No products in the cart.
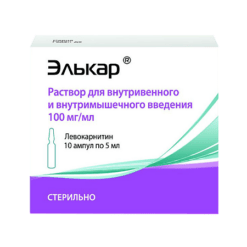
Rosulip Plus, 10 mg+10 mg capsules 30 pcs
€34.88 €30.23
Description
Pharmacotherapeutic group:Hypolipidemic combined agent (HMG-CoA reductase inhibitor+cholesterol absorption inhibitor)
ATC code: C10BA06
Pharmacological properties
Mechanism of action
Rosuvastatin
Rosuvastatin is a selective, competitive inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the enzyme that converts HMG-CoA to mevalonate, a precursor of cholesterol (CH). The main target of rosuvastatin action is the liver, where the synthesis of cholesterol and catabolism of low-density lipoproteins (LDL) take place.
Rosuvastatin increases the number of “hepatic” LDL receptors on the cell surface, increasing capture and catabolism of LDL, which in turn leads to inhibition of synthesis of very low density lipoproteins (VLDL), thus reducing the total amount of LDL and VLDL.
Ezetimibe
Ezetimibe is a representative of a new class of hypolipidemic agents that selectively inhibit the absorption of CH and some plant sterols in the intestine.
Pharmacodynamics
Rosuvastatin
Rosuvastatin reduces elevated concentrations of LDL-C, total cholesterol and triglycerides (TG), increases concentrations of high-density lipoprotein cholesterol (HDL-C) and decreases concentrations of apolipoprotein B (Apo B), low-density lipoprotein cholesterol (Non-LDL), HDL-C, TG-LDL-C, and increases apolipoprotein A-I concentration (Apo A-I) (see Tables 1 and 2). Table 1 and 2), decreases HC-LDL/ChC-LDL, total cholesterol/ChC-LDL and non-CLDL/ChC-LDL and Apo B/Apo A-I ratio.
Therapeutic effect is developed within one week after the treatment start. Within 2 weeks of therapy the efficacy reaches a level that is 90% of the maximum possible. The maximum therapeutic effect is usually reached by the 4th week of therapy and is maintained with regular use of the drug.
Table 1. Dose-dependent effect in patients with primary hypercholesterolemia (type ΙΙa and ΙΙb by Fredrickson classification) (mean adjusted percentage change from baseline).
Dose |
LDL-C | Total HC | HDL-C | TG |
Apo B | Apo A-Ι | |||||||||||||||||||||
Placebo | 13 | -7 |
3 | -3 | -7 | -3 | 0 | ||||||||||||||||||||
10 mg | 17 | -52 | -36 | 14 | | -48 | -42 | 4 | |||||||||||||||||||
20 mg | 17 | -55 | -40 | 8 < | -23 | -51 | -46 |
Table 2. Dose-dependent effect in patients with hypertriglyceridemia (type ΙΙb and ΙV according to Fredrickson classification) (mean percentage change from baseline).
Dose | strong>Number of patients | TG | HDL-C | Total HC | HDL-C | NonHDL-C | CHS-LLDP | TG-LDP | ||||
Placebo | 26 | 1 | 5 | 1 | -3 | 2 | 2 | 6 | ||||
10 mg | 23 | -37 | -45 | -40 | 8 | -49 | -48 | -39 | ||||
20 mg | 27 | -37 | -31 | -34 | 22 | -43 | -49 | -40 |
Clinical effectiveness
Rosuvastatin is effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia, regardless of race, sex or age, including patients with diabetes and familial hypercholesterolemia.
In 80% of patients with hypercholesterolemia of IIa and IIb types by Fredrickson classification (average baseline concentration of cholesterol-LDL is about 4.8 mmole/l) during the drug therapy in dose 10 mg cholesterol-LDL concentration reaches values less than 3 mmole/l.
In patients with homozygous familial hypercholesterolemia taking rosuvastatin at the doses of 20 mg and 40 mg the mean decrease of LDL-C concentration is 22%.
Patients with hypertriglyceridemia with initial TG concentrations of 273 to 817 mg/dL who received rosuvastatin at doses of 5 mg to 40 mg once daily for 6 weeks had significantly reduced plasma TG concentrations (see Table 2).
Additive effect is observed in combination with fenofibrate for TG concentration and with nicotinic acid at lipid-lowering doses for HDL-C concentration (see also section Cautionary Note).
Ezetimibe
Ezetimibe is effective when taken orally. Mechanism of action of ezetimibe differs from the mechanism of action of other classes of hypolipidemic agents (for example, HMG-CoA reductase inhibitors (statins), bile acid sequestrants, fibrates and plant statins). Molecular target of ezetimibe is Niemann-Pick C1-Like1 (NPC1-L1) transport protein, responsible for intestinal absorption of cholesterol and phytosterols.
ezetimibe is localized in small intestine brush border and prevents cholesterol absorption that leads to decrease of intestinal cholesterol reaching liver and due to this decrease of cholesterol reserve in liver and increase of phytosterol excretion from blood. Ezetimibe does not increase bile acid excretion (unlike bile acid sequestrants) and does not inhibit HC synthesis in the liver (unlike statins).
Statins reduce the synthesis of cholesterol in the liver. When used simultaneously, the drugs of these two groups provide additional reduction of cholesterol concentrations.
Ezetimibe used simultaneously with statins reduces the concentration of total cholesterol, LDL-C, apoB, non-HDL-C and TG, and increases plasma HDL-C concentration in patients with hypercholesterolemia to a greater extent than ezetimibe or statin used in monotherapy. Concomitant use of ezetimibe with fenofibrate reduces concentrations of total cholesterol, LDL-C, apoB, TG and non-HDL-C (calculated as the difference between total and HDL-C concentrations), and increases plasma HDL-C concentration in patients with hypercholesterolemia to a greater extent than ezetimibe or statin used in monotherapy.
Simultaneous use of ezetimibe with fenofibrate reduces end concentrations of total cholesterol, LDL-C, apo B, TG and non-HDL-C, and increases plasma HDL-C concentrations in patients with mixed hypercholesterolemia.
Clinical studies have shown that elevated concentrations of total cholesterol, LDL-C and apoB (the main protein component of LDL) contribute to the development of atherosclerosis. In addition, a decreased concentration of HDL-C is associated with the development of atherosclerosis. The results of epidemiological studies have shown that cardiovascular morbidity and mortality are directly related to the concentrations of total cholesterol and LDL-C and inversely related to HDL-C concentrations. Like LDL, lipoproteins rich in cholesterol and TG, including HDL, intermediate density lipoproteins (IDL) and remnants, may also contribute to atherosclerosis.
A series of preclinical studies were conducted to determine the selectivity of ezetimibe with regard to inhibiting cholesterol absorption.
Ezetimibe inhibited [14C]-CB absorption and had no effect on absorption of TGs, fatty acids, bile acids, progesterone, ethinylestradiol, or fat-soluble vitamins A and D.
Co-administration of rosuvastatin and ezetimibe
Adding ezetimibe to a stable dose of 5 mg or 10 mg of rosuvastatin resulted in a more pronounced decrease in LDL-C concentration compared with doubling the dose of rosuvastatin to 10 mg or 20 mg.Ezetimibe + rosuvastatin 5 mg lowered LDL-C concentration more than rosuvastatin 10 mg.
The efficacy and safety of rosuvastatin 40 mg in monotherapy and in combination with ezetimibe 10 mg in patients with high risk of coronary heart disease (CHD) were studied. Significantly more patients who received the combination rosuvastatin + ezetimibe, compared with rosuvastatin 40 mg monotherapy, achieved the target level of LDL-C concentration.Rosuvastatin 40 mg effectively improved the atherogenic lipid profile in this group of high-risk patients.
Children and adolescents
The European Medicines Agency has granted permission not to present the results of clinical trials of the combination rosuvastatin + ezetimibe in all age subgroups of children and adolescents in the treatment of elevated CHD concentrations (see
Pharmacokinetics
Absorption and distribution
Rosuvastatin
Maximum plasma concentration of rosuvastatin (Cmax) is reached approximately 5 hours after oral administration. Absolute bioavailability is approximately 20%.
Rosuvastatin is metabolized primarily by the liver, which is the main site of CH synthesis and metabolism of LDL-C. The volume of distribution (Vd) of rosuvastatin is approximately 134 liters. Approximately 90% of rosuvastatin is bound to plasma proteins, mainly to albumin.
Ezetimibe
After oral administration ezetimibe is rapidly absorbed and extensively metabolized in the small intestine and liver by conjugation into pharmacologically active phenolic glucoronide (ezetimibe-glucuronide). Cmax of ezetimibe-glucuronide is observed after 1-2 hours, of ezetimibe after 4-12 hours. Absolute bioavailability of ezetimibe cannot be determined since the substance is virtually insoluble in none of the aqueous solvents used for preparation of solutions for injection.
Food intake (low- or high-fat) did not affect the bioavailability of ezetimibe when taken orally as 10 mg tablets. Ezetimibe can be used regardless of meal times.
Ezetimibe and ezetimibe-glucuronide bind to plasma proteins by 99.7% and 88-92%, respectively.
Concomitant use of rosuvastatin at a dose of 10 mg and ezetimibe at a dose of 10 mg was accompanied by an increase in the area under the “concentration-time” curve (AUC) of rosuvastatin in patients with hypercholesterolemia (see Table 3).
Metabolism
Rosuvastatin
Subjected to limited metabolism (about 10%). Rosuvastatin is a non-core substrate for metabolism by isoenzymes of cytochrome P450 system. The main isoenzyme involved in metabolism of rosuvastatin is CYP2C9 isoenzyme. CYP2C19, CYP3A4 and CYP2D6 isoenzymes are less involved in metabolism.
The main identified metabolites of rosuvastatin are N-desmethyl and lactone metabolites. N-desmethyl is approximately 50% less active than rosuvastatin; lactone metabolites are pharmacologically inactive. More than 90% of pharmacological activity for inhibition of circulating HMG-CoA reductase is provided by rosuvastatin, the rest by its metabolites.
Ezetimibe
Metabolism of ezetimibe occurs primarily in the small intestine and liver by conjugation with glucuronide (phase II reaction) with subsequent excretion in the bile. Ezetimibe undergoes minimal oxidative metabolism (phase I reaction). Ezetimibe and ezetimibe-glucuronide (the main plasma derivatives of ezetimibe) constitute 10-20% and 80-90%, respectively, of the total plasma concentration of ezetimibe. Ezetimibe and ezetimibe-glucuronide are slowly eliminated from plasma by intestinal-hepatic recirculation. The half-life (T½) for ezetimibe and ezetimibe-glucuronide is approximately 22 hours.
Excretion
Rosuvastatin
About 90% of the dose of rosuvastatin is excreted unchanged through the intestine (including absorbed and unabsorbed rosuvastatin). The remainder is excreted by the kidneys. Plasma T1/2 is approximately 19 hours. The T1/2 does not change with increasing drug dose. Mean geometric plasma clearance is approximately 50 L/hour (coefficient of variation 21.7%). As in the case of other HMG-CoA reductase inhibitors, the membrane carrier of cholesterol is involved in “hepatic” uptake of rosuvastatin, which plays an important role in hepatic elimination of rosuvastatin.
Linearity
Systemic exposure of rosuvastatin increases in proportion to the dose. Pharmacokinetic parameters do not change with daily administration.
Ezetimibe
After oral administration of 20 mg of 14C-labeled ezetimibe, 93% of total ezetimibe (ezetimibe + ezetimibe-glucuronide) was detected in plasma of total radioactive product levels. Within 10 days, approximately 78% of the radioactive products ingested were excreted through the intestine with the bile, and 11% through the kidneys. After 48 hours no radioactive products were detected in blood plasma.
Pharmacokinetics in special groups of patients
Age and sex
Rosulip® Plus is contraindicated in children and adolescents under 18 years.
Gender and age have no clinically significant effect on the pharmacokinetics of rosuvastatin.
Pharmacokinetic parameters of ezetimibe were similar in children over 6 years old and adults. There are no pharmacokinetic data for children younger than 6 years.
In elderly patients (over 65 years) the plasma concentration of total ezetimibe is about 2 times higher than in young patients (18 to 45 years). The degree of reduction of LDL-C concentration and safety profile were comparable in elderly and younger patients receiving ezetimibe. No dose adjustment is required for elderly patients.
The plasma concentration of total ezetimibe is slightly higher in women (less than 20%) than in men. The degree of reduction of LDL-C concentration and safety profile are the same in men and women taking ezetimibe. Therefore, no dose adjustment is required for male or female patients.
Ethnic groups
Pharmacokinetic studies have shown approximately two-fold increase in median area under the curve “concentration-time” (AUC) and Cmax of rosuvastatin in Asian patients (Japanese, Chinese, Filipinos, Vietnamese and Koreans) compared to Europeans; in Indian patients a 1.3-fold increase in median AUC and Cmax was shown. Pharmacokinetic analysis revealed no clinically significant differences in pharmacokinetics among Europeans and members of the Negro race.
Renal insufficiency
In patients with mild to moderately severe renal insufficiency the plasma concentration of rosuvastatin or N-desmethyl does not change significantly. In patients with severe renal insufficiency (creatinine clearance (CK) < 30 ml/min) the plasma concentration of rosuvastatin is 3 times higher and that of N-desmethyl is 9 times higher than in healthy volunteers. Plasma concentration of rosuvastatin in patients on hemodialysis was approximately 50% higher than in healthy volunteers.
After a single dose of ezetimibe 10 mg in patients with severe renal dysfunction (n=8; IQ less than 30 ml/min/1.73 m2), the AUC value of total ezetimibe was increased approximately 1.5-fold compared to healthy volunteers (n=9). This result is not clinically significant. No dose adjustment is required for patients with impaired renal function.
In a patient after kidney transplantation who received complex therapy, including cyclosporine, the AUC of total ezetimibe increased 12-fold.
Liver failure
In patients with various stages of liver failure (with Child-Pugh score 7 and below) no increase in T1/2 of rosuvastatin was found. Two patients with Child-Pugh scores 8 and 9 showed at least 2-fold increase of T1/2. There is no experience of using rosuvastatin in patients with a Child-Pugh score above 9.
After a single dose of 10 mg ezetimibe, the mean AUC of total ezetimibe was 1.7 times greater in patients with mild hepatic impairment (Child-Pugh score 5-6) than in healthy volunteers. In a 14-day study of the use of ezetimibe at a dose of 10 mg per day involving patients with a moderate degree of liver failure (7-9 Child-Pugh scores), the mean AUC of total ezetimibe was increased 4-fold on days 1 and 14 compared with healthy volunteers.
No dose adjustment is required for patients with mild hepatic impairment. Since the consequences of increasing AUC value of total ezetimibe are unknown, ezetimibe is not recommended for patients with moderate to severe (more than 9 points by Child-Pugh scale) hepatic insufficiency (see section Caution).
Genetic polymorphisms
HMG-CoA reductase inhibitors, including rosuvastatin, bind to the transport proteins OATP1B1 (organic anion transport polypeptide involved in statin uptake by hepatocytes) and BCRP (efflux transporter). Carriers of SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA genotypes had 1.6 and 2.4-fold increased exposure (AUC) to rosuvastatin, respectively, compared with carriers of SLCO1B1 c.521T and ABCG2 c.421CC genotypes.
Indications
Indications
Primary hypercholesterolemia
The drug Rozulip® Plus is indicated in addition to the diet for patients with primary hypercholesterolemia (with the exception of heterozygous familial hypercholesterolemia).
Rosulip® Plus is prescribed as replacement therapy in patients whose lipid profile is adequately controlled by the simultaneous use of the individual drugs rosuvastatin and ezetimibe in doses equivalent to the corresponding doses in the fixed combination.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Combined lipid-lowering agent (HMG-CoA reductase inhibitor + cholesterol absorption inhibitor)
ATX code: C10BA06
Pharmacological properties
Mechanism of action
Rosuvastatin
Rosuvastatin is a selective, competitive inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, an enzyme that converts HMG-CoAb mevalonate, a precursor of cholesterol (C). The main target of action of rosuvastatin is the liver, where cholesterol synthesis and catabolism of low-density lipoproteins (LDL) take place.
Rosuvastatin increases the number of “liver” LDL receptors on the cell surface, increasing the uptake and catabolism of LDL, which in turn leads to inhibition of very low-density lipoprotein (VLDL) synthesis, thereby reducing the total amount of LDL and VLDL.
Ezetimibe
Ezetimibe is a member of a new class of lipid-lowering drugs that selectively inhibit the absorption of cholesterol and certain plant sterols in the intestine.
Pharmacodynamics
Rosuvastatin
Rosuvastatin reduces elevated concentrations of LDL-C, total cholesterol and triglycerides (TG), increases the concentration of high-density lipoprotein-C (HDL-C), and also reduces the concentration of apolipoprotein B (Apo B), low-density lipoprotein cholesterol (non-HDL-C), VLDL-C, VLDL-TG and increases the concentration of apolipoprotein A-I (Apo A-I) (see tables 1 and 2), reduces the ratio of LDL-C/HDL-C, total cholesterol/HDL-C and non-HDL-C/HDL-C and the Apo B/Apo A-I ratio.
The therapeutic effect develops within one week after the start of treatment. Within 2 weeks of therapy, the effectiveness reaches a level that is 90% of the maximum possible. The maximum therapeutic effect is usually achieved by the 4th week of therapy and is maintained with regular use of the drug.
Table 1. Dose response in patients with primary hypercholesterolemia (Fredrickson type ΙΙa and ΙΙb) (mean adjusted percentage change from baseline).
Dose
Number of patients
LDL-C
General HS
HDL-C
TG
Non-HDL cholesterol
Apo B
Apo A-Ι
Placebo
13
-7
-5
3
-3
-7
-3
0
10 mg
17
-52
-36
14
-10
-48
-42
4
20 mg
17
-55
-40
8
-23
-51
-46
5
Table 2. Dose response in patients with hypertriglyceridemia (Fredrickson type ΙΙb and ΙV) (mean percentage change from baseline).
Dose
Number of patients
TG
LDL-C
General HS
HDL-C
Non-HDL cholesterol
VLDL-C
TG-VLDL
Placebo
26
1
5
1
-3
2
2
6
10 mg
23
-37
-45
-40
8
-49
-48
-39
20 mg
27
-37
-31
-34
22
-43
-49
-40
Clinical effectiveness
Rosuvastatin is effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia, regardless of race, gender or age, including patients with diabetes mellitus and familial hypercholesterolemia.
In 80% of patients with type IIa and IIb hypercholesterolemia according to the Fredrickson classification (the average initial LDL-C concentration is about 4.8 mmol/l), when taking the drug at a dose of 10 mg, the LDL-C concentration reaches values of less than 3 mmol/L.
In patients with homozygous familial hypercholesterolemia taking rosuvastatin 20 mg and 40 mg, the average reduction in LDL-C concentrations is 22%.
In patients with hypertriglyceridemia with an initial TG concentration of 273 to 817 mg/dL who received rosuvastatin at a dose of 5 mg to 40 mg once daily for 6 weeks, the concentration of TG in the blood plasma was significantly reduced (see Table 2).
An additive effect is observed in combination with fenofibrate in relation to the concentration of TG and with nicotinic acid in lipid-lowering doses in relation to the concentration of HDL-C (see also section Special instructions).
Ezetimibe
Ezetimibe is effective when taken orally. The mechanism of action of ezetimibe differs from that of other classes of lipid-lowering agents (for example, HMG-CoA reductase inhibitors (statins), bile acid sequestrants, fibrates and plant stanols). The molecular target of ezetimibe is the Niemann-Pick C1-Like1 (NPC1L1) transport protein, which is responsible for the absorption of cholesterol and phytosterols in the intestine.
Ezetimibe is localized in the brush border of the small intestine and interferes with the absorption of cholesterol, which leads to a decrease in the supply of cholesterol from the intestine to the liver, thereby reducing cholesterol reserves in the liver and increasing the removal of cholesterol from the blood. Ezetimibe does not enhance the excretion of bile acids (unlike bile acid sequestrants) and does not inhibit the synthesis of cholesterol in the liver (unlike statins).
Statins reduce cholesterol synthesis in the liver. When used simultaneously, drugs from these two groups provide an additional reduction in cholesterol concentrations.
Ezetimibe, used concomitantly with statins, reduces the concentration of total cholesterol, LDL-C, ApoB, non-HDL-C and TG, and also increases the concentration of HDL-C in the blood plasma in patients with hypercholesterolemia to a greater extent than ezetimibe or a statin used in monotherapy. The simultaneous use of ezetimibe with fenofibrate reduces the concentrations of total cholesterol, LDL-C, ApoB, TG and non-HDL-C (calculated as the difference between the concentrations of total cholesterol and HDL-C), and also increases the concentration of HDL-C in the blood plasma in patients with hypercholesterolemia to a greater extent than ezetimibe or a statin used in monotherapy.
The simultaneous use of ezetimibe with fenofibrate reduces the concentrations of total cholesterol, LDL-C, Apo B, TG and non-HDL-C, and also increases the concentration of HDL-C in the blood plasma in patients with mixed hypercholesterolemia.
Clinical studies have shown that elevated concentrations of total cholesterol, LDL-C and ApoB (the main protein component of LDL) contribute to the development of atherosclerosis. In addition, reduced HDL-C concentrations are associated with the development of atherosclerosis. The results of epidemiological studies have shown that cardiovascular morbidity and mortality are directly related to the concentrations of total cholesterol and LDL-C and inversely related to the concentration of HDL-C. Like LDL, cholesterol- and TG-rich lipoproteins, including VLDL, intermediate-density lipoprotein (IDL), and remnant lipoproteins, may also contribute to the development of atherosclerosis.
A series of preclinical studies were conducted to determine the selectivity of ezetimibe for inhibition of cholesterol absorption.
Ezetimibe inhibited the absorption of [14C]-CS and had no effect on the absorption of TG, fatty acids, bile acids, progesterone, ethinyl estradiol, or fat-soluble vitamins A and D.
Concomitant use of rosuvastatin and ezetimibe
Adding ezetimibe to a stable dose of rosuvastatin 5 mg or 10 mg resulted in a more pronounced decrease in LDL-C concentrations compared with doubling the dose of rosuvastatin to 10 mg or to 20 mg. Ezetimibe + rosuvastatin 5 mg lowered LDL-C concentrations to a greater extent than rosuvastatin 10 mg.
The effectiveness and safety of the use of rosuvastatin 40 mg in monotherapy and in combination with ezetimibe 10 mg in patients with a high risk of coronary heart disease (CHD) was studied. Significantly more patients receiving the combination of rosuvastatin + ezetimibe, compared with rosuvastatin 40 mg monotherapy, achieved the target LDL-C concentration level. Rosuvastatin 40 mg effectively improved the atherogenic lipid profile in this group of high-risk patients.
Children and teenagers
The European Medicines Agency has granted permission not to present the results of clinical studies of the combination of rosuvastatin + ezetimibe in all age subgroups of children and adolescents in the treatment of elevated cholesterol concentrations (see section Dosage and Administration).
Pharmacokinetics
Absorption and distribution
Rosuvastatin
The maximum plasma concentration of rosuvastatin (Cmax) is achieved approximately 5 hours after oral administration. Absolute bioavailability is approximately 20%.
Rosuvastatin is metabolized primarily by the liver, which is the main site of cholesterol synthesis and LDL-C metabolism. The volume of distribution (Vd) of rosuvastatin is approximately 134 L. Approximately 90% of rosuvastatin is bound to plasma proteins, mainly albumin.
Ezetimibe
After oral administration, ezetimibe is rapidly absorbed and extensively metabolized in the small intestine and liver by conjugation to the pharmacologically active phenolic glucuronide (ezetimibe glucuronide). Cmax of ezetimibe glucuronide is observed after 1-2 hours, ezetimibe – after 4-12 hours. The absolute bioavailability of ezetimibe cannot be determined because this substance is practically insoluble in any of the aqueous solvents used to prepare solutions for injections.
Meal intake (low or high fat) did not affect the bioavailability of ezetimibe when administered orally as 10 mg tablets. Ezetimibe can be used regardless of meal time.
Ezetemibe and ezetimibe glucuronide are 99.7% and 88-92% bound to plasma proteins, respectively.
The simultaneous use of rosuvastatin at a dose of 10 mg and ezetimibe at a dose of 10 mg was accompanied by an increase in the area under the concentration-time curve (AUC) of rosuvastatin in patients with hypercholesterolemia (see Table 3).
Metabolism
Rosuvastatin
Subject to limited metabolism (about 10%). Rosuvastatin is a non-core substrate for metabolism by isoenzymes of the cytochrome P450 system. The main isoenzyme involved in the metabolism of rosuvastatin is the CYP2C9 isoenzyme. Isoenzymes CYP2C19, CYP3A4 and CYP2D6 are involved in metabolism to a lesser extent.
The main identified metabolites of rosuvastatin are N-desmethyl and lactone metabolites. N-desmethyl is approximately 50% less active than rosuvastatin; lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity of inhibiting circulating HMG-CoA reductase is provided by rosuvastatin, the rest by its metabolites.
Ezetimibe
Metabolism of ezetimibe occurs primarily in the small intestine and liver by conjugation with a glucuronide (phase II reaction) followed by excretion in the bile. Ezetimibe undergoes minimal oxidative metabolism (phase I reaction). Ezetimibe and ezetimibe glucuronide (the main ezetimibe derivatives detected in blood plasma) account for 10-20% and 80-90%, respectively, of the total concentration of ezetimibe in blood plasma. Ezetimibe and ezetimibe glucuronide are slowly eliminated from the blood plasma through enterohepatic recirculation. The half-life (T½) for ezetimibe and ezetimibe glucuronide is approximately 22 hours.
Removal
Rosuvastatin
About 90% of the dose of rosuvastatin is excreted unchanged through the intestine (including absorbed and unabsorbed rosuvastatin). The remaining part is excreted by the kidneys. Plasma T1/2 is approximately 19 hours. T1/2 does not change with increasing dose of the drug. The geometric mean plasma clearance is approximately 50 L/h (coefficient of variation 21.7%). As in the case of other HMG-CoA reductase inhibitors, the process of “hepatic” uptake of rosuvastatin involves a membrane cholesterol transporter, which plays an important role in the hepatic elimination of rosuvastatin.
Linearity
Systemic exposure of rosuvastatin increases in proportion to the dose. Pharmacokinetic parameters do not change with daily use.
Ezetimibe
After oral administration of 20 mg of 14C-labeled ezetimibe, 93% of the total ezetimibe (ezetimibe + ezetimibe glucuronide) of the total level of radioactive products was detected in the blood plasma. Within 10 days, approximately 78% of the radioactive products taken were excreted through the intestines with bile, 11% through the kidneys. After 48 hours, no radioactive products were detected in the blood plasma.
Pharmacokinetics in special groups of patients
Age and gender
Rozulip® Plus is contraindicated in children and adolescents under 18 years of age.
Gender and age do not have a clinically significant effect on the pharmacokinetics of rosuvastatin.
The pharmacokinetic parameters of ezetimibe were similar in children over 6 years of age and adults. There are no pharmacokinetic data for children under 6 years of age.
In elderly patients (over 65 years of age), the concentration of total ezetimibe in the blood plasma is approximately 2 times higher than in young patients (from 18 to 45 years of age). The degree of reduction in LDL-C concentrations and the safety profile were comparable in older and younger patients receiving ezetimibe. For elderly patients, dose selection is not required.
The concentration of total ezetimibe in blood plasma is slightly higher in women (less than 20%) than in men. The degree of reduction in LDL-C concentrations and the safety profile are similar in men and women taking ezetimibe. Therefore, dose selection of the drug is not required for male or female patients.
Ethnic groups
Pharmacokinetic studies have shown an approximately twofold increase in the median area under the concentration-time curve (AUC) and Cmax of rosuvastatin in patients of Asian nationality (Japanese, Chinese, Filipinos, Vietnamese and Koreans) compared with Europeans; in Indian patients, an increase in median AUC and Cmax was shown by 1.3 times. Pharmacokinetic analysis did not reveal clinically significant differences in pharmacokinetics between Europeans and blacks.
Kidney failure
In patients with mild to moderate renal failure, the plasma concentration of rosuvastatin or N-desmethyl does not change significantly. In patients with severe renal failure (creatinine clearance (CC) <30 ml/min.), the concentration of rosuvastatin in the blood plasma is 3 times higher, and the concentration of N-desmethyl is 9 times higher than in healthy volunteers. Plasma concentrations of rosuvastatin in hemodialysis patients were approximately 50% higher than in healthy volunteers.
After a single dose of ezetimibe at a dose of 10 mg in patients with severe renal impairment (n=8; CC not more than 30 ml/min/1.73 m2), the AUC value of total ezetimibe increased approximately 1.5 times compared to healthy volunteers (n=9). This result is not clinically significant. For patients with impaired renal function, dose selection is not required.
In a patient after kidney transplantation who received complex therapy, including cyclosporine, the AUC value of total ezetimibe increased 12-fold.
Liver failure
In patients with various stages of liver failure (with a score of 7 and below on the Child-Pugh scale), an increase in T1/2 of rosuvastatin was not detected. In two patients with scores of 8 and 9 on the Child-Pugh scale, an increase in T1/2 by at least 2 times was noted. There is no experience with the use of rosuvastatin in patients with a score above 9 on the Child-Pugh scale.
Following a single 10 mg dose of ezetimibe, the mean AUC of total ezetimibe was 1.7 times greater in patients with mild hepatic impairment (Child-Pugh score 5–6) than in healthy volunteers. In a 14-day study of ezetimibe 10 mg daily in patients with moderate hepatic impairment (Child-Pugh score 7–9), the mean AUC of total ezetimibe increased 4-fold on days 1 and 14 compared with healthy volunteers.
For patients with mild liver failure, no dose adjustment is required. Because the consequences of increasing total ezetimibe AUC are unknown, ezetimibe is not recommended in patients with moderate to severe (Child-Pugh score >9) hepatic impairment (see Precautions).
Genetic polymorphism
HMG-CoA reductase inhibitors, including rosuvastatin, bind to the transport proteins OATP1B1 (organic anion transport polypeptide involved in the uptake of statins by hepatocytes) and BCRP (efflux transporter). Carriers of the SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA genotypes had an increase in exposure (AUC) to rosuvastatin by 1.6 and 2.4 times, respectively, compared with carriers of the SLCO1B1 c.521TT and ABCG2 c.421CC genotypes.
Special instructions
Special instructions
Effect on skeletal muscles
In patients treated with all doses of rosuvastatin, and especially when taking doses >20 mg, effects of the drug on skeletal muscles were observed: for example, the development of myalgia, myopathy and (rarely) rhabdomyolysis. As with other HIG-CoA reductase inhibitors, the incidence of rhabdomyolysis with post-marketing use of rosuvastatin is higher when taking a dose of 40 mg.
In the post-registration period, cases of myopathy and rhabdomyolysis were observed with the use of ezetimibe. Rhabdomyolysis has been reported in very rare cases both with ezetimibe monotherapy and when ezetimibe is added to other medicinal products associated with an increased risk of rhabdomyolysis. If myopathy is suspected (based on muscle symptoms or increased CPK activity), ezetimibe, all statins, and any drugs known to be associated with increased rates of rhabdomyolysis should be immediately discontinued. At the beginning of treatment, all patients should be warned about the risk of myopathy and the need to promptly report any episodes of unreasonable muscle pain, muscle soreness or weakness (see section Adverse effects).
Effect on the liver
In controlled studies with co-administration of ezetimibe and a statin, consistent increases in transaminases (≥3 ULN) were observed.
It is recommended to determine liver function before starting treatment and 3 months after starting rosuvastatin therapy. Rosuvastatin should be discontinued or its dose reduced if serum transaminase activity is > 3xULN. The incidence of serious liver events (mainly increased transaminase activity) during post-registration use is more often observed when taking a dose of rosuvastatin of 40 mg.
In patients with secondary hypercholesterolemia caused by hypothyroidism or nephrotic syndrome, treatment of the underlying disease is necessary before starting therapy with Rozulip® Plus.
Due to the unknown effects of increased exposure to ezetimibe in patients with moderate or severe hepatic impairment, the use of Rozulip® Plus in them is not recommended (see Pharmacokinetics section).
Effect on the kidneys
Proteinuria, detected by rapid testing, predominantly of a tubular nature, was noted in patients receiving treatment with increased doses of rosuvastatin, in particular, a dose of 40 mg. In most cases, proteinuria was transient or inconsistent. Proteinuria has not been shown to signal the development of acute or progressive kidney disease (see Side Effects section). In the post-marketing period, serious renal adverse reactions were observed more frequently with the 40 mg dose. When monitoring patients taking the 40 mg dose, consider monitoring renal function (at least every 3 months).
Determination of creatine phosphokinase activity
CPK activity should not be determined after intense physical activity or if there are other likely reasons for increased CPK activity that may complicate the interpretation of the results.
If a significant increase in CPK activity is initially observed (5 ULN), a repeat measurement should be performed after 5–7 days. If repeated measurements confirm that CPK activity is 5 ULN, treatment should not be started.
Fusidic acid
Rosulip® Plus capsules should not be used in conjunction with fusidic acid for systemic use or within 7 days after discontinuation of fusidic acid treatment. In patients requiring treatment with fusidic acid, rosuvastatin should be discontinued throughout the entire treatment period. Rhabdomyolysis (in some cases fatal) has been reported in patients receiving rosuvastatin and fusidic acid together (see Interactions with Other Drugs). Patients should be informed to seek immediate medical attention if they develop muscle weakness, pain, or tenderness.
7 days after the last dose of fusidic acid, you can start treatment with rosuvastatin again.
In exceptional cases, when long-term treatment with fusidic acid is necessary, for example, in severe infections, the decision on the need for combined use of fusidic acid and Rozulip® Plus should be made individually, weighing the potential risks of therapy and the possible benefits with careful monitoring of the patient’s condition.
Before starting treatment
Rozulip® Plus, like other drugs that contain HMG CoA reductase inhibitors, should be prescribed with caution to patients with factors predisposing to the development of myopathy or rhabdomyolysis:
Kidney failure;
Hypothyroidism;
Hereditary muscle diseases in personal or family history;
Toxic effect on muscles when using another HMG-CoA inhibitor or fibrate;
Alcohol abuse;
Age 70 years;
Situations in which it is possible to increase the levels of active substances in plasma (see section “Pharmacokinetics”);
Simultaneous use of fibrates.
In such patients, the risks and possible benefits of treatment need to be assessed, and clinical monitoring is recommended. Treatment should not be started if there is a significant initial increase in CPK activity (5 ULN).
During treatment
Patients should be asked to immediately report any unexplained muscle pain, weakness, or muscle spasms, especially if accompanied by general weakness or fever. CPK activity should be measured in these patients. Treatment should be discontinued if there is a noticeable increase in CPK activity (≥5 ULN) or in the presence of severe symptoms that cause daily discomfort (even with CPK activity ≥5 ULN). Routine monitoring of CK activity is not required in asymptomatic patients.
There are very rare reports of the development of immune-mediated necrotizing myopathy during or after treatment with statins, including rosuvastatin. Clinically, this disease is characterized by proximal muscle weakness and increased serum CPK activity, which persist despite statin discontinuation.
In clinical studies, there was no evidence of increased effects on skeletal muscles in a small number of patients concomitantly taking rosuvastatin and other lipid-lowering drugs. An increased incidence of myositis and myopathy was observed in patients concomitantly taking other HMG-CoA reductase inhibitors and fibric acid derivatives (including gemfibrozil), cyclosporine, nicotinic acid, azole antifungals, protease inhibitors or macrolide antibiotics. Gemfibrozil increases the risk of myopathy when taken together with certain HMG-CoA reductase inhibitors. Therefore, the combination of Rozulip® Plus and gemfibrozil is not recommended. The benefits of further lowering lipid levels when taking Rosulip® Plus and fibrates or niacin in combination should be carefully weighed against the possible risks of this combination of drugs.
Rosulip® Plus should not be used in patients with serious acute conditions that are likely to have myopathy or that predispose them to the development of renal failure due to rhabdomyolysis (for example, sepsis, hypotension, major surgery, trauma, severe metabolic, endocrine or electrolyte disorders, uncontrolled seizures).
Ethnicity of patients
Pharmacokinetic studies of rosuvastatin have shown increased drug exposure in Asian patients compared to Caucasian patients (see Dosage and Administration and Pharmacokinetics).
Protease inhibitors
Increased systemic exposure to rosuvastatin was observed in patients concomitantly taking rosuvastatin and various protease inhibitors in combination with ritonavir. Consideration should be given to both the lipid-lowering benefits of Rosulip® Plus in HIV-infected patients receiving protease inhibitors and the possibility of increased rosuvastatin plasma concentrations when initiating and titrating the dose of rosuvastatin. Concomitant use of the drug with some protease inhibitors is recommended only with dose adjustment of Rozulip® Plus (see sections Dosage and Administration and Pharmacokinetics).
Interstitial lung diseases
In exceptional cases, the development of interstitial lung diseases has been reported with some statins, especially with long-term therapy. Symptoms of these illnesses include a nonproductive cough and poor general health (fatigue, weight loss, and fever). If a patient is suspected of developing interstitial lung disease, statin therapy should be discontinued.
Diabetes mellitus
Some data suggest that drugs of the statin class increase blood glucose concentrations and, in some patients at high risk of developing diabetes mellitus, may lead to hyperglycemia, the level of which meets the formal definition of diabetes mellitus and requires the initiation of antidiabetic therapy. This risk, however, is outweighed by the reduction in vascular risk with statins and should therefore not be a reason to discontinue statin therapy. In patients at risk (fasting glucose concentration – 5.6–6.9 µmol/l, BMI >30 kg/m2, increased TG concentrations, hypertension), clinical and biochemical monitoring of diabetes mellitus should be carried out in accordance with national guidelines.
In the JUPITER study, the overall incidence of diabetes mellitus was reported to be 2.8% in the rosuvastatin group and 2.3% in the placebo group (predominantly in patients with fasting glucose concentrations of 5.6–6.9 mmol/L).
Fibrates
The safety and effectiveness of coadministration of ezetimibe and fibrates have not been established. If cholestasis is suspected in a patient taking Rozulip® Plus and fenofibrate, the gallbladder should be examined and this therapy should be discontinued (see sections Interactions with other medicinal products and Side effects).
Anticoagulants
If Rozulip® Plus is added to therapy with warfarin, another coumarin anticoagulant or fluindione, appropriate monitoring of the international normalized ratio (INR); see section Interactions with other medicinal products).
Cyclosporine:
see sections Contraindications and Interactions with other drugs.
Pediatric patients
The safety and effectiveness of Rozulip® Plus in persons under 18 years of age have not yet been established, and therefore the use of the drug in this age group is not recommended.
Liver diseases and alcohol consumption
Rozulip® Plus should be used with caution in patients with excessive alcohol consumption and/or a history of liver disease.
Impact on the ability to drive vehicles and operate machinery
No studies have been conducted to evaluate the effect of Rozulip® Plyusna on the ability to drive vehicles and operate machines, however, it should be noted that dizziness may occur during treatment.
Active ingredient
Active ingredient
Rosuvastatin, Ezetimibe
Composition
Composition
Composition per 1 capsule 5 mg+10 mg, 10 mg+10 mg, 20 mg+10 mg:
Tablet containing rosuvastatin:
Active ingredient: Rosuvastatin zinc (which corresponds to rosuvastatin) 5.34 mg (5.00 mg), 10.68 mg (10.00 mg), 21.36 mg (20.00 mg).
Excipients: Microcrystalline silicon cellulose* 68.71 mg, 63.33 mg, 126.67 mg; colloidal silicon dioxide anhydrous 0.06 mg, 0.11 mg, 0.22 mg; magnesium stearate 0.89 mg, 0.88 mg, 1.75 mg.
* – Composition of microcrystalline silicon cellulose: microcrystalline cellulose 98.0%, colloidal anhydrous silicon dioxide 2.0%.
Tablet containing 10 mg ezetimibe:
Active ingredient: Ezetimibe 10.00 mg.
Excipients: povidone K-25 5.00 mg, croscarmellose sodium 19.00 mg, microcrystalline cellulose 30.30 mg, mannitol 30.30 mg, sodium lauryl sulfate 4.40 mg, hyprolose 10.00 mg, magnesium stearate 1.00 mg.
Hard gelatin capsule (CONI–SNAP 0):** approx. 96.00 mg.
**- Composition of hard gelatin capsule (CONI–SNAP 0) 10 mg+10 mg, 20 mg+10 mg, capsule base/capsule cap:
Red iron oxide dye (E172) -/ -, -/0.16%; iron dye yellow oxide (E172) 0.18%/0.18%, 0.18%/0.30%; titanium dioxide (E171) 1.00%/1.00%, 1.00%/1.30%; gelatin up to 100%/up to 100%, up to 100%/up to 100%, respectively.
Composition of hard gelatin capsule (CONI–SNAP 0) 5 mg+10 mg, capsule base/capsule cap:
Iron dye yellow oxide (E172) -/0.18%; titanium dioxide (E171) 2.00%/1.00%; gelatin up to 100%/up to 100%.
Pregnancy
Pregnancy
The drug Rozulip® Plus is contraindicated during pregnancy and breastfeeding.
Women of reproductive age should use reliable methods of contraception.
Pregnancy
Since cholesterol and cholesterol biosynthesis products are important for fetal development, the potential risk of inhibiting HMG-CoA reductase outweighs the benefit of using the drug in pregnant women.
If pregnancy is diagnosed during therapy, the drug should be discontinued immediately.
There are no clinical data on the use of ezetimibe during pregnancy.
Animal studies of ezetimibe have shown no direct or indirect adverse effects on pregnancy, embryo/fetal development, childbirth or postnatal development. When ezetimibe was administered to pregnant rats in combination with lovastatin, simvastatin, pravastatin or atorvastatin, no teratogenic effects were observed. When administered to pregnant rabbits, defects in skeletal development in the fetus were observed with low frequency.
There are no clinical data on the use of ezetimibe during pregnancy, so caution should be exercised when prescribing the drug to pregnant women. If pregnancy occurs, the drug should be discontinued.
Breastfeeding period
In studies in rats, ezetimibe was found to be excreted in milk. There is no data on the excretion of rosuvastatin and ezetimibe in breast milk in women, therefore, during breastfeeding, the drug should be discontinued (see section Contraindications).
Fertility
There are no clinical data on the effect of ezetimibe on human fertility. Ezetimibe does not affect the fertility of male or female rats.
Contraindications
Contraindications
• Hypersensitivity to rosuvastatin, ezetimibe or any of the components/excipients in the drug;
• Active liver disease, including a persistent increase in serum transaminase activity and any increase in serum transaminase activity (> 3x the upper limit of normal (ULN));
• Moderate and severe liver failure (7-9 or more points on the Child-Pugh scale);
• Concomitant use of cyclosporine;
• In women: pregnancy, breastfeeding, lack of reliable methods of contraception in women with intact reproductive function;
• Severe renal dysfunction (creatinine clearance < 30 ml/min);
• Myopathy;
• Predisposition to the development of myotoxic complications;
• Children and adolescents under 18 years of age.
With caution
There is a risk of developing myopathy/rhabdomyolysis – renal failure, hypothyroidism, personal or family history of hereditary muscle diseases and a previous history of muscle toxicity when using other HMG-CoA reductase inhibitors or fibrates; excessive alcohol consumption; age over 65 years; conditions in which an increase in plasma concentration of rosuvastatin is noted; race (Asian race); simultaneous administration with fibrates (see section Pharmacokinetics); history of liver disease; sepsis; arterial hypotension; major surgery, trauma, severe metabolic, endocrine or electrolyte disturbances or uncontrolled seizures.
Caution should be exercised when used simultaneously with indirect anticoagulants (including warfarin and fluindione). Patients taking ezetimibe and fenofibrate concomitantly should be aware of the possible risk of developing gallbladder disease.
Children and teenagers
The effectiveness and safety of Rozulip® Plus in children under 18 years of age has not yet been established, therefore the use of this drug is not recommended in patients of this age group.
Patients with liver failure
There are no data and experience with the use of the drug in patients with a score above 9 on the Child-Pugh scale (see sections Pharmacodynamics and Special instructions).
Side Effects
Side Effects
Security Profile Summary
Adverse reactions observed when taking rosuvastatin are usually mild and go away on their own. According to controlled clinical studies, less than 4% of patients receiving rosuvastatin dropped out of the studies due to the development of adverse reactions.
In clinical studies of up to 112 weeks, 2,396 patients received ezetimibe 10 mg daily as monotherapy, 11,308 patients in combination with a statin, and 185 patients in combination with fenofibrate. Adverse reactions were moderate and reversible. The overall incidence of side effects, as well as the percentage of patients who dropped out of the study due to adverse reactions, were similar in the ezetimibe and placebo groups.
In clinical trials, 1200 patients were reported to have received combination treatment with rosuvastatin and ezetimibe. According to the literature, in patients with hypercholesterolemia, the most common adverse events associated with the combination of rosuvastatin + ezetimibe were increased activity of liver transaminases, gastrointestinal disorders and muscle pain. These are known side effects for these active ingredients. However, from the point of view of side effects, a pharmacodynamic interaction between rosuvastatin and ezetimibe cannot be completely excluded.
Tabular list of adverse reactions
The incidence of adverse events is presented as follows:
Often (> 1/100, 1/1000, 1/10,000, < 1/1,000); Very rare (< 1/10,000), Frequency unknown (cannot be determined from available data).
Organ System Classes, MedDRA
Often
Uncommon
Rarely
Very rarely
Unknown
Blood and lymphatic system disorders
thrombocytopenia2
thrombocytopenia5
Immune system disorders
hypersensitivity reactions, including Quincke’s edema2
hypersensitivity (including skin rash, urticaria, anaphylaxis and angioedema) 5
Endocrine disorders
systems
diabetes mellitus1, 2
Metabolic and nutritional disorders
decline
appetite3
Mental disorders
depression2.5
Nervous system disorders
headache2,4,
dizziness2
paresthesia4
polyneuropathy2,
loss
memory2
peripheral neuropathy2
sleep disorders (including insomnia and nightmares)2
dizziness5; paresthesia5
Violations by
vessels
tides3; increased blood pressure3
Violations by
respiratory system,
organs of the chest and mediastinum
cough3
cough2, shortness of breath2.5
Violations by
gastrointestinal tract
constipation2, nausea2, pain in
stomach2,3
diarrhea3; flatulence3
dyspepsia3; gastroesophageal reflux disease3; nausea3
dry mouth4; gastritis4
pancreatitis2
diarrhea2
pancreatitis5; constipation5
Disorders of the liver and biliary tract
increased activity of liver transamnase 2
jaundice2, hepatitis2
hepatitis5,
cholelithiasis5, cholecystitis5,
Skin and subcutaneous tissue disorders
skin itching2.4, skin rash2.4,
urticaria2,4
Stevens-Johnson syndrome2
erythema multiforme5
Violations by
musculoskeletal and connective tissue
myalgia2,4
arthralgia3; muscle spasms3;
neck pain3
back pain4; muscle weakness4; pain in limbs4
myopathy (including myositis) 2, rhabdo-myolysis2
arthralgia2
immune-mediated necrotizing myopathy2,
damage to the tendons, sometimes with their rupture2,
myalgia5; myopathy and rhabdomyolysis5
Renal and urinary tract disorders
hematuria2
Disorders of the reproductive system and mammary glands
gyneco-mastia2
General and administration site disorders
asthenia2
fatigue3
chest pain3,
pain3
asthenia4;
peripheral edema4
peripheral edema2
asthenia5
Influence on laboratory and instrumental results
research
increased activity of alanine aminotransferase (ALT) and/or
aspartate-
aminotransferases (AST)4
increased activity of ALT and/or AST 3;
creatine phosphokinase (CPK)3;
γ-glutamyl transfers (GGT)3;
deviations in biochemical indicators of liver function3
1For rosuvastatin, the frequency depends on the presence or absence of risk factors (fasting glucose concentration ≥ 5.6 mmol/l, body mass index (BMI) > 30 kg/m2, increased TG concentration, history of arterial hypertension (AH).
2Adverse reaction profile for rosuvastatin, based on data from clinical trials and widespread post-registration use.
3Adverse reactions during monotherapy with ezetimibe. (n=2396), were observed with greater frequency than when taking placebo (n=1159)
4Adverse reactions when taking ezetimibe with a statin (n=11308) were observed with a higher frequency than when taking a statin alone (N=9361).
5Additional adverse reactions when taking ezetimibe in the post-registration period. Because these adverse events were identified based on spontaneous reports, the frequency of these events is unknown and cannot be calculated.
As with other HMG-CoA reductase inhibitors, the incidence of adverse drug reactions tends to be dose dependent.
Effect on the kidneys: In patients treated with rosuvastatin, the appearance of proteinuria was noted, which was determined by the express method and was predominantly of a tubular nature. A change in proteinuria from “-/traces” initially to “++” or more was noted by 1% of patients at any time when taking doses of 10 and 20 mg and in approximately 3% of patients when taking a dose of 40 mg. When taking a dose of 20 mg, a slight increase in proteinuria of the “+” degree was noted with a background proteinuria level of “–/traces”. In most cases, proteinuria resolved spontaneously or decreased with continued therapy. Analysis of data from clinical trials and post-marketing use of the drug to date has not revealed a causal relationship between proteinuria and acute or progressive kidney disease.
Hematuria was observed in patients treated with rosuvastatin. Data from clinical studies show a low incidence of this phenomenon.
Effects on skeletal muscle: In patients treated with all doses of rosuvastatin, especially doses >20 mg per day, effects on skeletal muscle, such as myalgias, myopathy (including myositis) and, in rare cases, rhabdomyolysis, with or without the development of acute renal failure, were noted. In patients taking rosuvastatin, a dose-dependent increase in CPK activity was also noted. Most of these cases were of minor severity: asymptomatic and transient. If CPK activity increases (5 ULN), treatment should be interrupted.
Effect on the liver: As with other HMG-CoA reductase inhibitors, a dose-dependent increase in transaminase activity was observed in a small number of patients taking rosuvastatin. Most of these cases were of minor severity: asymptomatic and transient.
The following adverse events have been reported with the use of some statins:
• Sexual dysfunction
• In exceptional cases – interstitial lung diseases (especially with long-term therapy.
Frequency of reports of rhabdomyolysis, serious disorders of the liver (mainly increased activity of liver transaminases) and kidneys when taking 40 mg of rosuvastatin per day.
Hyperglycemia and increased concentrations of glycosylated hemoglobin have also been reported.
Laboratory indicators
In controlled monotherapy clinical trials, the incidence of clinically significant increases in serum transaminases (ALT and/or AST ≥3 ULN) was similar in the ezetimibe (0.5%) and placebo (0.3%) groups. In drug combination studies, the incidence of increase was 1.3% in patients treated with ezetimibe plus a statin and 0.4% in patients treated with a statin alone. These episodes of elevation were usually asymptomatic, were not associated with cholestasis, and transaminase activity values returned to baseline after cessation of treatment or during continued treatment (see section “Special Instructions”).
In clinical trials, CK elevations >10 ULN were observed in 4 of 1674 (0.2%) patients receiving ezetimibe alone, 1 of 786 (0.1%) patients receiving placebo, 1 of 917 patients (0.1%) receiving ezetimibe + a statin, and 4 of 929 patients (0.4%) receiving a statin alone. Compared with a matched control group (placebo or statin monotherapy), ezetimibe was not associated with an increased incidence of myopathy or rhabdomyolysis.
Pediatric patients
The safety and effectiveness of Rozulip® Plus in persons under 18 years of age have not been established (see Pharmacodynamics section).
Rosuvastatin:
In a 52-week clinical study of rosuvastatin, episodes of CK elevations >10 ULN and muscle symptoms after exercise were more common in children and adolescents compared with the frequency in adult patients. Otherwise, the safety profile of rosuvastatin in children and adolescents was similar to that in adults.
Ezetimibe:
Children and adolescents aged 6 to 17 years
In a study of children aged 6-10 years with hereditary heterozygous or non-hereditary hypercholesterolemia (n = 138), increases in AST and/or ALT (≥3X ULN) were observed in 1.1% of patients (1 patient) receiving ezetimibe and 0% receiving placebo. There were no increases in CPK activity (≥ 10 ULN) or cases of myopathy,
In a separate study of adolescents (10–17 years) with heterozygous familial hypercholesterolemia (n = 248), episodes of increased ALT and/or AST (≥3 ULN) were observed in 3% of patients (4 people) receiving ezetimibe and simvastatin, compared with 2% (2 people) in the simvastatin monotherapy group. As for the increase in CK ≥ 10 ULN, these values were 2% (2 people) and 0%, respectively. No cases of myopathy were noted.
These studies were not suitable for comparison of rare adverse drug reactions.
Reporting Suspected Adverse Reactions
Providing data on suspected adverse drug reactions is very important to enable continuous monitoring of the risk/benefit ratio of the drug. Health care professionals should provide information about any suspected adverse reactions to the contacts listed at the end of the instructions, as well as through the national reporting system.
Interaction
Interaction
Contraindications
Cyclosporine: With simultaneous use of rosuvastatin and cyclosporine, the AUC values of rosuvastatin were on average 7 times higher compared to values in healthy volunteers. This combination does not affect plasma concentrations of cyclosporine.
The combined use of Rozulip® Plus and cyclosporine is contraindicated.
In a study of eight renal transplant patients with creatinine clearance >50 mL/min on a constant dose of cyclosporine, a single dose of 10 mg ezetimibe resulted in a 3.4-fold (range 2.3 to 7.9-fold) increase in mean ezetimibe AUC compared with the AUC in a healthy control population from another study receiving ezetimibe alone (n=17). In another study, a kidney transplant patient with severe renal failure was given cyclosporine and many other drugs. This patient experienced a 12-fold increase in systemic exposure to ezetimibe compared with control participants receiving ezetimibe alone. In a two-arm crossover study conducted in twelve healthy participants, daily administration of 20 mg ezetimibe for 8 days + a single dose of 100 mg cyclosporine per day resulted in an average 15% increase in cyclosporine AUC (range: 10% decrease to 51% increase) compared with a single dose of 100 mg cyclosporine alone. There have been no controlled studies of the effect of co-administration of ezetimibe and cyclosporine on the effects of the latter in patients after kidney transplantation.
Not recommended combinations
Protease inhibitors: Although the exact mechanism of interaction is unknown, concomitant use of protease inhibitors may result in a significant increase in systemic exposure to rosuvastatin (see table). For example, in a pharmacokinetic study, coadministration of 10 mg rosuvastatin and a combination of two protease inhibitors (atazanavir 300 mg + ritonavir 100 mg) to healthy volunteers was associated with an approximately three-fold increase in rosuvastatin AUC and an approximately seven-fold increase in rosuvastatin Cmax. Concomitant use of rosuvastatin and certain combinations of protease inhibitors is possible only after careful assessment of rosuvastatin doses, adjusted based on the expected increase in rosuvastatin exposure. This dose combination is not suitable as first-line therapy. Combination treatment should only be started after selecting the appropriate dosage of rosuvastatin or both components.
Transporter protein inhibitors: Rosuvastatin is a substrate of several transporter proteins, including the liver uptake transporter OATP1B1 and the efflux transporter BCRP. Concomitant use of Rosulip® Plus and drugs that inhibit these transporter proteins may lead to increased plasma concentrations of rosuvastatin and an increased risk of myopathy.
Gemfibrozil and other lipid-lowering drugs: the combined use of rosuvastatin and gemfibrozil leads to a 2-fold increase in the Cmax and AUC of rosuvastatin (see section “Special Instructions”). Based on specific interaction data, a pharmacokinetically significant interaction with fenofibrate is not expected, but a pharmacodynamic interaction is possible.
Gemfibrozil, fenofibrate, other fibrates and lipid-lowering doses of niacin (nicotinic acid 1 g/day or higher) increased the risk of myopathy when used concomitantly with HMG-CoA reductase inhibitors, possibly due to the fact that they can cause myopathy when used in monotherapy.
Clinicians should be aware that patients taking ezetimibe and fenofibrate are at risk of developing gallstones and gallbladder disease. If cholestasis is suspected in a patient taking ezetimibe and fenofibrate, examination of the gallbladder is indicated, as well as discontinuation of this therapy. Coadministration of fenofibrate and gemfibrozil increased total ezetimibe concentrations (approximately 1.5-fold and 1.7-fold, respectively). The combined use of ezetimibe with other fibrates has not been studied. Fibrates can increase the excretion of cholesterol into bile, leading to cholelithiasis. In animal studies, ezetimibe sometimes (not in all animal species) increased cholesterol concentrations in gallbladder bile. It cannot be excluded that the therapeutic use of ezetimibe is associated with the risk of developing cholelithiasis.
Fusidic acid:
When fusidic acid is used systemically with statins, the risk of myopathy, including rhabdomyolysis, may increase. The mechanism of this interaction (whether it is pharmacodynamic and/or pharmacokinetic) has not yet been elucidated. Cases of rhabdomyolysis, some fatal, have been reported in patients receiving these combinations. If treatment with fusidic acid is necessary, then statins should be discontinued throughout the entire period of treatment with fusidic acid (see section Special instructions).
Other interactions
Antacids: simultaneous use of rosuvastatin and antacid suspensions containing aluminum and magnesium hydroxide leads to a decrease in plasma concentrations of rosuvastatin by approximately 50%. This effect is less pronounced if antacids are used 2 hours after taking rosuvastatin. The clinical significance of this interaction has not been studied.
Erythromycin: simultaneous use of rosuvastatin and erythromycin leads to a decrease in AUC of rosuvastatin by 20% and Cmax of rosuvastatin by 30%. This interaction may occur as a result of increased intestinal motility caused by erythromycin.
Cytochrome P450 isoenzymes: the results of invivo and invitro studies showed that rosuvastatin is neither an inhibitor nor an inducer of cytochrome P450 isoenzymes. In addition, rosuvastatin is a weak substrate for these isoenzymes. Therefore, interaction of rosuvastatin with other drugs at the metabolic level involving cytochrome P450 isoenzymes is not expected.
There was no clinically significant interaction of rosuvastatin with fluconazole (an inhibitor of the CYP2C9 and CYP3A4 isoenzymes) and ketoconazole (an inhibitor of the CYP2A6 and CYP3A4 isoenzymes).
Preclinical studies have shown that ezetimibe does not induce cytochrome P450 drug metabolizing enzymes. No clinically significant pharmacokinetic interactions were noted between ezetimibe and drugs metabolized by cytochromes P450: 1A2, 2D6, 2C8, 2C9, 3A4 – or N-acetyltransferase
Vitamin K antagonists: As with other HMG-CoA reductase inhibitors, initiating or increasing the dose of rosuvastatin in patients concomitantly taking vitamin K antagonists (heparin or other coumarin anticoagulants) may result in an increase in the international normalized ratio (INR). Discontinuation or dose reduction of rosuvastatin may result in a decrease in the INR. In such situations, appropriate INR monitoring is advisable.
Ezetimibe (10 mg once daily) did not affect warfarin bioavailability or prothrombin time in a study of twelve healthy adult men. There are, however, reports of increases in international normalized ratio in patients when ezetimibe is added to warfarin or fluindione. If Rosulip® Plus is added to warfarin, another coumarin anticoagulant or fluindione, INR monitoring should be carried out accordingly (see section Special instructions).
Oral contraceptives and hormone replacement therapy (HRT): Concomitant use of rosuvastatin and oral contraceptives increased the AUC of ethinyl estradiol and norgestrel by 26% and 34%, respectively. This increase in plasma drug levels should be taken into account when adjusting dosages of oral contraceptives. There are no pharmacokinetic data available for concomitant use of rosuvastatin and HRT, and therefore a similar interaction cannot be excluded. However, this combination has been well studied in clinical studies in women and was well tolerated.
In clinical drug interaction studies, ezetimibe did not affect the pharmacokinetics of oral contraceptives that included ethinyl estradiol and levonorgestrel.
Cholestyramine: Concomitant use of cholestyramine decreased the mean area under the pharmacokinetic curve (AUC) of the sum of ezetimibe and its glucuronide by approximately 55%. This interaction may interfere with the consistent reduction in low-density lipoprotein cholesterol (LDL-C) when ezetimibe is added to cholestyramine therapy (see Dosage and Administration).
Statins: No clinically significant pharmacokinetic interactions were observed when ezetimibe was co-administered with atorvastatin, simvastatin, pravastatin, lovastatin, fluvastatin or rosuvastatin.
Other medicinal products: Based on data obtained from drug interaction studies, no clinically significant interaction is expected between rosuvastatin and digoxin.
In clinical drug interaction studies, ezetimibe did not affect the pharmacokinetics of dapsone, dextromethorphan, digoxin, glipizide, tolbutamide, or midazolam. Cimetidine, when taken together with ezetimibe, did not affect the bioavailability of the latter.
Interactions with drugs that require dose adjustment of rosuvastatin (see Table 3)
When co-administration of rosuvastatin and other drugs that increase the systemic exposure of rosuvastatin is required, dose adjustment of the latter is necessary. If the expected increase in exposure (AUC) is 2 times or greater, start rosuvastatin at a dose of 5 mg/day. The maximum daily dose of rosuvastatin should also be adjusted so that the expected systemic exposure of rosuvastatin does not exceed that for a dose of 40 mg taken without the simultaneous administration of drugs that interact with rosuvastatin. For example, the maximum daily dose of rosuvastatin when used simultaneously with gemfibrozil is 20 mg (increased exposure by 1.9 times), with ritonavir/atazanavir – 10 mg (increased exposure by 3.1 times).
Table 3.
Effect of concomitant therapy on rosuvastatin exposure (AUC, data in descending order) – results of published clinical studies
Dosage regimen of the drug with which rosuvastatin interacts
Dosage regimen
rosuvastatin
Change in rosuvastatin AUC*
Cyclosporine 75–200 mg 2 times a day, 6 months
10 mg 1 time/day, 10 days
7.1 times ↑
Regorafenib 160 mg, 1 time/day, 14 days
5 mg, once
3.8 times ↑
Atazanavir 300 mg + ritonavir 100 mg 1 time/day, 8 days
10 mg, once
3.1 times ↑
Lopinavir 400 mg + ritonavir 100 mg 2 times a day, 17 days
20 mg 1 time/day, 7 days
2.1 times ↑
Simeprevir 150 mg 1 time/day, 7 days
10 mg once
2.8 times ↑
Elbasvir 50 mg + grazoprevir 200 mg once a day
10 mg once
2.26 times ↑**
Grazoprevir 200 mg once daily
10 mg once
1.59 times ↑**
Clopidogrel 300 mg once and 75 mg every 24 hours
20 mg, once
2 times ↑
Gemfibrozil 600 mg 2 times a day, 7 days
80 mg, once
1.9 times ↑
Eltrombopag 75 mg 1 time/day, 10 days
10 mg, once
1.6 times ↑
Darunavir 600 mg + ritonavir 100 mg 2 times a day, 7 days
10 mg 1 time/day, 7 days
1.5 times ↑
Tipranavir 500 mg + ritonavir 200 mg 2 times a day, 11 days
10 mg, once
1.4 times ↑
Dronendarone 400 mg 2 times/day
No data
1.4 times ↑
Itraconazole 200 mg 1 time/day, 5 days
10 mg, once
1.4 times ↑***
Fosamprenavir 700 mg + ritonavir 100 mg 2 times a day, 8 days
10 mg, once
↔
Aleglitazavir 0.3 mg, 7 days
40 mg, 7 days
↔
Silymarin 140 mg 3 times/day, 5 days
10 mg, once
↔
Fenofibrate 67 mg 3 times/day, 7 days
10 mg, 7 days
↔
Rifampin 450 mg 1 time/day, 7 days
20 mg, once
↔
Ketoconazole 200 mg 2 times/day, 7 days
80 mg, once
↔
Fluconazole 200 mg 1 time/day, 11 days
80 mg, once
↔
Erythromycin 500 mg 4 times a day, 7 days
80 mg, once
28% ↓
Baicalin 50 mg 3 times/day, 14 days
20 mg, once
47% ↓
*Data given as x-fold change is the ratio of AUC when taking a combination of drugs and rosuvastatin alone. The data given as % is the % difference relative to taking rosuvastatin alone.
↑ – increase, ↔ – no change, ↓ – decrease
** When used together with elbasvir or grazoprevir, the daily dose of rosuvastatin should not exceed 10 mg.
***Several interaction studies have been conducted with other dosages of rosuvastatin, the table shows the most significant change in AUC.
Overdose
Overdose
There is no data in the literature on an overdose of rosuvastatin.
There is no specific therapy in case of rosuvastatin overdose.
In clinical studies, ezetimibe 50 mg/day in 15 healthy participants for up to 14 days or 40 mg/day in 18 patients with primary hypercholesterolemia for up to 56 days was generally well tolerated. No toxicity was observed in animals following a single oral dose of ezetimibe (5000 mg/kg in rats and mice and 3000 mg/kg in dogs).
A few cases of ezetimibe overdose have been reported and are not usually associated with adverse events. Adverse events reported were not serious.
In case of overdose, symptomatic and supportive therapy should be provided. Liver function and CPK activity should be monitored. The benefit of hemodialysis is unlikely.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 ºС.
Keep out of the reach of children.
Shelf life
Shelf life
3 years
Do not use after the expiration date stated on the package.
Manufacturer
Manufacturer
EGIS, Hungary
Additional information
| Shelf life | 3 years Do not use after the expiration date on the package. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ºC. Keep out of reach of children. |
| Manufacturer | EGIS, Hungary |
| Medication form | capsules |
| Brand | EGIS |
Other forms…
Related products
Buy Rosulip Plus, 10 mg+10 mg capsules 30 pcs with delivery to USA, UK, Europe and over 120 other countries.