No products in the cart.
Simbrinza, eye drops 2 mg/ml+10 mg/ml 5 ml
€53.70 €46.54
Description
Pharmacotherapeutic group: Antiglaucoma drugs and myotics. Carboangidrase inhibitors. Brinzolamide in combination with other drugs.
The ATC code: S01EC54
Pharmacological properties
Pharmacodynamics
The mechanism of action
The drug Simbrinza® contains two active ingredients: brinzolamide and brimonidine tartrate. These two components decrease intraocular pressure (IOP) in patients with open-angle glaucoma (OAG) and intraocular hypertension (IOP) by inhibiting the production of aqueous humor in the ciliary body. Although both brinzolamide and brimonidine reduce IOP by inhibiting aqueous humor formation, their mechanisms of action are different.
Brinzolamide acts by inhibiting the type 2 enzyme carboanhydrase (CA-II) in the ciliary epithelium, which reduces the formation of bicarbonate ions with a subsequent
reduction in the passage of sodium and fluid through the ciliary epithelium, resulting in a reduction in aqueous humor formation. Brimonidine, an alpha 2-adrenergic receptor agonist, inhibits the enzyme adenylate cyclase and inhibits the cAMP-dependent formation of aqueous humor. In addition, the use of brimonidine leads to an increase in uveoscleral outflow.
Pharmacokinetics
Absorption
After topical application, brinzolamide is absorbed through the cornea. The substance also penetrates into the systemic bloodstream, where it binds firmly to carboangidase in erythrocytes. Plasma concentrations of brinzolamide are very low. Blood elimination half-life in humans is long (>100 days) due to binding to erythrocyte carboangidase.
Brinzolamide is rapidly absorbed into ocular tissue after topical application. In rabbit studies the maximum concentration in ocular tissues was reached in less than an hour in most cases. Maximum human plasma concentrations are <1 ng/ml and are reached within <1 hour. The plasma elimination half-life is about 2-3 hours. No accumulation is observed with continued use.
The clinical study examined the pharmacokinetics of Simbrinza® when administered topically 2 and 3 times daily compared to brinzolamide and brimonidine monotherapy administered in the same dosing regimens.
The pharmacokinetics of brinzolamide and N-dezethylbrinzolamide in whole blood when reaching equilibrium concentrations were similar when using the combination drug Simbrinza and brinzolamide monotherapy. Similarly, the pharmacokinetics of brimonidine upon reaching equilibrium in plasma with the fixed combination was similar to that observed with brimonidine alone, with the exception of the twice-daily Simbrinza® use group, in which the average AUC0-12 hours was approximately 25% lower than with brimonidine twice-daily monotherapy.
Distribution
In rabbit studies, maximum concentrations of brinzolamide in ocular tissues after topical administration are achieved in the anterior segment of the eye: cornea, conjunctiva, aqueous humor, iris and ciliary body. Prolonged presence in ocular tissues is due to binding of the drug to carboangidase. Brinzolamide binds moderately (about 60%) to human plasma proteins.
Brimonidine exhibits affinity to pigmented tissues of the eye, particularly the iris and ciliary body, which is due to the known ability of the molecule to bind to melanin. However, clinical and preclinical safety data show that the drug is well tolerated and safe with continued use.
Metabolism
Brinzolamide is metabolized by cytochrome P450 isoenzymes in the liver, specifically CYP3A4, CYP2A6, CYP2B6, CYP2C8 and CYP2C9. The major metabolite is Ndezethylbrinzolamide, followed by N-desmethoxypropyl and O-desmethyl metabolites, as well as an N-propionic acid analog formed by oxidation of the N-propyl side chain of O-desmethylbrinzolamide. Brinzolamide and N-dezethylbrinzolamide do not inhibit cytochrome P450 isoenzymes at concentrations at least 100 times higher than the maximum systemic concentrations.
Brimonidine is extensively metabolized by hepatic aldehydoxidase to form 2-oxobrimonidine, 3-oxobrimonidine and 2,3-dioxobrimonidine, which are the major metabolites. Oxidative cleavage of the imidazoline ring to 5-bromo-6-guanidinoquinoxaline is also observed.
Brinzolamide is mainly excreted unchanged in the urine. In humans, the urine detects 60% brinzolamide and 6% N-desethylbrinzolamide of the administered dose. In rats, excretion of the drug with bile (about 30% of the administered dose) mainly in the form of metabolites was also shown.
Brimonidine is excreted mainly in the urine as metabolites. In preclinical in vivo experiments, urinary metabolites accounted for 60% to 75% of the administered dose
of the drug in both oral and intravenous routes of administration.
Linearity/nonlinearity
The pharmacokinetics of brinzolamide are inherently nonlinear due to saturable binding to carboanhydrase in whole blood and various tissues.
The exposure at equilibrium does not increase in proportion to the dose. In contrast, brimonidine exhibits linear pharmacokinetics across the clinical therapeutic dose range.
The relationship between pharmacokinetics and pharmacodynamics
The drug Simbrinza is intended to act locally within the tissues of the eye. Evaluation of intraocular exposure in humans of effective doses is not possible.
The effects of the drug’s pharmacokinetics and pharmacodynamics in humans on IOP reduction have not been established.
Other special patient populations
There have been no studies to determine the effect of age, race, renal or hepatic impairment with Simbrinza®.
A study of brinzolamide use in Japanese compared to patients of other ethnicities showed similar systemic pharmacokinetics in both groups.
A study of brinzolamide in patients with impaired renal function showed that systemic exposure to brinzolamide and N-dezethylbrinzolamide in patients with moderate
renal impairment was 1.6 to 2.8 times that of patients with normal renal function. This increase in equilibrium concentrations of the drug and its metabolites did not cause inhibition of erythrocyte carboanhydrase to levels associated with systemic side effects. However, the use of the combination drug is contraindicated in patients with severe renal impairment (creatinine clearance < 30 ml/min). Cmax, AUC and half-life of brimonidine are similar in elderly patients (>65 years) and adult patients of younger age. The effect of renal and hepatic dysfunction on the systemic pharmacokinetics of brimonidine has not been evaluated. Given the low systemic exposure of brimonidine after topical ophthalmic use, changes in plasma exposure are not expected to be clinically significant.
Children
The systemic pharmacokinetics of brinzolamide and brimonidine, in monotherapy or in combination, have not been studied in pediatric patients.
Indications
Indications
Reducing elevated intraocular pressure (IOP) in patients with open-angle
glaucoma or ocular hypertension, for which monotherapy does not provide
sufficient reduction in IOP
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Antiglaucoma drugs and miotics. Carbonic anhydrase inhibitors. Brinzolamide in combination with other drugs.
ATX code: S01EC54
Pharmacological properties
Pharmacodynamics
Mechanism of action
Simbrinza® contains two active ingredients: brinzolamide and brimonidine tartrate. These two components reduce intraocular pressure (IOP) in patients with open-angle glaucoma (OAG) and intraocular hypertension (IOH) by inhibiting the formation of aqueous humor in the ciliary body. Although brinzolamide and brimonidine both reduce IOP by inhibiting aqueous humor formation, their mechanisms of action are different.
Brinzolamide acts by inhibiting the enzyme carbonic anhydrase type 2 (CA-II) in the ciliated epithelium, which reduces the formation of bicarbonate ions with subsequent
a decrease in the passage of sodium and fluid through the ciliated epithelium, which leads to a decrease in the formation of aqueous humor. Brimonidine, an alpha-2 adrenergic receptor agonist, inhibits the enzyme adenylate cyclase and suppresses cAMP-dependent aqueous humor formation. In addition, the use of brimonidine leads to an increase in uveoscleral outflow.
Pharmacokinetics
Absorption
After topical application, brinzolamide is absorbed through the cornea. The substance also penetrates the systemic circulation, where it binds tightly to carbonic anhydrase in erythrocytes. Plasma concentrations of brinzolamide are very low. The half-life in humans is long (>100 days), due to binding to carbonic anhydrase in red blood cells.
Brimonidine is rapidly absorbed into the eye tissue after topical application. In studies in rabbits, maximum ocular concentrations were achieved in less than an hour in most cases. Maximum concentrations in human plasma are <1 ng/ml and are achieved within <1 hour. The half-life from blood plasma is about 2-3 hours. With continuous use, no accumulation is observed.
A clinical study examined the pharmacokinetics of Simbrinza® when administered topically 2 and 3 times a day in comparison with monotherapy with brinzolamide and brimonidine used in the same dosage regimens.
The pharmacokinetics of brinzolamide and N-desethylbrinzolamide in whole blood at steady state concentrations were similar between Simbrinza combination therapy and brinzolamide monotherapy. Similarly, the pharmacokinetics of brimonidine at steady state in plasma with the fixed combination were similar to those observed with brimonidine alone, with the exception of the twice-daily Simbrinza group, in which the mean AUC0-12 hours was approximately 25% less than with brimonidine twice-daily monotherapy.
Distribution
In studies on rabbits, the maximum concentrations of brinzolamide in ocular tissues after topical application were achieved in the anterior segment of the eye: in the cornea, conjunctiva, aqueous humor, iris and ciliary body. Long-term presence in the tissues of the eye is due to the binding of the drug to carbonic anhydrase. Brinzolamide is moderately bound (about 60%) to human plasma proteins.
Brimonidine exhibits affinity for pigmented tissues of the eye, in particular the iris and ciliary body, due to the known ability of the molecule to bind to melanin. However, clinical and preclinical safety data indicate that the drug is well tolerated and safe with chronic use.
Metabolism
Brinzolamide is metabolized by cytochrome P450 isoenzymes in the liver, in particular CYP3A4, CYP2A6, CYP2B6, CYP2C8 and CYP2C9. The major metabolite is N-desethylbrinzolamide, followed by N-desmethoxypropyl and O-desmethyl metabolites, as well as an N-propionic acid analogue formed by oxidation of the N-propyl side chain of O-desmethylbrinzolamide. Brinzolamide and Ndesethylbrinzolamide do not inhibit cytochrome P450 isoenzymes at concentrations at least 100 times the maximum systemic concentration.
Brimonidine is extensively metabolized by hepatic aldehyde oxidase to form 2-oxobrimonidine, 3-oxobrimonidine and 2,3-dioxobrimonidine, which are the main metabolites. Oxidative cleavage of the imidazoline ring to 5-bromo-6-guanidinoquinoxaline is also observed.
Removal
Brinzolamide is mainly excreted unchanged in the urine. In humans, 60% of brinzolamide and 6% of N-desethylbrinzolamide from the administered dose are determined in urine. Excretion of the drug into bile (about 30% of the administered dose) was also shown in rats, mainly in the form of metabolites.
Brimonidine is excreted primarily in the urine in the form of metabolites. In preclinical in vivo experiments, metabolites in urine ranged from 60% to 75% of the administered dose
the drug via both oral and intravenous routes of administration.
Linearity/nonlinearity
The pharmacokinetics of brinzolamide are inherently nonlinear due to saturable binding to carbonic anhydrase in whole blood and various tissues.
Exposure at steady state does not increase proportionally to dose. In contrast, brimonidine exhibits linear pharmacokinetics over the clinical therapeutic dose range.
Relationship between pharmacokinetics and pharmacodynamics
Simbrinza is intended for local action within the tissues of the eye. Estimation of intraocular exposure in humans at effective doses is not possible.
The effect of the pharmacokinetics and pharmacodynamics of the drug in humans on reducing IOP has not been established.
Other special patient populations
Studies have not been conducted to determine the effects of age, race, or renal or hepatic impairment on Simbrinza.
A study of brinzolamide in Japanese patients compared with patients of other nationalities showed similar systemic pharmacokinetics in both groups.
A study of brinzolamide in patients with impaired renal function showed that systemic exposure of brinzolamide and N-desethylbrinzolamide in patients with moderate
impaired renal function is 1.6-2.8 times higher than that in patients with normal renal function. This increase in steady-state concentrations of the drug and its metabolites did not inhibit erythrocyte carbonic anhydrase to levels associated with systemic side effects. However, the use of the combination drug is contraindicated in patients with severe renal impairment (creatinine clearance 65 years) and younger adult patients. The effect of renal and hepatic impairment on the systemic pharmacokinetics of brimonidine has not been assessed. Given the low systemic exposure of brimonidine following topical ophthalmic administration, changes in plasma exposure are not expected to be clinically significant.
Children
The systemic pharmacokinetics of brinzolamide and brimonidine, alone or in combination, have not been studied in pediatric patients.
Special instructions
Special instructions
The drug should not be administered by injection. Patients should be instructed not to take Simbrinza® by mouth.
Effect on the organ of vision
Simbrinza has not been studied in patients with angle-closure glaucoma and its use in such patients is not recommended. The possible effect of brinzolamide on corneal endothelial function has not been studied in patients with corneal disorders (especially in patients with low endothelial cell counts). The drug has also not been studied in patients who wear contact lenses, and close monitoring of such patients is recommended when using brinzolamide, since carbonic anhydrase inhibitors may affect corneal hydration, and wearing contact lenses may increase the risk of corneal damage. Close monitoring of
is recommended
patients with corneal disorders, including patients with diabetes mellitus or corneal dystrophy. Simbrinza® can be used while wearing
contact lenses with careful observation (see below under Benzalkonium Chloride).
Brimonidine tartrate may cause allergic reactions in the eyes. If allergic reactions occur, treatment with the drug should be discontinued. There are reports of delayed-type hypersensitivity reactions in the eye when using brimonidine tartrate, in some cases occurring with an increase in IOP.
Potential effects following discontinuation of treatment with Simbrinza have not been studied, and in particular the duration of the drug’s effect on IOP levels has not been assessed.
After discontinuation of brinzolamide, the IOP-lowering effect is expected to persist for 5-7 days. IOP reduction with brimonidine may continue
longer.
Systemic effects
Simbrinza® contains brinzolamide, a sulfonamide carbonic anhydrase inhibitor, which, despite topical application, penetrates the systemic circulation. With local use of sulfonamides, the same adverse reactions may occur as with systemic use. If signs of a serious hypersensitivity reaction occur, discontinue use of the drug immediately.
Heart disorders
Some patients experienced a slight decrease in blood pressure after taking Simbrinza. Caution is recommended during the simultaneous use of antihypertensive drugs and (or) cardiac glycosides, as well as in patients with severe or unstable and uncontrolled cardiovascular diseases (see section “Interaction with other drugs”).
Simbrinza should be used with caution in patients with depression, cerebrovascular insufficiency or coronary insufficiency, Raynaud’s syndrome, orthostatic hypotension or thromboangiitis obliterans.
Acid-base balance disorders
Disturbances in acid-base balance have been reported with the use of oral carbonic anhydrase inhibitors. Simbrinza® contains brinzolamide, a carbonic anhydrase inhibitor, which, despite topical application, penetrates into the systemic circulation. When using Simbrinza topically, the same adverse reactions may occur as when using oral carbonic anhydrase inhibitors (i.e., acid-base imbalance) (see section “Interaction with other drugs”).
The drug should be used with caution in patients at risk of renal impairment due to the possible risk of developing metabolic acidosis. Simbrinza®
Contraindicated in patients with severe renal impairment (see section “Contraindications”).
Liver dysfunction
Simbrinza has not been studied in patients with hepatic impairment; care should be taken when treating such patients (see section “Method
application and dose”).
Ability to concentrate
Oral carbonic anhydrase inhibitors may impair the ability to perform tasks requiring alertness and/or physical coordination in elderly patients.
The drug Simbrinza® penetrates the systemic bloodstream, so these phenomena can be observed with local use of the drug (see section “Effects on the ability to drive vehicles and machines”).
Benzalkonium chloride
Simbrinza® contains benzalkonium chloride, which may cause eye irritation and discoloration of soft contact lenses. Avoid contact of the drug with soft
contact lenses. Patients should be instructed to remove contact lenses before instilling Simbrinza® and to wait at least 15 minutes before using them
re-installation.
Benzalkonium chloride has been reported to cause punctate keratopathy and/or toxic ulcerative keratopathy. Frequent or prolonged use requires careful monitoring.
Use in children
The safety and effectiveness of Simbrinza® in children and adolescents from 2 to 18 years of age have not been established. In cases where brimonidine in the form of eye drops was used
As part of the treatment of congenital glaucoma in neonates and infants, symptoms of brimonidine overdose (such as loss of consciousness, decreased blood pressure, hypotension, bradycardia, hypothermia, cyanosis, and apnea) have been reported. Therefore, Simbrinza® is contraindicated in children under 2 years of age (see section “Contraindications”).
Treatment of children aged 2 years and older (especially in persons aged 2-7 years and/or weighing less than 20 kg) is not recommended due to the possible occurrence of side effects
effects on the central nervous system (see section “Overdose”).
Impact on the ability to drive vehicles and machinery
Simbrinza® has a moderate effect on the ability to drive vehicles and operate machinery.
Simbrinza may cause dizziness, fatigue and/or drowsiness, which may impair your ability to drive.
means or work with machinery.
Temporary blurred vision or other visual disturbances may occur, which may affect the ability to drive or operate machinery.
Active ingredient
Active ingredient
Brimonidine, Brinzolamide
Composition
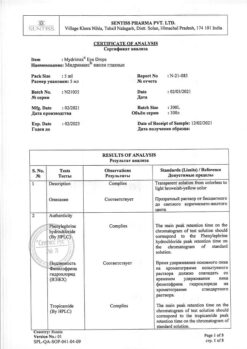
Composition
1 ml of the drug contains:
active ingredients:
Brimonidine tartrate – 2 mg,
brinzolamide – 10 mg;
excipients: carbomer 974P, sodium chloride, mannitol, propylene glycol, tyloxapol, boric acid, benzalkonium chloride, sodium hydroxide and/or hydrochloric acid, purified water
Pregnancy
Pregnancy
Pregnancy
There are no or limited data on the use of Simbrinza in pregnant women. Brinzolamide was not teratogenic in rats and rabbits after systemic administration.
Studies of oral administration of brinzolamide in animals did not reveal any direct negative effects on reproductive function. In animal studies, brimonidine crossed the placenta and entered the fetal circulation in limited quantities. It is not recommended to use Simbrinza® during pregnancy and in women of reproductive age who do not use reliable contraceptive measures.
Breast-feeding
It has not been established whether Simbrinza® is excreted into breast milk in women. Available pharmacodynamic/toxicological data from animal studies indicate that minimal amounts of brinzolamide are excreted into breast milk following oral administration. Brimonidine is excreted into breast milk after oral administration.
Simbrinza® should not be used during breastfeeding.
Fertility
Preclinical data have not shown an effect of brinzolamide or brimonidine on fertility.
There are no data on the effects of Simbrinza® on fertility when administered topically to ophthalmology in humans.
Contraindications
Contraindications
Hypersensitivity to active or excipients, or to sulfonamides:
– During therapy with monoamine oxidase inhibitors (MAO);
– When using antidepressants that affect noradrenergic transmission (for example, tricyclic antidepressants and mianserin);
– Severe renal impairment;
– Hyperchloremic acidosis;
– Newborns and children under 2 years of age;
With caution:
– History of angle-closure glaucoma;
– Liver dysfunction;
– Corneal disorders;
– Severe, unstable and/or uncontrolled cardiovascular disease;
– Depression;
– Cerebral or coronary insufficiency, Raynaud’s phenomenon, orthostatic hypotension or thromboangiitis obliterans;
– Pregnancy and breastfeeding (see section “Use during pregnancy and breastfeeding”) ;
– Children aged 2 to 18 years due to insufficient data on effectiveness and safety;
– When used simultaneously with substances that depress the central nervous system;
– When used together with drugs that may affect the metabolism and uptake of circulating amines;
– When used together with antihypertensive drugs and (or) cardiac glycosides;
– With simultaneous treatment (or dose change) with systemic drugs (regardless of the dosage form), which may interact with alpha-adrenergic receptor agonists or interfere with the manifestation of their activity;
– Wearing contact lenses;
– Patients at risk of renal impairment.
Side Effects
Side Effects
In clinical studies using Simbrinza twice daily, the most common adverse reactions were ocular hyperemia and ocular allergic reactions, occurring in approximately 6-7% of patients, and dysgeusia (bitter or unusual taste in the mouth after instillation), occurring in approximately 3% of patients. The safety profile of Simbrinza® was similar to the safety profile of its individual components (brinzolamide 10 mg/ml and brimonidine 2 mg/ml).
The following adverse reactions were reported during clinical studies with Simbrinza® twice daily, as well as during clinical studies and post-marketing surveillance with the individual components, brinzolamide and brimonidine.
Adverse reactions are classified according to the following classification: very common (≥1/10), common (≥1/100, <1/10), uncommon (≥1/1000, <1/100), rare
(≥1/10000, <1/1000), very rare (<1/10000), unknown (cannot be estimated based on available data). Within each frequency group, adverse reactions are presented in descending order of severity.
Infectious and parasitic diseases: uncommon – nasopharyngitis2, pharyngitis2, sinusitis2; frequency unknown – rhinitis2.
Blood and lymphatic system disorders: uncommon – decreased red blood cell count2, increased chloride levels2.
Immune system disorders: uncommon – hypersensitivity reactions3.
Mental disorders: uncommon – apathy2, depression2,3, depressed mood2, insomnia1, decreased libido2, nightmares2, nervousness2.
Nervous system disorders: often – drowsiness1, dizziness3, dysgeusia1; uncommon – headache1, motor dysfunction2, amnesia2, memory impairment2, paresthesia2;
very rarely – fainting3; frequency unknown – tremor2, hypoesthesia2, ageusia2.
Violations of the organ of vision: often – allergic reaction of the eyes1, keratitis1, pain in the eyes1, discomfort in the eyes1, blurred vision1, blurred vision3, eye hyperemia1, pallor of the conjunctiva3; infrequently – corneal erosion1, corneal edema2, blepharitis1, deposits in the cornea (precipitates)1, disorders of the conjunctiva (papillae)1, photophobia1, photopsia2, ocular edema2, eyelid edema1, conjunctival edema1, dry eye1, discharge from the eye1, decreased visual acuity2, increased lacrimation1, pterygium2, eyelid erythema1, meibomyitis2, diplopia2, eye pain in bright light2, eye hypoesthesia2, scleral pigmentation2, subconjunctival cyst2, discomfort in the eyes1, asthenopia1; very rarely – uveitis3, miosis3; frequency unknown – visual impairment2, madarosis2.
Hearing and labyrinthine disorders: uncommon – dizziness1, ringing in the ears2.
Cardiac disorders: uncommon – cardiorespiratory distress2, angina2, arrhythmia3, palpitations2,3, irregular heart rhythm2, bradycardia2,3, tachycardia3.
Vascular disorders: uncommon – decreased blood pressure1; very rarely – increased blood pressure3.
Disorders of the respiratory system, chest and mediastinal organs: infrequently – shortness of breath2, bronchial hyperreactivity2, pharyngolaryngeal pain2, dry throat1, cough2, nosebleeds2, upper respiratory tract congestion2, nasal congestion1, rhinorrhea2, pharyngeal irritation2, dry nasal cavity1, postnasal drip1, sneezing2;
frequency unknown – asthma2.
Gastrointestinal disorders: often – dry mouth1; uncommon – dyspepsia1, esophagitis2, abdominal discomfort1, diarrhea2, vomiting2, nausea2, frequent bowel movements2, flatulence2, oral hypoesthesia2, oral paresthesia.1
Disorders of the liver and biliary tract: frequency unknown – deviation of liver function tests from the norm2.
Disorders of the skin and subcutaneous tissues: uncommon – contact dermatitis1, urticaria2, rash2, maculopapular rash2, generalized itching2, alopecia2, skin thickening2; frequency unknown – facial swelling3, dermatitis2,3, erythema2,3.
Musculoskeletal and connective tissue disorders: uncommon – back pain2, muscle spasms2, myalgia2; frequency unknown – arthralgia2, pain in the extremities2.
Renal and urinary tract disorders: uncommon – pain in the kidney area2
Disorders of the genital organs and breast: uncommon – erectile dysfunction2;
General disorders and disorders at the injection site: uncommon – pain2, discomfort in the chest2, deterioration of health2, anxiety2, irritability2, drug residues1; frequency unknown – chest pain2, peripheral edema2,3.
Note
1 adverse reactions observed with Simbrinza®.
2 additional adverse reactions observed with brinzolamide monotherapy.
3 additional adverse reactions observed with brimonidine monotherapy.
Description of selected adverse reactions
Dysgeusia was the most common systemic adverse reaction associated with Simbrinza® (3.4%). This is likely due to eye drops entering the nasopharynx through the nasolacrimal duct and is mainly due to the presence of brinzolamide in Simbrinza®. Occlusion of the nasolacrimal duct or slight closure of the eyelids after instillation may reduce the incidence of this effect (see section “Dosage and Administration”).
Simbrinza® contains brinzolamide, a sulfonamide carbonic anhydrase inhibitor that penetrates into the systemic circulation. Effects on the gastrointestinal tract, nervous system, blood system, kidneys and metabolism are mainly associated with the systemic action of carbonic anhydrase inhibitors. When carbonic anhydrase inhibitors are used topically, the same adverse reactions may develop as with oral use.
Adverse reactions associated with the brimonidine content of Simbrinza® include the development of allergic reactions in the eyes, increased
fatigue and/or drowsiness, as well as dry mouth. Brimonidine use is associated with minimal reductions in blood pressure. Some patients receiving Simbrinza experienced a reduction in blood pressure similar to that observed with brimonidine alone.
Interaction
Interaction
Specific drug interaction studies have not been conducted with Simbrinza®.
Simbrinza® is contraindicated in patients receiving monoamine oxidase inhibitors and antidepressants that affect noradrenergic
transmission (for example, tricyclic antidepressants and mianserin), (see section “Contraindications”). Tricyclic antidepressants may reduce the ability of Simbrinza to reduce IOP.
Caution is recommended during concomitant use with substances that depress the central nervous system (alcohol, barbiturates, opiates, sedatives or
anesthetics) due to the possibility of developing an additive or potentiating effect.
There are no data on the concentration of circulating catecholamines after use of Simbrinza®. However, caution is advised when treating patients receiving drugs that may affect the metabolism and uptake of circulating amines (eg, chlorpromazine, methylphenidate, reserpine, serotonin-norepinephrine reuptake inhibitors).
Alpha-adrenergic agonist class drugs (eg, brimonidine tartrate) may decrease heart rate and lower blood pressure. Some patients experienced a slight decrease in blood pressure after taking Simbrinza. Caution is recommended when using Simbrinza® concomitantly with antihypertensive drugs and/or cardiac glycosides.
Caution is recommended when initiating concomitant treatment (or changing the dose) with drugs with systemic effects (regardless of drug
forms) that can interact with alpha-adrenergic receptor agonists or interfere with the manifestation of their activity, that is, agonists or antagonists
adrenergic receptors (for example, isoprenaline, prazosin).
Brinzolamide is a carbonic anhydrase inhibitor that, despite topical application, penetrates into the systemic circulation. Acid-base disturbances have been reported
balance when using oral carbonic anhydrase inhibitors. Possible interactions should be considered in patients receiving Simbrinza®.
There is a potential for increased known systemic effects of carbonic anhydrase inhibitors in patients receiving an oral carbonic anhydrase inhibitor and
brinzolamide for topical use. Concomitant use of Simbrinza and oral carbonic anhydrase inhibitors is not recommended.
Cytochrome P-450 isoenzymes responsible for the metabolism of brinzolamide include CYP3A4 (major), CYP2A6, CYP2B6, CYP2C8 and CYP2C9. It is expected that inhibitors
CYP3A4 drugs such as ketoconazole, itraconazole, clotrimazole, ritonavir and troleandomycin will inhibit the CYP3A4 metabolism of brinzolamide. Recommended
use caution when coadministering CYP3A4 inhibitors. However, the accumulation of brinzolamide is unlikely, since the main route of elimination is
kidneys Brinzolamide is not an inhibitor of cytochrome P-450 isoenzymes.
Overdose
Overdose
In case of overdose of Simbrinza®, symptomatic and supportive therapy should be carried out. It is necessary to monitor the patient’s airway.
Due to the presence of brinzolamide in Simbrinza®, electrolyte imbalance, acidosis, and nervous system disorders may occur.
The content of electrolytes in the blood serum (in particular, potassium) and blood pH should be monitored.
There is very limited information regarding accidental ingestion of brimonidine from Simbrinza in adults. To date, the only reported adverse event is a decrease in blood pressure. It was reported that the episode of hypotension was accompanied by a rebound increase in blood pressure.
Overdose with other oral alpha-2 agonists has been reported to cause symptoms such as hypotension, asthenia, vomiting, lethargy, sedation, bradycardia, arrhythmias, miosis, apnea, hypotension, hypothermia, respiratory depression and convulsions.
Children
There have been reports of serious adverse events in children following accidental ingestion of brimonidine in Simbrinza®. Patients experienced symptoms of central nervous system depression: transient coma or decreased level of consciousness, lethargy, somnolence, hypotension, bradycardia, hypothermia, pallor, respiratory depression and apnea, which required hospitalization in the intensive care unit and intubation as indicated. All effects were reported to be reversible within 6-24 hours
Storage conditions
Storage conditions
At a temperature not exceeding 30°C in the original packaging (bottle in a pack).
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use after the expiration date stated on the package.
Use within 28 days after opening the bottle.
Manufacturer
Manufacturer
S.A. Alkon-Couvreur n.v., Belgium
Additional information
| Shelf life | 2 years. Do not use after the expiration date stated on the package. Use within 28 days after opening the bottle. |
|---|---|
| Conditions of storage | At the temperature not more than 30°C in the original package (bottle in the package). Keep out of reach of children. |
| Manufacturer | s.a. Alcon-Couvreur n.a., Belgium |
| Medication form | eye drops |
| Brand | s.a. Alcon-Couvreur n.a. |
Related products
Buy Simbrinza, eye drops 2 mg/ml+10 mg/ml 5 ml with delivery to USA, UK, Europe and over 120 other countries.