No products in the cart.
Rovamycin, 1.5 ml ml 16 pcs
€32.43 €28.10
Description
Pharmacotherapeutic group: antibiotic, macrolide.
The ATX code is J01FA02.
Pharmacological action
Pharmacodynamics
- Spiramycin belongs to the antibiotic group of macrolides.
- Commonly susceptible microorganisms: minimum suppressive concentration (MSC) Moderately susceptible microorganisms: the antibiotic is moderately active in vitro. Positive results may be seen at antibiotic concentrations in the inflammatory site higher than the MAC (see Pharmacokinetics). Neisseria gonorrhoea, Clostridium perfringens, Ureaplasma urealyticum.
- Resistant microorganisms (MPC > 4 mg/L): at least 50% of strains of varieties are resistant.
The antibacterial spectrum of spiramycin is as follows:
Methicillin – resistant Staphylococcus aureus, Enterobacteria, Pseudomonas, Acinetobacter, Nocardia asteroides, Fusobacterium,, Haemophilus, Mycoplasma hominis.
Spiramycin activity against Toxoplasma gondii has been proven in vitro and in vivo.
Note: due to lack of clinical indications some varieties of bacteria are not listed in the spectrum. In France, 20% to 25% of pneumococci are resistant to all macrolides (cross-resistance to all macrolides).
Spiramycin penetrates and accumulates in phagocytes (neutrophils, monocytes and peritoneal and alveolar macrobacteriophages). In humans, concentrations of the drug within phagocytes are quite high. These properties explain the effects of spiramycin on intracellular bacteria.
Pharmacokinetics
Absorption
Absorption of spiramycin is rapid but not complete, with wide variability (10 to 60%).
Distribution
After oral administration of 6 million ME of spiramycin, the maximum plasma concentration is about 3.3 µg/ml.
Spiramycin does not penetrate the cerebrospinal fluid, but diffuses into breast milk. It penetrates the placental barrier (fetal blood concentration is about 50% of the concentration in maternal serum).
Concentrations in placental tissue are 5 times higher than the corresponding concentrations in blood serum.
The volume of distribution is approximately 383 liters.
The drug penetrates well into saliva and tissues (concentrations in lungs 20 to 60 µg/g, tonsils 20 to 80 µg/g, infected sinuses 75 to 110 µg/g, bones 5 to 100 µg/g). Ten days after the end of treatment, the concentration of the drug substance in the spleen, liver and kidneys is 5 to 7 µg/g.
The binding to plasma proteins is low (approximately 10%).
Biotransformation
Spiramycin is metabolized in the liver with the formation of active metabolites with an unspecified chemical structure.
Excretion
It is excreted mainly with bile (concentrations 15-40 times higher than in serum). Renal excretion of active spiramycin is about 10% of the administered dose.
The elimination half-life after administration of 3 million ME of spiramycin is approximately 8 hours. It may be prolonged in elderly patients. No adjustment of the spiramycin dose is necessary in patients with impaired renal function.
Indications
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to the drug:
– Acute and chronic pharyngitis caused by beta-haemolytic streptococcus A (as an alternative to treatment with beta-lactam antibiotics, especially if contraindicated for their use);
– acute sinusitis (given the sensitivity of the most common microorganisms that cause this pathology, the use of Rovamycin® is indicated if there are contraindications to the use of beta-lactam antibiotics);
– acute and chronic tonsillitis caused by spiramycin-sensitive microorganisms;
– acute bronchitis caused by a bacterial infection that developed after acute viral bronchitis;
– exacerbation of chronic bronchitis;
– community-acquired pneumonia in patients without risk factors for adverse outcome, severe clinical symptoms and clinical signs of pneumococcal etiology of pneumonia;
– pneumonia caused by atypical pathogens (such as Chlamydia pneumoniae, Chlamydia trachomatis, Mycoplasma pneumoniae, Legionella spp.) or suspected (regardless of severity and presence or absence of risk factors for adverse outcome);
– skin and subcutaneous tissue infections, including impetigo, impetiginosis, ecthyma, infectious dermohypodermitis (especially Roma), secondary infectious dermatoses, erythrazma;
– oral infections (including, but not limited to
– nongonococcal genital infections;
– toxoplasmosis, including in pregnancy;
– infections of the musculoskeletal system and connective tissue, including periodontal.
Prevention of recurrence of rheumatism in patients with allergies to beta-lactam antibiotics.
Eradication of Neisseria meningitidis from the nasopharynx (when contraindicated to take rifampicin) to prevent (but not treat) meningococcal meningitis:
– in patients after treatment and before leaving quarantine;
– in patients who have been in contact with persons who have excreted Neisseria meningitidis with saliva into the environment within 10 days before hospitalization.
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
The drug is taken orally.
Adults take 2-3 tablets of 3 million IU or 4-6 tablets of 1.5 million IU (i.e., 6-9 million IU) per day. Daily dose is divided into 2 or 3 doses. The maximum daily dose is 9 million IU.
In children and adolescents aged 6 to 18 years, only 1.5 million ME tablets should be used.
In children over 6 years of age, the daily dose is 150-300,000 ME per kg body weight divided into 2 or 3 doses to 6-9 million ME. The maximum daily dose in children is 300,000 ME per kg of body weight, but in children over 30 kg it should not exceed 9 million ME
In prophylaxis of meningococcal meningitis in adults 3 million ME 2 times a day for 5 days, in children 75,000 ME/kg of body weight 2 times a day for 5 days.
In patients with impaired renal function due to insignificant renal excretion of spiramycin no dose adjustment is required.
The tablets are taken orally with plenty of water.
Interaction
Interaction
Spiramycin inhibits carbidopa absorption with decreased plasma concentrations of levodopa. Clinical monitoring and dose adjustments of levodopa are required when spiramycin is concomitantly administered.
There have been numerous reported cases of increased activity of indirect anticoagulants in patients taking antibiotics. The type of infection or severity of the inflammatory reaction, age and general condition of the patient are predisposing risk factors. In such circumstances, it is difficult to determine the extent to which the infection itself or its treatment plays a role in MHO changes. However, with certain groups of antibiotics, this effect is observed more frequently, particularly with fluoroquinolones, macrolides, cyclines, sulfamethoxazole+trimethoprim combination, and some cephalosporins.
Special Instructions
Special Instructions
During treatment with the drug, liver function should be periodically monitored in patients with liver disease.
If generalized erythema and pustules with high body temperature occur at the start of treatment, acute generalized exanthematous pustulosis should be suspected; if this reaction occurs, treatment should be stopped, and further use of spiramycin, both in monotherapy and in combination, is contraindicated.
Pediatric use
The 3 million ME tablets are not indicated in children because of the difficulty in swallowing in children due to the large diameter of the tablets and the danger of airway obstruction.
Impact on the ability to drive and operate machinery
There are no reports of adverse effects of the drug on the ability to drive and engage in other potentially dangerous activities. However, the severity of the patient’s condition should be taken into account, which may affect attention and speed of psychomotor reactions. Therefore, the decision about the possibility of driving or engaging in other potentially hazardous activities in a particular patient must be made by the attending physician.
Contraindications
Contraindications
Side effects
Side effects
Overdose
Overdose
There are no known cases of spiramycin overdose.
Symptoms: nausea, vomiting, diarrhea are possible. Cases of prolongation of the QT interval, which resolves on withdrawal of the drug, have been observed in neonates receiving high doses of spiramycin or after IV administration of spiramycin in patients predisposed to prolongation of the QT interval.
Treatment: in case of overdose of spiramycin it is recommended ECG monitoring with determination of QT interval duration, especially in the presence of risk factors (hypokalemia, congenital prolongation of the QT interval, simultaneous use of drugs that prolong the QT interval and cause development of ventricular tachycardia of “pirouette” type). There is no specific antidote. In case of suspected spiramycin overdose, symptomatic therapy is recommended.
Pregnancy use
Pregnancy use
Rovamycin can be administered in pregnancy when indicated.
There is a wide experience of using the drug Rovamycin® in pregnancy. Reduction of the risk of transmitting toxoplasmosis to the fetus during pregnancy was observed from 25% to 8% when using the drug in the first trimester, from 54% to 19% in the second trimester and from 65% to 44% in the third trimester. No teratogenic or fetotoxic effects were observed.
Breastfeeding should be stopped if Rovamycin® is prescribed during lactation because spiramycin may penetrate into the breast milk.
Additional information
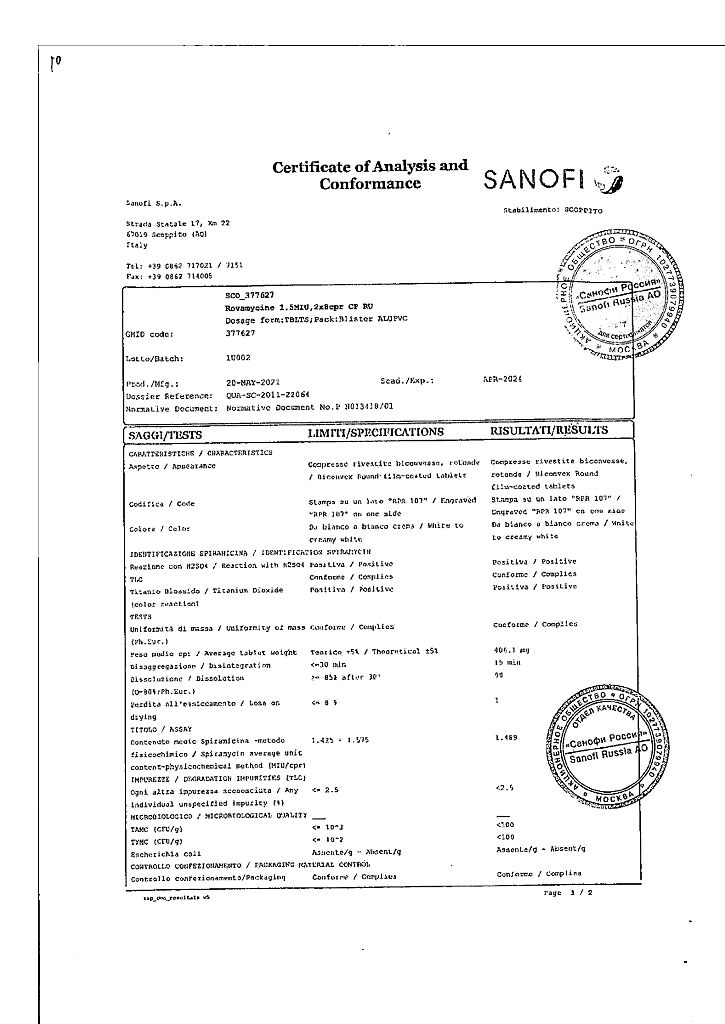
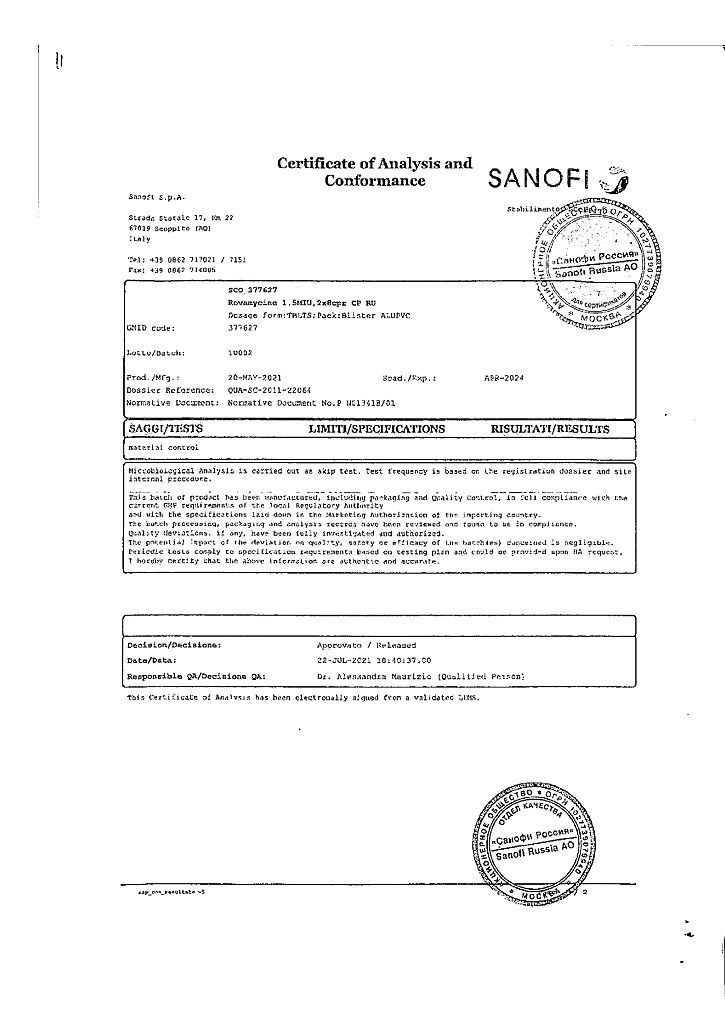
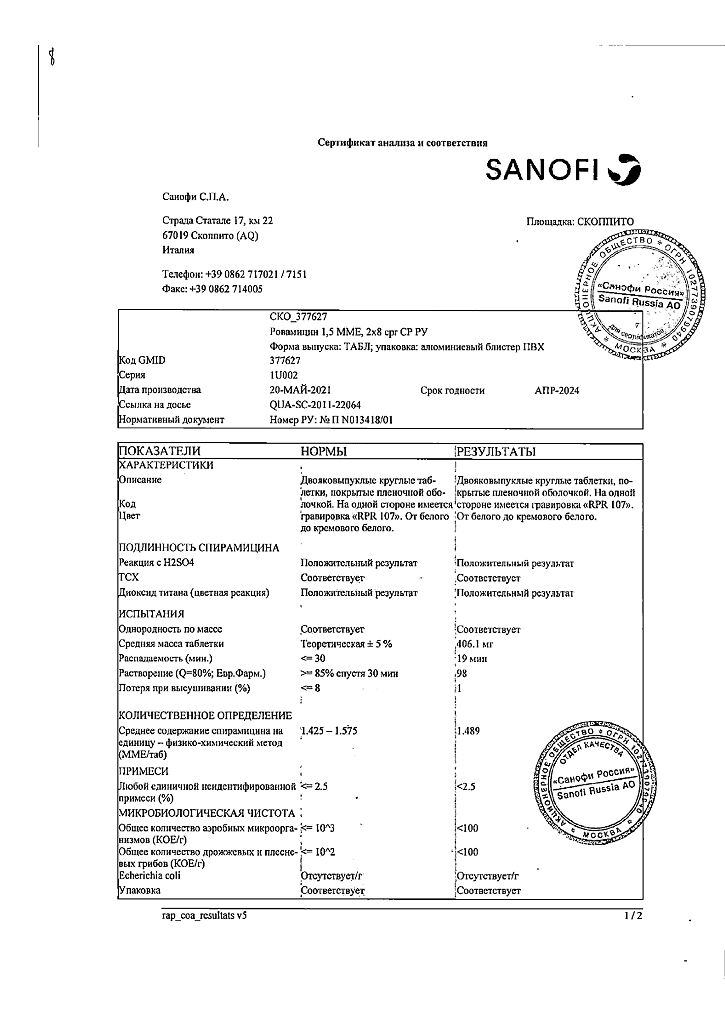
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | The drug should be kept out of reach of children at a temperature not exceeding 25 ° C. |
| Manufacturer | Sanofi S.p.A., Italy |
| Medication form | pills |
| Brand | Sanofi S.p.A. |
Related products
Buy Rovamycin, 1.5 ml ml 16 pcs with delivery to USA, UK, Europe and over 120 other countries.