linear pharmacokinetics within therapeutic limits after IV administration, inhalation of dry powder and inhalation of solution.
Pharmacokinetics in special clinical cases
In elderly patients
In the elderly, there is decreased renal clearance of tiotropium bromide (326 mL/min in patients with COPD under 58 years of age and 163 mL/min in patients with COPD over 70 years), which may be due to decreased renal function. Urinary excretion of tiotropium bromide after inhaled administration decreased from 14% in young healthy volunteers to approximately 7% in COPD patients, but plasma concentrations in elderly COPD patients were not significantly altered when inter- and intraindividual variability were considered (AUC increased by 43% after inhalation of dry powder).
In patients with impaired renal function
Small renal dysfunction (CK 50-80 ml/min), which may be seen in elderly patients, is accompanied by a slight increase in plasma concentration of tiotropium bromide (AUC increased by 39% after intravenous infusion). In patients with COPD and moderate or significant renal impairment (CK < 50 ml/min), intravenous administration of tiotropium bromide resulted in a twofold increase in plasma concentration (AUC increased by 82%); a similar increase in plasma concentration was observed after inhalation of dry powder.
In patients with impaired hepatic function
Hepatic impairment is not thought to have a significant effect on the pharmacokinetics of tiotropium bromide since tiotropium bromide is primarily excreted by the kidneys.
Indications
Indications
As maintenance therapy in patients with COPD, including chronic bronchitis and emphysema (with persistent shortness of breath and to prevent exacerbations).
Pharmacological effect
Pharmacological effect
Tiotropium bromide is a long-acting m-anticholinergic blocker. The drug has the same affinity for the M 1 -M 5 subtypes of muscarinic receptors. The result of inhibition of M 3 receptors in the respiratory tract is relaxation of smooth muscles. The bronchodilator effect depends on the dose and lasts for at least 24 hours. The significant duration of action is probably due to the very slow dissociation of the drug from M 3 receptors; The half-dissociation period is significantly longer than that of ipratropium bromide.
When administered by inhalation, tiotropium bromide, as an N-quaternary ammonium derivative, has a local selective effect (on the bronchi), while in therapeutic doses it does not cause systemic m-anticholinergic side effects. Dissociation from M 2 receptors occurs faster than from M 3 receptors, which indicates the predominance of selectivity for the M 3 receptor subtype over M 2 receptors. High affinity for receptors and slow dissociation of the drug from connection with receptors determine a pronounced and long-lasting bronchodilator effect in patients with chronic obstructive pulmonary disease (COPD).
Bronchodilation that develops after inhalation of tiotropium bromide is primarily due to local (on the respiratory tract) rather than systemic effects.
In clinical studies, it was shown that the use of Spiriva Respimat 1 time / day leads to a significant improvement (compared to placebo) in lung function (forced expiratory volume in 1 second FEV1 and forced vital capacity FVC) within 30 minutes after the first dose. Improvement in lung function persists for 24 hours at steady state.
Pharmacodynamic equilibrium was achieved within one week. Spiriva Respimat significantly improved morning and evening peak expiratory volume flow (PEEF) measured by patients. Spiriva Respimat resulted in a reduction (compared with placebo) in rescue bronchodilator use. The bronchodilator effect of the drug persists for 48 weeks of use of the drug; There are no signs of addiction.
Analysis of combined data from two randomized, placebo-controlled, crossover clinical trials showed that the bronchodilator effect of Spiriva Respimat (5 mcg) after a 4-week treatment period was quantitatively greater than the effect of Spiriva (18 mcg).
In long-term (12-month) studies, Spiriva Respimat was found to significantly reduce shortness of breath; improves quality of life; reduces the psychosocial impact of COPD and increases activity.
Spiriva Respimat significantly improved overall health status (total score) compared with placebo at the end of two 12-month studies, a difference that was maintained throughout the treatment period; Spiriva Respimat significantly reduced the number of exacerbations of COPD and increased the period until the first exacerbation compared to placebo.
Spiriva Respimat has been shown to reduce the risk of exacerbation of COPD and significantly reduce the number of hospitalizations.
In a retrospective analysis of individual clinical studies, a statistically insignificant increase, compared with placebo, in the number of deaths in patients with cardiac arrhythmias was observed. However, these data are not statistically confirmed and may be associated with heart disease.
Pharmacokinetics
Tiotropium bromide is a quaternary ammonium derivative, sparingly soluble in water. Tiotropium bromide is available as an inhalation solution, which is used with the Respimat inhaler. Approximately 40% of the inhalation dose is deposited in the lungs, the rest enters the gastrointestinal tract. Some pharmacokinetic data described below were obtained using doses higher than those recommended for treatment.
Suction
After inhalation of the solution by young healthy volunteers, it was found that about 33% of the inhalation dose enters the systemic circulation. Eating does not affect the absorption of tiotropium bromide, due to the fact that it is poorly absorbed from the gastrointestinal tract. Absolute bioavailability when taken orally is 2-3%. Cmax in plasma is observed 5 minutes after inhalation.
Distribution
The binding of the drug to plasma proteins is 72%; Vd – 32 l/kg. At the dynamic equilibrium stage, the peak plasma concentration of tiotropium bromide in patients with COPD is 10.5-11.7 pg/ml 10 minutes after administration of the drug at a dose of 5 mcg using the Respimat inhaler. At the stage of dynamic equilibrium, the lowest plasma concentration was 1.49-1.68 pg/ml. Studies have shown that tiotropium bromide does not cross the BBB.
Metabolism
The degree of biotransformation is insignificant. This is confirmed by the fact that after intravenous administration of the drug to young healthy volunteers, 74% of the substance tiotropium bromide in unchanged form is found in the urine. Tiotropium bromide is an ester that splits into ethanol-N-methylscopine and dithienylglycolic acid; these compounds do not bind to muscarinic receptors.
In vitro studies have shown that some of the drug (<20% of the dose after intravenous administration) is metabolized by oxidation by cytochrome P450, followed by conjugation with glutathione and the formation of various metabolites. This mechanism can be inhibited by inhibitors of the CYP 2D6 and 3A4 isoenzymes (quinidine, ketoconazole and gestodene). Thus, CYP2D6 and 3A4 are involved in drug metabolism. Tiotropium bromide, even at supratherapeutic concentrations, does not inhibit cytochrome P450 1A1, 1A2, 2B6, 2C9, 2C19, 2D6, 2E1 or 3A in human liver microsomes.
Removal
The terminal half-life of tiotropium bromide after inhalation is 5-6 days. The total clearance after intravenous administration of the drug to young healthy volunteers was 880 ml/min, with an individual variability of 22%. Tiotropium bromide after intravenous administration is mainly excreted unchanged by the kidneys (74%). After inhalation of the solution, renal excretion is 20.1-29.4%, the remaining unabsorbed portion is excreted through the intestine. The renal clearance of tiotropium bromide exceeds the clearance of creatinine, indicating its tubular secretion. After long-term inhalation administration of the drug 1 time per day in patients with COPD, pharmacokinetic equilibrium is achieved on day 7; at the same time, no further cumulation is observed.
Tiotropium bromide has linear pharmacokinetics within therapeutic limits after intravenous administration, dry powder inhalation and solution inhalation.
Pharmacokinetics in special clinical situations
In elderly patients
In old age, there is a decrease in the renal clearance of tiotropium bromide (326 ml/min in patients with COPD under the age of 58 years and 163 ml/min in patients with COPD over 70 years of age), which may be explained by a decrease in renal function. Urinary excretion of tiotropium bromide after inhalation is reduced from 14% in young healthy volunteers to approximately 7% in patients with COPD, but plasma concentrations in elderly patients with COPD did not change significantly when inter- and intra-individual variability was taken into account (AUC increased by 43% after inhalation of dry powder).
In patients with impaired renal function
Minor impairment of renal function (creatinine clearance 50-80 ml/min), which can be observed in elderly patients, is accompanied by a slight increase in plasma tiotropium bromide concentrations (after IV infusion, AUC increased by 39%). In patients with COPD and moderate or severe renal impairment (creatinine clearance < 50 ml/min), intravenous tiotropium bromide resulted in a twofold increase in plasma concentrations (AUC increased by 82%), and a similar increase in plasma concentrations was observed after inhalation of dry powder.
In patients with impaired liver function
It is assumed that hepatic impairment does not have a significant effect on the pharmacokinetics of tiotropium bromide, since tiotropium bromide is primarily excreted by the kidneys.
Special instructions
Special instructions
The drug Spiriva Respimat, as a bronchodilator used once a day for maintenance treatment, should not be used as initial therapy for acute attacks of bronchospasm, that is, in emergency cases.
Immediate hypersensitivity reactions may occur after using the drug.
Spiriva Respimat, like other anticholinergic drugs, should be used with caution in patients with angle-closure glaucoma, prostatic hyperplasia or bladder neck obstruction.
Inhalation of the drug may cause bronchospasm.
In case of moderate or severe renal failure (creatinine clearance <50 ml/min), the drug should be taken under close supervision, as with all drugs excreted primarily by the kidneys.
Before use, patients should be familiar with the instructions for use.
Do not allow the solution or aerosol to get into your eyes. Pain or discomfort in the eyes, blurred vision, visual halos combined with redness of the eyes, swelling of the conjunctiva and cornea can be symptoms of acute angle-closure glaucoma. If any combination of these symptoms develops, you should immediately consult a specialist. Miotic eye drops are not considered an effective treatment.
Spiriva Respimat should not be used more than once a day.
Spiriva cartridges should only be used with the Respimat inhaler.
Impact on the ability to drive vehicles and operate machinery
No studies have been conducted to study the effect on the ability to drive vehicles and operate machinery. Caution should be exercised when performing these activities as dizziness or blurred vision may occur.
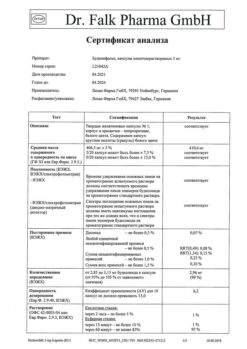
Active ingredient
Active ingredient
Tiotropium bromide
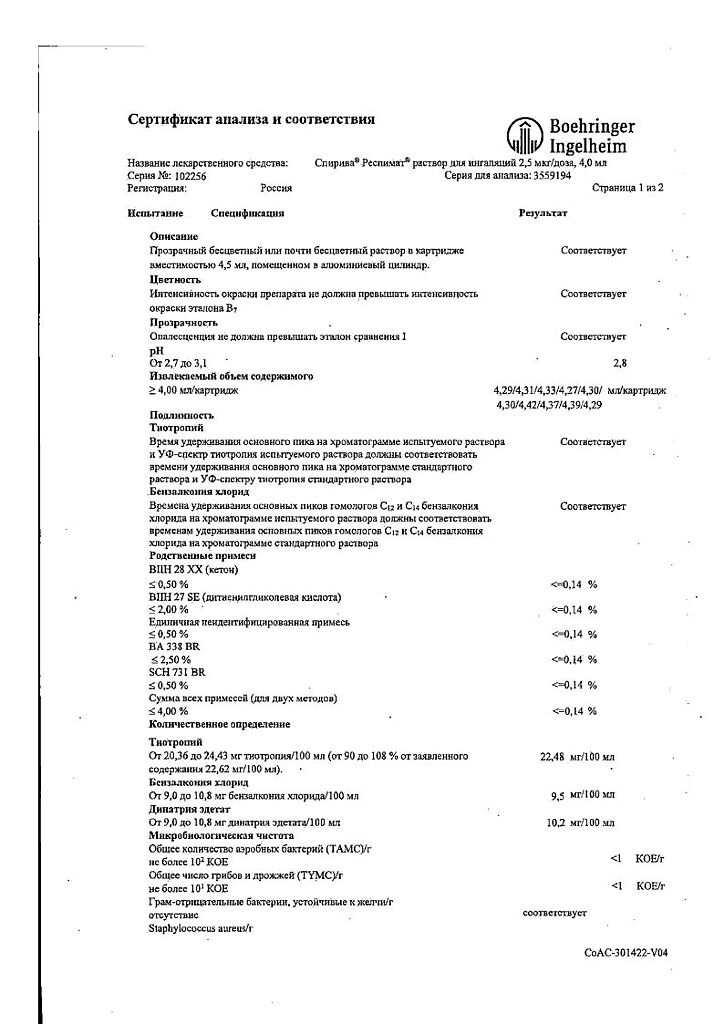
Composition
Composition
1 dose of solution for inhalation contains:
Active ingredient:
tiotropium bromide monohydrate – 3.1235 mcg, which corresponds to the content of tiotropium – 2.5 mcg.
Excipients:
benzalkonium chloride – 1.105 mcg,
disodium edetate – 1.105 mcg,
hydrochloric acid 1M – up to pH 2.8 – 3.0,
water – up to 11.05 mg.
Pregnancy
Pregnancy
Pregnancy
There are no clinical data on the safety and effectiveness of Spiriva Respimat during pregnancy.
In preclinical studies, there were no indications of direct or indirect adverse effects on pregnancy, embryo/fetal development, childbirth or postnatal development.
Lactation
There are no clinical data on the safety and effectiveness of tiotropium bromide during breastfeeding.
The drug should not be used in pregnant or breastfeeding women unless the potential benefit to the mother outweighs the potential risk to the fetus and child. During the period of use of the drug, it is necessary to stop breastfeeding the child.
Contraindications
Contraindications
Age under 18 years, hypersensitivity to the components of the drug Spiriva.
Side Effects
Side Effects
From the gastrointestinal tract: dry mouth (usually mild, often disappears with continued treatment), constipation.
From the respiratory system: cough, local irritation, possible development of bronchospasm, as well as when taking other inhalation agents.
Other: tachycardia, difficulty or retention of urination (in men with predisposing factors), angioedema, blurred vision, acute glaucoma (associated with anticholinergic effects).
Interaction
Interaction
Concomitant use with other anticholinergic drugs is not recommended.
It is possible to use tiotropium bromide in combination with other drugs commonly used to treat COPD – sympathomimetics, methylxanthines, oral and inhaled steroids.
Overdose
Overdose
Symptoms: possible dry mouth, impaired accommodation, increased heart rate.
Treatment: symptomatic therapy.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C (do not freeze). Do not freeze.
Manufacturer
Manufacturer
Boehringer Ingelheim Pharma GmbH & Co.KG, Germany
Additional information
| Conditions of storage | At a temperature not exceeding 25 °C (do not freeze). Do not expose to freezing. |
|---|---|
| Manufacturer | Boehringer Ingelheim Pharma GmbH & Co. |
| Medication form | solution for inhalation |
| Brand | #Н/Д |
Related products
Buy Spiriva, 2.5 mcg/dose 4 ml (60 doses) cartridges complete with inhaler with delivery to USA, UK, Europe and over 120 other countries.