No products in the cart.
Simdax, 2.5mg/ml 5 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacodynamics
Levosimendan increases calcium sensitivity of contractile proteins by binding to myocardial troponin C (calcium-dependent binding), increases cardiac contractility, opens ATP-sensitive potassium channels in vascular smooth muscle and induces dilation of arteries, including coronary, and veins. In vitro selective inhibitory activity of levosimendan against phosphodiesterase III has been demonstrated.
The significance of this effect when using the drug in therapeutic concentrations has not been established. In patients with chronic heart failure, the calcium-dependent positive inotropic and vasodilatory effect of levosimendan leads to an increase in heart force and a decrease in preload and postload without worsening diastolic function. Activates ischemic myocardium in patients after percutaneous transluminal coronary angioplasty or thrombolysis.
Hemodynamic studies in healthy volunteers and in patients with chronic heart failure have shown dose-dependent effects of loading dose (3 µg/kg body weight) and prolonged infusion (0.05 to 0.2 µg/kg body weight per 1 minute). Levosimendan increases cardiac output, stroke volume, increases ejection fraction and heart rate (HR), reduces systolic and diastolic blood pressure (BP), pulmonary capillary wedging pressure, right atrial pressure and total peripheral vascular resistance.
A single active metabolite is produced when the drug is administered at the recommended dose and produces hemodynamic effects similar to those of levosimendan. They persist for 7-9 days after cessation of 24-hour levosimendan infusion.
Levosimendan infusion causes increased coronary blood flow in patients who have undergone coronary artery surgery and improves myocardial perfusion in patients with chronic heart failure.
These positive effects are not accompanied by a significant increase in myocardial oxygen consumption. Significantly reduces endothelin 1 in patients with chronic heart failure. The drug does not increase plasma catecholamine concentrations if the recommended rate of administration is followed.
The REVIVE I and REVIVE II programs.
The REVIVE programs compared the efficacy of levosimendan and placebo in combination with standard therapy in patients with acute decompensated chronic heart failure with left ventricular ejection fraction ≤35% and dyspnea at rest. Continuation of previous therapy was allowed with the exception of intravenous administration of milrinone.
The results showed that most patients improved; a smaller number of patients deteriorated. There was a slight increase in the incidence of death at day 90 in the Simdax group compared to the control group (15% and 12%, respectively). SURVIVE baseline systolic BP has been shown.
A double-blind, multicenter comparison study of levosimendan and dobutamine in 1,327 patients with acute decompensated chronic heart failure and ineffective prior therapy with diuretics and vasodilators compared 180-day mortality rates. In percent incidence, the advantage was with levosimendan on day 5 (4% levosimendan, 6% dobutamine). This advantage was maintained through day 31 (12% levosimendan, 14% dobutamine), especially in those patients who had initially received beta-adrenoblockers. Patients with baseline lower BP had worse mortality rates in both groups.
LIDO
In a double-blind, multicenter study of 203 patients with severe chronic heart failure with low cardiac output (ejection fraction 15 mm Hg) who needed inotropic therapy, they received levosimendan (a loading dose of 24 mcg/kg for 10 min, followed by a continuous infusion of 0.1-0.2 µg/kg/min for 24 hours) or dobutamine 5-10 µg/kg/min for 24 hours. An increase in cardiac output of >30% and a concomitant reduction in pulmonary capillary congestion pressure of 25% or more after 24 h was achieved in 28% of patients receiving levosimendan and in 15% of patients receiving dobutamine (p=0.025). Dyspnea decreased in 68% and 59% of patients, respectively, and fatigue decreased in 63% and 47%. The 31-day mortality rate was 7.8% in the levosimendan group and 17% in the dobutamine group.
RUSSLAN
In a double-blind, multicenter study whose primary objective was to examine safety, 504 patients with decompensated chronic heart failure after acute myocardial infarction who needed inotropic therapy received levosimendan or placebo for 6 hours. The groups did not differ significantly in the incidence of arterial hypotension and myocardial ischemia.
In a retrospective analysis of the two LIDO and RUSSLAN studies, no adverse effect of levosimendan on 6-month survival was found.
Pharmacokinetics
The pharmacokinetics of levosimendan at therapeutic doses of 0.05 to 0.2 µg/kg/min. is linear.
Distribution
The volume of distribution of levosimendan (Vss) is approximately 0.2 L/kg. Levosimendan is 97-98% bound to plasma proteins, mainly to albumin. The binding of active metabolites (OR-1855 and OR-1896) to proteins is 39% and 42%, respectively.
Metabolism
Levosimendan is mainly metabolized by conjugation with cyclic or N-acetylated cysteinylglycine and cysteine conjugates. Only about 5% of the dose of levosimendan is metabolized in the small intestine by oxidation to aminophenylpyridazinone (OR-1855), which after reabsorption into the systemic bloodstream is biotransformed in plasma by N-acetyltransferase to the active metabolite OR-1896. The rate of acetylation is genetically determined. The “fast acetylators” have slightly higher concentrations of OR-1896 metabolite than the “slow” ones. However, this is not reflected in the clinically significant hemodynamic effects of the drug at the recommended doses.
Only 2 metabolites, OR-1855 and OR-1896, are detected in significant amounts in the systemic bloodstream. In “slow” acetylators, OR-1855 predominates, and in “fast” – OR-1896. However, the total amount of these metabolites and the frequency of hemodynamic effects are the same in “fast” and “slow” acetylators. These metabolites can have a long-term effect on hemodynamic parameters (within 7-9 days after cessation of a 24-hour infusion of levosimendan).
In vitro, levosimendan and the metabolites OR-1855 and OR-1896, at concentrations produced by the recommended doses of the drug, do not inhibit CYP1A2, CYP 2A6, CYP2C19, CYP2E1, CYP2C9, CYP2D6, or CYP3A4. Levosimendan does not inhibit CYP 1A1, and its metabolism is not affected by CYP3A inhibitors.
Elimination
The clearance of levosimendan is approximately 3.0 ml/min/kg and the elimination half-life is approximately 1 h. Over 95% of the dose of levosimendan is eliminated within 1 week as inactive metabolites. A small part of the dose (Special groups
Children: Few data suggest that pharmacokinetics of levosimendan after single administration in children (aged 3 months to 6 years) is similar to that in adults. Pharmacokinetics of the active metabolite in children has not been studied. Levosimendan should not be used in children.
Patients with impaired renal function: Pharmacokinetics of levosimendan is similar in patients with mild to moderate impaired renal function and in patients on hemodialysis. In patients with severe renal impairment pharmacokinetic parameters may be slightly reduced.
In patients with severe renal impairment and those on hemodialysis, the free fraction of levosimendan is slightly elevated and the AUC (area under the concentration-time curve) of metabolites OR-1855 and OR-1896 is 170% higher. Mild to moderate renal impairment is thought to have less effect on the pharmacokinetics of OR-1855 and OR-1896 metabolites. Levosimendan is not excreted by hemodialysis. Although OR-1855 and OR-1896 metabolites are excreted by hemodialysis, their clearance is low (approximately 8-23 ml/min).
Patients with impaired hepatic function: In patients with mild to moderate hepatic impairment in cirrhosis, the pharmacokinetics and protein binding of levosimendan do not differ from those of healthy preobese patients.
The pharmacokinetics of levosimendan and the metabolites OR-1855 and OR-1896 are similar in healthy preobese and in patients with moderate hepatic impairment (Child-Pugh class B) except that the elimination half-life of these metabolites is slightly longer in moderate hepatic impairment.
In a population-based analysis, age, ethnicity, or gender were not found to affect the pharmacokinetics of levosimendan. However, the volume of distribution and total clearance are influenced by body weight.
Indications
Indications
The short-term treatment of acute decompensation of severe chronic heart failure (CHF) when standard therapy is ineffective and inotropic therapy is needed.
Active ingredient
Active ingredient
Composition
Composition
1 ml of concentrate for preparation of solution for infusion contains:
the active ingredient:
Levosimendan 2.5 mg;
excipients:
povidone for parenteral administration,
citric acid b/w for parenteral administration,
ethanol b/w.
How to take, the dosage
How to take, the dosage
Simdax 2.5 mg/ml concentrate should only be used diluted!
Preparation of infusion solution and infusion rate
To prepare a 0.05 mg/ml infusion solution, 10 ml of levosimendan 2.5 mg/ml concentrate should be diluted in 500 ml of 5% dextrose (glucose) solution. Table 1 shows the infusion rate for loading and maintenance doses of 0.05 mg/ml levosimendan solution as a function of body weight:
To prepare a 0.025 mg/ml infusion solution, 5 ml of levosimendan 2.5 mg/ml concentrate should be diluted in 500 ml of 5% dextrose (glucose) solution.
Table 2 shows the infusion rate for the loading dose and maintenance dose of 0.025 mg/ml of Simdax as a function of body weight:
Simdax Concentrate 2.5 mg/ml is for single use only!
Before infusion, the diluted solution, like other parenteral preparations, should be checked for foreign particles and color changes. During storage the color of the concentrate may change to orange, which is not accompanied by a decrease in the activity of the drug.
Infusion can be performed through peripheral or central veins.
The dose and duration of treatment are chosen individually taking into account the clinical state of the patient and the therapeutic effect.
Treatment starts with a loading dose of 6-12 mcg/kg which is administered for 10 minutes (see Table 1 and 2). A continuous infusion is then given at a rate of 0.1 µg/kg/min. A lower dose of 6 µg/kg is recommended in patients receiving concomitant intravenous therapy with vasodilators and/or inotropic agents. Prescribing a higher loading dose of 12 mcg/kg will be accompanied by greater hemodynamic effects, but it is possible that the incidence of transient adverse effects will also increase.
The patient’s response to therapy is evaluated at loading dose or within 3060 minutes of dose adjustment or depending on the clinical picture.
In case of marked changes of hemodynamic parameters (arterial hypotension, tachycardia) the infusion rate should be reduced to 0.05 mcg/kg/min or the infusion should be stopped. If the initial dose is well tolerated and a more pronounced hemodynamic effect is needed, the infusion rate may be increased to 0.2 µg/kg/min.
The recommended duration of infusion is 24 h. No signs of tolerance or “withdrawal” syndrome were found after discontinuation of Simdax infusion. Hemodynamic effects have been observed for at least 24 h and may not persist for 9 days after completion of the 24-hour infusion.
Patients in the elderly
Dose adjustment in elderly patients is not required.
Renal dysfunction
Simdax should be used with caution in patients with mild to moderate renal impairment. It should not be administered in patients with severe renal impairment (creatinine clearance less than 30 mL/min) (see sections Pharmacokinetics, Contraindications, Precautions).
Hepatic impairment
Simdax should be used with caution in patients with mild (Child-Pugh score 5-6) or moderate (Child-Pugh score 7-9) hepatic impairment, but no dose adjustment is necessary. It should not be administered to patients with severe hepatic impairment (> Child-Pugh score 9) (see sections Pharmacokinetics, Contraindications, and Precautions).
Children
Simdax should not be used in children and adolescents under 18 years of age (see Pharmacokinetics, Contraindications, Specific Indications)
Experience with repeated infusions of Simdax and its use in combination with other inotropic agents (except digoxin) is limited.
Compatibility
Simdax may be administered concomitantly
Interaction
Interaction
Levosimendan should be used with caution in combination with intravenous vasodilators due to a possible increased risk of arterial hypotension.
In vitro studies on human liver microsomes have shown that levosimendan should not interact with drugs metabolized by cytochrome P450 (CYP) isoenzymes due to low affinity for various CYP isoenzymes.
Population pharmacokinetic analysis showed no evidence of interaction between digoxin and levosimendan. Levosimendan can be used in patients receiving beta-adrenoblockers, which does not affect the effectiveness of treatment.
The simultaneous use of isosorbide mononitrate and levosimendan in healthy volunteers caused a significant increase in orthostatic hypotension.
Incompatibilities
The drug must not be mixed with other drugs or solutions except as listed under Dosage and administration/compatibilities.
Special Instructions
Special Instructions
The drug may only be used in a hospital setting that has the necessary equipment to monitor vital functions and has medical personnel experienced in inotropic agents.
The drug can only be used if it is within the expiration date and has been stored according to the instructions for use.
The initial hemodynamic effect of levosimendan is to decrease systolic and diastolic BP; therefore, it should be used with caution in patients with baseline low systolic and diastolic BP or with a tendency to arterial hypotension. For these patients, use of low doses of the drug is recommended.
The dose, speed of administration, and duration of therapy should be adjusted according to the patient’s condition and response to therapy.
Effective hypovolemia should be corrected prior to infusion of Simdax. If significant changes or fluctuations in BP and HR are observed, the infusion rate should be reduced or the infusion should be stopped.
Hemodynamic effects are usually observed within 7-10 days. This is partly due to the circulation of the active metabolite, whose plasma concentration reaches a maximum about 48 hours after the end of the infusion. Non-invasive monitoring is recommended to continue for at least 4-5 days after discontinuation of the infusion until BP begins to rise again after a period of maximum decrease.
The monitoring period can be longer than 5 days if the BP continues to decline, but can be less than 5 days if the patient has stabilized.
Infusion of Simdax should be used with caution in patients with mild to moderate renal or hepatic impairment. The available data on excretion of active metabolites in impaired renal function are insufficient. Renal and hepatic dysfunction may lead to increased concentrations of active metabolites and more pronounced and persistent hemodynamic effects. The functional status of the liver and renal function should be monitored for at least 5 days after the end of infusion.
At the time of treatment, it is advisable to continuously monitor ECG, BP and HR and measure diuresis for at least 3 days after discontinuation of the infusion or until the patient’s condition has stabilized.
Infusion of Simdax may cause decreased serum potassium concentrations, so hypokalemia should be corrected before infusion and serum potassium levels monitored during treatment.
Infusions of Simdax, as well as other agents intended to treat chronic heart failure, may be accompanied by a decrease in hemoglobin and hematocrit concentrations, so caution should be exercised in patients with coronary heart disease and concomitant anemia.
Infusion of Simdax should be used with caution in patients with tachycardia or tachysystolic atrial fibrillation or potentially life-threatening arrhythmias.
The experience with repeated use of Simdax, use of Simdax in heart failure after surgery, and in severe heart failure in patients awaiting heart transplantation is limited. There is also insufficient experience with inotropic agents (excluding digoxin) concomitantly with Simdax.
The benefits and risks of prescribing such medications must be evaluated on a case-by-case basis.
The use of Simdax in cardiogenic shock has not been studied.
Infusion of Simdax should be performed under continuous ECG monitoring in patients with persistent myocardial ischemia and prolonged QT interval regardless of etiology or concomitant use of other drugs that cause QT interval prolongation.
There is no information about the use of Simdax in the following diseases: restrictive cardiomyopathy, hypertrophic cardiomyopathy, severe mitral valve failure, myocardial rupture, cardiac tamponade, right ventricular myocardial infarction. There is very limited experience with Simdax in children and adolescents under 18 years of age, so it should not be used in patients under 18 years of age.
Prepared solution
While prepared Simdax solution is stable for 24 h at 25°C, it should be administered immediately after preparation. If the solution is not immediately used, medical personnel are responsible for the duration and conditions of storage. In any case, the duration of storage of the prepared solution should not exceed 24 hours.
Contraindications
Contraindications
Side effects
Side effects
The most frequent adverse effects (in 53% of patients) reported in clinical trials (REVIVE) were headache, markedly reduced BP, and ventricular tachycardia.
In the SURVIVE clinical trial, 18% of patients experienced: ventricular tachycardia, atrial fibrillation, marked BP decrease, ventricular extrasystole, tachycardia, headache.
The following are the adverse effects reported in clinical trials (REVIVE I, REVIVE I, SURVIVE, LIDO, RUSSLAN) in >1% of patients. Adverse events were distributed by frequency as follows: very common (>1/10), common (>1/100, Frequent
Metabolic side: hypokalemia. Mental status: insomnia.
Gastrointestinal tract: nausea, constipation, diarrhea, vomiting.
Laboratory findings: decreased hemoglobin concentration.
Very common
Central nervous system: dizziness, headache. Cardiovascular system: atrial fibrillation, atrial flutter, tachycardia, ventricular extrasystole, ventricular tachycardia, arterial hypotension up to severe, heart failure, myocardial ischemia, extrasystole.
In the marketing use of the drug, ventricular fibrillation has been reported.
Overdose
Overdose
Symptoms: marked BP decrease and tachycardia, increased blood content of the active metabolite, possible prolongation of the QT interval.
Treatment: with marked BP decrease vasopressor agents may be used: dopamine in patients with chronic heart failure and epinephrine (adrenaline) after cardiac surgery.
A sharp decrease in ventricular filling pressure may limit the effect of levosimendan; parenteral administration of fluids is indicated to restore pressure.
Permanent ECG monitoring, repeat serum electrolyte determination and invasive hemodynamic monitoring should be performed.
Pregnancy use
Pregnancy use
There is no experience with the use of levosimendan in pregnant women.
In this regard, levosimendan in pregnant women may be used only if the benefit to the mother exceeds the possible risk to the fetus and/or child.
There is no information about excretion of levosimendan with the breast milk.
Women should not breastfeed when using and for 14 days after levosimendan infusion.
Additional information
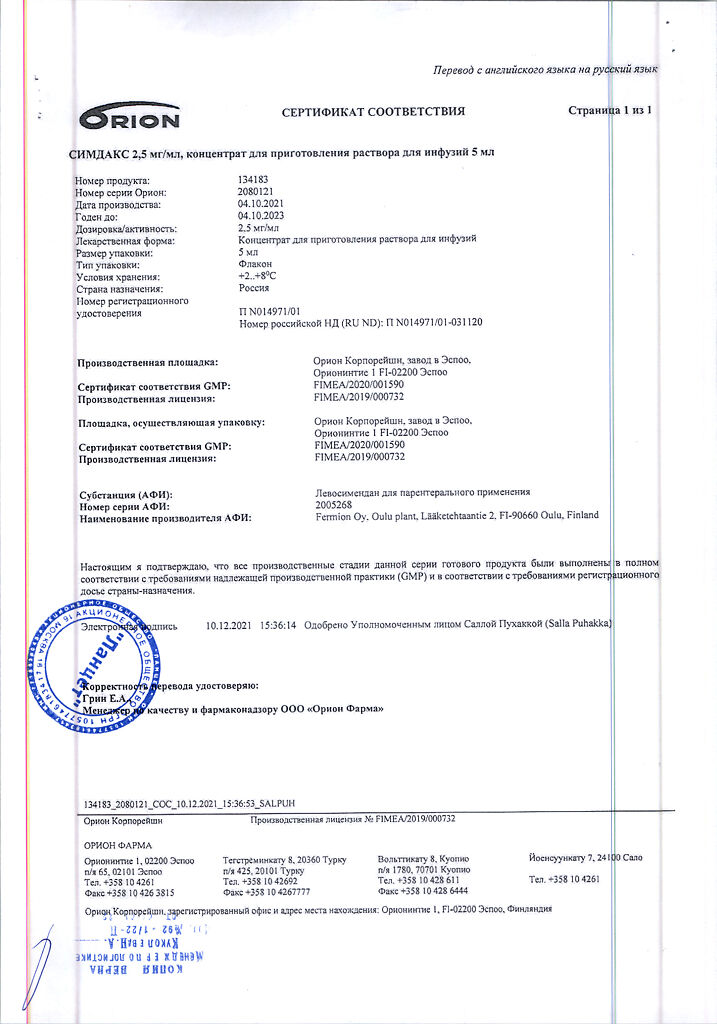
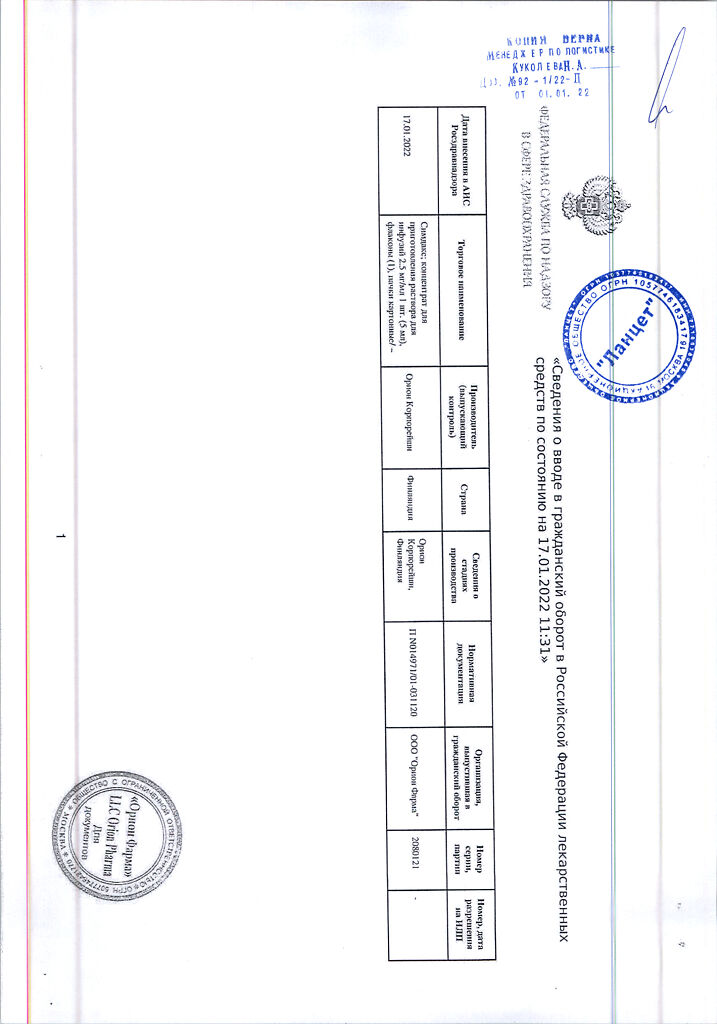
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At 2-8 °C (do not freeze) |
| Manufacturer | Orion Corporation, Finland |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Orion Corporation |
Related products
Buy Simdax, 2.5mg/ml 5 ml with delivery to USA, UK, Europe and over 120 other countries.