No products in the cart.
Description
Rupatadine belongs to the second generation of antihistamines and is a long-lasting and selective blocker of peripheral H1-histamine receptors. Some of its metabolites (desloratadine and 3-hydroxydesloratadine) retain antihistamine activity and may contribute to the overall effectiveness of the drug.
Rupatadine shows high affinity for H1-histamine receptors. Studies of rupatadine in vitro in high concentration have shown suppression of mast cell degranulation caused by immunological and non-immunological stimuli, suppression of eosinophil and neutrophil chemotaxis, as well as release of cytokines (IL-5 (interleukin-5), IL-6, IL-8, GM-CSF (granulocyte-macrophage colony-stimulating factor)), in particular TNF-ϖ (tumor necrosis factor alpha), from human mast cells and monocytes. In addition, rupatadine caused a dose-dependent suppression of neutrophil adhesion molecule expression.
Due to the selectivity of rupatadine toward peripheral H1-histamine receptors, it has no significant effect on central nervous system (CNS) activity at doses of 10 or 20 mg/day.
Because histamine release is a key link in the pathogenesis of all urticaria, it is expected that when rupatadine is prescribed according to clinical guidelines, it can effectively reduce the severity of symptoms not only of chronic idiopathic urticaria, but also of other variants of urticaria.
Pharmacokinetics
Rupatadine is rapidly absorbed when taken orally, with a time to reach maximum concentration (TCmax.) of approximately 0.75 hours. The mean maximum concentration (Cmax) is 2.6 ng/mL after a single oral dose of 10 mg and 4.6 ng/mL after a single oral dose of 20 mg rupatadine. The pharmacokinetics of rupatadine are linear for doses from 10 to 40 mg. After a dose of 10 mg once daily for 7 days, the average Stah is 3.8 ng/ml. Plasma concentrations decrease according to a biexponential curve, with a mean half-life (T1/2) of 5.9 hours. The binding coefficient of rupatadine to plasma proteins is 98.5 – 99%.
Since rupatadine has never been used intravenously in humans, there are no data on its absolute bioavailability.
Eating increases the overall effect of rupatadine on the body (AUC – area under the concentration-time curve) by approximately 23%. The effects on one of its active metabolites and on the main inactive metabolite are almost identical (reduction by approximately 5% and 3%, respectively). The time required to reach maximum plasma concentration (TCmax) of rupatadine was prolonged by 1 hour. Cmax in plasma was not altered by food intake. These differences had no clinical significance.
A study of excretion in humans (40 mg 14C-rupatadine) found that 34.6% of the drug was excreted by the kidneys and 60.9% through the intestine within 7 days. Rupatadine undergoes significant presystemic metabolism when administered orally. The unchanged active substance is found only in small amounts in urine and feces. This means that rupatadine is almost completely metabolized. In vitro metabolism studies in human liver microsomes indicate that rupatadine is metabolized predominantly by cytochrome P450 (CYP3A4 isoenzyme).
In a study on healthy volunteers comparing results obtained in young and elderly subjects, the AUC and Cmax values for rupatadine were higher in elderly study participants. This is probably due to reduced hepatic metabolism during “first passage through the liver” in the elderly. These differences were noted only for rupatadine and not for its metabolites. The mean T1/2 of rupatadine in older and younger volunteers was 8.7 hours and 5.9 hours, respectively. Because the results for rupatadine and for its metabolites were not clinically significant, it was concluded that no dose adjustment of the drug was necessary when administered to elderly patients at a dose of 10 mg.
Indications
Indications
Symptomatic treatment of allergic rhinitis and urticaria in adults and adolescents (over 12 years of age).
Pharmacological effect
Pharmacological effect
Rupatadine belongs to the second generation of antihistamines and is a long-acting and selective blocker of peripheral H1-histamine receptors. Some of its metabolites (desloratadine and 3-hydroxydesloratadine) retain antihistamine activity and may contribute to the overall effectiveness of the drug.
Rupatadine demonstrates high affinity for histamine H1 receptors. In vitro studies of rupatadine at high concentrations have shown inhibition of mast cell degranulation induced by immunological and non-immunological stimuli, suppression of eosinophil and neutrophil chemotaxis, as well as cytokine release (IL-5 (interleukin-5), IL-6, IL-8, GM-CSF (granulocyte-macrophage colony-stimulating factor)), in particular, TNF-ϖ (tumor necrosis factor alpha), from human mast cells and monocytes. In addition, rupatadine caused a dose-dependent suppression of the expression of neutrophil adhesion molecules.
Due to the selectivity of rupatadine for peripheral H1-histamine receptors, it does not have a significant effect on the activity of the central nervous system (CNS) at doses of 10 or 20 mg/day.
Since histamine release is a key factor in the pathogenesis of all types of urticaria, it is expected that when rupatadine is prescribed in accordance with clinical recommendations, it will be able to effectively reduce the severity of symptoms not only of chronic idiopathic urticaria, but also of other types of urticaria.
Pharmacokinetics
Rupatadine is rapidly absorbed when taken orally, the time to reach maximum concentration (TCmax.) is approximately 0.75 hours. The average maximum concentration (Cmax) is 2.6 ng/ml after a single oral dose of 10 mg and 4.6 ng/ml after a single oral dose of 20 mg rupatadine. The pharmacokinetics of rupatadine is linear for doses from 10 to 40 mg. After taking a dose of 10 mg once daily for 7 days, the average Cmax is 3.8 ng/ml. Plasma concentrations decrease along a biexponential curve, with an average half-life (T1/2) of 5.9 hours. The binding coefficient of rupatadine to plasma proteins is 98.5 – 99%.
Since rupatadine has never been used intravenously in humans, there is no data on its absolute bioavailability.
Eating increases the overall effect of rupatadine on the body (AUC – area under the concentration-time curve) by approximately 23%. The effect on one of its active metabolites and on the main inactive metabolite is almost the same (reduction of approximately 5% and 3%, respectively). The time required to achieve maximum plasma concentration (TCmax) of rupatadine was extended by 1 hour. Cmax in plasma did not change as a result of food intake. These differences were not clinically significant.
An excretion study in humans (40 mg of 14C-rupatadine) found that 34.6% of the drug was excreted by the kidneys and 60.9% through the intestines within 7 days. Rupatadine undergoes significant first-pass metabolism when administered orally. Unchanged active substance is found in urine and feces only in small quantities. This means that rupatadine is almost completely metabolized. In vitro metabolism studies in human liver microsomes indicate that rupatadine is metabolized primarily by cytochrome P450 (CYP3A4 isoenzyme).
In a study in healthy volunteers, comparing results obtained in young and elderly subjects, the AUC and Cmax values for rupatadine were higher in older study participants. This is likely due to decreased hepatic first-pass metabolism in older adults. These differences were noted only for rupatadine and not for its metabolites. The mean T1/2 of rupatadine in elderly and young volunteers was 8.7 hours and 5.9 hours, respectively. Because the results for rupatadine and its metabolites were not clinically significant, it was concluded that no dosage adjustment is required when the drug is administered to elderly patients at a dose of 10 mg.
Active ingredient
Active ingredient
Rupatadine fumarate
Composition
Composition
Active ingredient:
rupatadine fumarate – 12.8 mg, which corresponds to 10 mg rupatadine;
Excipients:
pregelatinized starch – 10.0 mg,
microcrystalline cellulose -15.0 mg,
iron dye red oxide E-172-0.025 mg,
iron dye yellow oxide E-172-0.075 mg,
lactose monohydrate – 61.1 mg,
magnesium stearate-1.0 mg
Pregnancy
Pregnancy
The drug Rupafin® is contraindicated for use during pregnancy and lactation.
Contraindications
Contraindications
Hypersensitivity to the components of the drug.
Children under 12 years of age (efficacy and safety have not been established).
Kidney failure.
Liver failure.
Pregnancy and lactation period.
Rare hereditary galactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome.
With caution: patients with a prolonged QT interval, uncorrected hypokalemia, persistent proarrhythmic conditions such as clinically significant bradycardia, acute myocardial ischemia; elderly patients (65 years and older), concomitant use with statins, concomitant use with grapefruit juice.
Side Effects
Side Effects
From the nervous system: drowsiness, headache, dizziness, fatigue, asthenia, decreased concentration, irritability.
From the respiratory system, chest and mediastinal organs: nosebleeds, dry nasal mucosa, pharyngitis, cough, dry throat, pain in the pharynx and larynx, rhinitis.
From the gastrointestinal tract: dry mouth, nausea, diarrhea, dyspepsia, vomiting, abdominal pain, constipation.
Metabolism and nutrition: increased appetite.
From the skin and subcutaneous tissues: rash.
Musculoskeletal and connective tissue disorders: back pain, arthralgia, myalgia.
General disorders: thirst, malaise, fever, weight gain.
Changes in laboratory parameters: increased creatine phosphokinase, alanine aminotransferase, aspartate aminotransferase; changes in liver function test parameters.
Interaction
Interaction
Interaction with ketoconazole and erythromycin
The combined use of rupatadine at a dose of 20 mg and ketoconazole or erythromycin increases the systemic effect of rupatadine by 10 times and the latter by 2-3 times. These combinations are not accompanied by changes in the QT interval or an increase in the frequency of adverse reactions compared to the separate use of these drugs. However, rupatadine should be used with caution in combination with these drugs and other inhibitors of the CYP3A4 isoenzyme.
Interaction with grapefruit juice
Simultaneous administration of rupatadine and grapefruit juice increases the overall effect of rupatadine by 3.5 times. You should not drink grapefruit juice at the same time as taking the drug.
Interaction with alcohol
When used simultaneously with alcohol, rupatadine at a dose of 10 mg does not cause more pronounced changes in cognitive and psychomotor activity compared to taking alcohol alone. A dose of 20 mg enhances changes caused by alcohol intake.
Interaction with drugs that depress the central nervous system
The possibility of interaction of rupatadine with other antihistamines and central nervous system depressants cannot be excluded.
Interaction with statins
Due to the fact that some of the statins, like rupatadine, are metabolized by the cytochrome P450 isoenzyme CYP3A4, the possibility of an increase in creatinine phosphokinase levels when used together cannot be ruled out. For these reasons, rupatadine should be used with caution concomitantly with statins.
Effect on the ability to drive a car and other mechanisms
When using the drug at a dose of 10 mg, there was no effect on the ability to drive a car or use other mechanisms. At the same time, there are reports of drowsiness noted during treatment with Rupafin®. In this regard, it is recommended to exercise caution when driving a car or engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions until the patient’s individual response to rupatadine is established.
Overdose
Overdose
There are no cases of drug overdose described in the literature. In a clinical safety study, rupatadine was well tolerated at a daily dose of 100 mg for 6 days.
Symptoms: The most common adverse reaction is drowsiness.
Treatment: in case of accidental ingestion of the drug in very high doses, it is recommended to induce vomiting in the patient followed by administration of activated charcoal. If this manipulation turns out to be impossible or ineffective, it is necessary to rinse the stomach with isotonic sodium chloride solution.
Storage conditions
Storage conditions
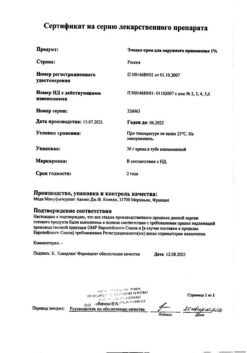
In a dry place, protected from light, at a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
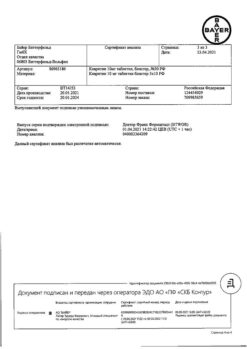
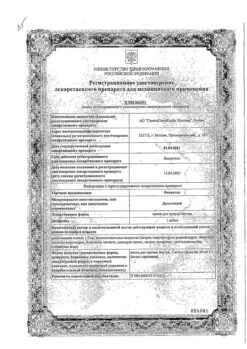
Manufacturer
Manufacturer
H.Uriyah, Spain
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a dry, light-protected place at a temperature not exceeding 25 °C |
| Manufacturer | J. Uriah, Spain |
| Medication form | pills |
| Brand | J. Uriah |
Related products
Buy Rupafin, 10 mg tablets, 7 pcs. with delivery to USA, UK, Europe and over 120 other countries.