No products in the cart.
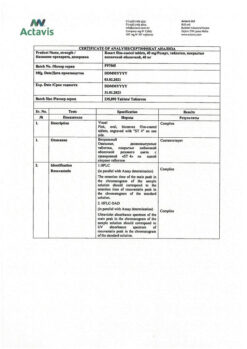
Rosart, 40 mg 30 pcs.
€43.65 €36.38
Description
Pharmacotherapeutic group
Hypolipidemic drug – HMG-CoA reductase inhibitor
ATX code: C10AA07
Pharmacological Properties
.Pharmacodynamics
Hypolipidemic drug from the group of statins. Selective competitive inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA)-reductase – the enzyme that converts HMG-CoA to mevalonate, a precursor of cholesterol.
increases the number of low-density lipoprotein (LDL) receptors on the surface of hepatocytes, which leads to increased capture and catabolism of LDL, inhibiting the synthesis of very low-density lipoprotein (VLDL), reducing the total amount of LDL and VLDL. Reduces elevated concentrations of LDL cholesterol, low-density lipoprotein cholesterol (non-LDL), LDL cholesterol, total cholesterol, triglycerides (TG), TG-LDL, apolipoprotein B (ApoB), decreases ratios of cholesterol-LDL/cholesterol-LDL, total cholesterol/cholesterol-LDL, cholesterol-non-LDL/cholesterol-LDL, apoB/apolipoprotein A-I (apoA-I), increases the concentration of cholesterol-LDL and apoA-I.
The hypolipidemic effect is directly proportional to the dose prescribed. The therapeutic effect appears within 1 week after the start of therapy, after 2 weeks it reaches 90% of the maximum, by 4 weeks it reaches the maximum and after that it remains constant. Effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia (regardless of race, sex or age), including patients with diabetes and familial hypercholesterolemia. In 80% of patients with hypercholesterolemia of IIa and IIb types (Fredrickson classification) with a mean baseline LDL-cholesterol index of about 4.8 mmol/l against the background of taking this medicine in dose 10 mg, LDL-cholesterol concentration reached values less than 3 mmol/l. In patients with homozygous familial hypercholesterolemia taking the drug in doses of 20 mg and 40 mg the average decrease of LDL-cholesterol concentration is 22%.
Additive effect is noted in combination with fenofibrate (with respect to decrease in TG concentration) and with nicotinic acid in lipid-lowering doses ≥1 g/day (with respect to increase in HDL cholesterol concentration).
Pharmacokinetics
Intake
The maximum concentration (Cmax) of rosuvastatin in plasma is reached approximately 5 h after drug administration. Absolute bioavailability is approximately 20%. Systemic exposure of rosuvastatin increases in proportion to the dose. Pharmacokinetic parameters do not change with daily administration.
Distribution
Rosuvastatin penetrates the placental barrier. Rosuvastatin is absorbed primarily by the liver, which is the main site of cholesterol synthesis and metabolism of LDL-C. The volume of distribution is 134 l. Binding to plasma proteins (predominantly to albumin) is approximately 90%.
Metabolism
Biotransformation in the liver is low (about 10%), being a non-core substrate for cytochrome P450 system isoenzymes. As in the case of other HMG-CoA reductase inhibitors, a specific membrane transporter, polypeptide transporting organic anion (OATP) 1B1, is involved in the hepatic uptake of the drug, which plays an important role in its hepatic elimination. The main isoenzyme involved in the metabolism of rosuvastatin is CYP2C9. CYP2C19, CYP3A4 and CYP2D6 isoenzymes are less involved in metabolism.
The main metabolites of rosuvastatin are N-desmethyl and lactone metabolites. N-desmethyl is about 50% less active than rosuvastatin; lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity for inhibition of circulating HMG-CoA reductase is provided by rosuvastatin, the rest by its metabolites.
Elimation
About 90% of the dose of rosuvastatin is excreted unchanged through the intestine, the remainder – by the kidneys. The elimination half-life (T1/2) is approximately 19 h and does not change with increasing dose of the drug. Mean plasma clearance is approximately 50 l/h (coefficient of variation 21.7%).
In patients with mild to moderately severe renal impairment plasma concentrations of rosuvastatin or N-desmethyl do not change significantly. In patients with severe renal impairment (creatinine clearance (CK) less than 30 ml/min), plasma concentrations of rosuvastatin are 3 times higher and N-desmethyl are 9 times higher than in healthy volunteers. Plasma concentrations of rosuvastatin in patients on hemodialysis are approximately 50% higher than in healthy volunteers.
In patients with various stages of hepatic failure with a Child-Pugh score of 7 or lower, no increase in T1/2 rosuvastatin; in patients with Child-Pugh scores 8 and 9 there was a prolongation of T1/2 by 2 times. There is no experience of using the drug in patients with more severe liver dysfunction.
Gender and age have no clinically significant effect on the pharmacokinetics of rosuvastatin. Pharmacokinetic parameters depend on race: the area under the curve “concentration-time” (AUC) in Japanese and Chinese is 2 times higher than that in Europe and North America. The average value of AUC and Cmax increases by a factor of 1.3 for mongoloids and Indians.
Indications
Indications
• Primary hypercholesterolemia (type IIa according to the Fredrickson classification), including heterozygous hereditary hypercholesterolemia or mixed (combined) hyperlipidemia (type IIb according to the Fredrickson classification), as an addition to diet and other non-pharmacological measures (physical activity and weight loss).
• Homozygous form of hereditary hypercholesterolemia when diet therapy and other treatments aimed at lowering lipid concentrations (for example, LDL apheresis) are insufficiently effective or if such treatments are not suitable for the patient.
• Hypertriglyceridemia (Fredrickson type IV) as an adjunct to diet.
• To slow the progression of atherosclerosis as an adjunct to diet in patients who are candidates for therapy to lower total and LDL cholesterol concentrations.
• Primary prevention of major cardiovascular complications (stroke, heart attack, arterial revascularization) in adult patients without clinical signs of coronary heart disease (CHD), but with an increased risk of its development (age over 50 years for men and over 60 years for women, increased concentration of C-reactive protein (≥2 mg/l) in the presence of at least one of the additional risk factors, such as arterial hypertension, low concentration HDL cholesterol, smoking, family history of early onset ischemic heart disease).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Lipid-lowering agent – HMG-CoA reductase inhibitor
ATX code: C10AA07
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics
A lipid-lowering drug from the group of statins. A selective competitive inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, an enzyme that converts HMG-CoA into mevalonate, a cholesterol precursor.
Increases the number of low-density lipoprotein (LDL) receptors on the surface of hepatocytes, which leads to increased uptake and catabolism of LDL, inhibition of the synthesis of very low-density lipoproteins (VLDL), reducing the total number of LDL and VLDL. Reduces elevated concentrations of LDL-cholesterol, low-density lipoprotein cholesterol (non-HDL), VLDL-cholesterol, total cholesterol, triglycerides (TG), VLDL-TG, apolipoprotein B (ApoB), reduces the LDL-cholesterol/HDL-cholesterol, total cholesterol/HDL-cholesterol ratios, non-HDL cholesterol/HDL cholesterol, ApoB/apolipoprotein A-I (ApoA-I), increases the concentration of HDL cholesterol and ApoA-I.
The lipid-lowering effect is directly proportional to the prescribed dose. The therapeutic effect appears within 1 week after the start of therapy, after 2 weeks it reaches 90% of the maximum, by 4 weeks it reaches a maximum and after that remains constant. Effective in adult patients with hypercholesterolemia with or without hypertriglyceridemia (regardless of race, sex or age), including patients with diabetes mellitus and familial hypercholesterolemia. In 80% of patients with type IIa and IIb hypercholesterolemia (Fredrickson classification) with an average initial LDL cholesterol level of about 4.8 mmol/l, when taking the drug at a dose of 10 mg, the concentration of LDL cholesterol reaches values less than 3 mmol/l. In patients with homozygous familial hypercholesterolemia taking the drug at a dose of 20 mg and 40 mg, the average reduction in LDL-cholesterol concentrations is 22%.
An additive effect is observed in combination with fenofibrate (in terms of reducing TG concentrations) and with nicotinic acid in lipid-lowering doses of ≥1 g/day (in terms of increasing HDL cholesterol concentrations).
Pharmacokinetics
Suction
The maximum concentration (Cmax) of rosuvastatin in blood plasma is reached approximately 5 hours after taking the drug. Absolute bioavailability is approximately 20%. Systemic exposure of rosuvastatin increases in proportion to the dose. Pharmacokinetic parameters do not change with daily use.
Distribution
Penetrates through the placental barrier. Rosuvastatin is absorbed primarily by the liver, which is the main site of cholesterol synthesis and LDL-C metabolism. Distribution volume – 134 l. Plasma protein binding (mainly albumin) is approximately 90%.
Metabolism
It is biotransformed in the liver to a small extent (about 10%), being a non-core substrate for isoenzymes of the cytochrome P450 system. As in the case of other HMG-CoA reductase inhibitors, a specific membrane transporter is involved in the process of hepatic uptake of the drug – organic anion transporting polypeptide (OATP) 1B1, which plays an important role in its hepatic elimination. The main isoenzyme involved in the metabolism of rosuvastatin is CYP2C9. Isoenzymes CYP2C19, CYP3A4 and CYP2D6 are involved in metabolism to a lesser extent.
The main metabolites of rosuvastatin are N-desmethyl and lactone metabolites. N-desmethyl is approximately 50% less active than rosuvastatin; lactone metabolites are pharmacologically inactive. More than 90% of the pharmacological activity of inhibiting circulating HMG-CoA reductase is provided by rosuvastatin, the rest by its metabolites.
Removal
About 90% of the dose of rosuvastatin is excreted unchanged through the intestines, the remainder by the kidneys. The half-life (T1/2) is approximately 19 hours, does not change with increasing doses of the drug. The average plasma clearance is approximately 50 l/h (coefficient of variation 21.7%).
In patients with mild to moderate renal failure, plasma concentrations of rosuvastatin or N-desmethyl do not change significantly. In patients with severe renal failure (creatinine clearance (CC) less than 30 ml/min), the plasma concentration of rosuvastatin is 3 times higher, and N-desmethyl is 9 times higher than in healthy volunteers. Plasma concentrations of rosuvastatin in hemodialysis patients are approximately 50% higher than in healthy volunteers.
In patients with various stages of liver failure with a score of 7 and below on the Child-Pugh scale, no increase in T1/2 of rosuvastatin was detected; in patients with scores of 8 and 9 on the Child-Pugh scale, a 2-fold prolongation of T1/2 was noted. There is no experience with the use of the drug in patients with more severe liver dysfunction.
Gender and age do not have a clinically significant effect on the pharmacokinetics of rosuvastatin. Pharmacokinetic parameters depend on race: the area under the concentration-time curve (AUC) in Japanese and Chinese is 2 times higher than that in residents of Europe and North America. In representatives of the Mongoloid race and Indians, the average value of AUC and Cmax increases by 1.3 times.
Special instructions
Special instructions
Effect on kidney function
In patients receiving high doses of rosuvastatin (mainly 40 mg), tubular proteinuria was observed during urine dipstick analysis, which in most cases was transient. This proteinuria did not indicate acute kidney disease or progression of kidney disease. The incidence of post-marketing reports of serious renal adverse reactions was higher in patients receiving rosuvastatin 40 mg.
When using the drug Rozart at a dose of 40 mg, it is recommended to monitor kidney function indicators during treatment.
Effect on the musculoskeletal system
Myalgia, myopathy and, in rare cases, rhabdomyolysis have been reported with all doses of rosuvastatin, and particularly with doses greater than 20 mg. In very rare cases, rhabdomyolysis has been reported while taking HMG-CoA reductase inhibitors and ezetimibe. In this case, a pharmacodynamic interaction cannot be excluded, so caution should be exercised when taking them together. As with other HMG-CoA reductase inhibitors, the incidence of post-marketing reports of rhabdomyolysis associated with rosuvastatin was higher with the 40 mg dose.
Determination of creatine phosphokinase
Determination of CPK activity should not be carried out after intense physical activity or in the presence of other possible reasons for an increase in its activity, which may lead to incorrect interpretation of the results obtained. If the initial CPK activity is significantly increased, a repeat measurement should be taken after 5-7 days; therapy should not be started if a repeat test confirms the initial CPK activity (5 times higher than normal).
Before starting therapy
Caution should be exercised when prescribing Rozart, as well as when prescribing other HMG-CoA reductase inhibitors, to patients with existing risk factors for the development of myopathy/rhabdomyolysis (see section Caution). It is necessary to consider the balance between the expected benefit of therapy and the potential risk and conduct clinical monitoring throughout the course of treatment. If the initial activity of CPK is significantly increased (5 times higher than the ULN), then treatment with the drug should not be started.
During treatment
The patient should be informed to immediately report to the doctor the unexpected onset of muscle pain, muscle weakness or cramps, especially in combination with malaise and fever. In such patients, CPK activity should be determined. Therapy should be discontinued if CPK activity is significantly increased (more than 5 times the ULN) or if muscle symptoms are severe and cause daily discomfort (even if CPK activity is 5 times less than the ULN). If symptoms disappear and CPK activity returns to normal, re-prescribing Rozart or other HMG-CoA reductase inhibitors in lower doses should be considered with careful monitoring of the patient. Routine monitoring of CPK activity in the absence of symptoms is impractical.
Very rare cases of immune-mediated necrotizing myopathy have been reported with clinical manifestations of persistent proximal muscle weakness and increased serum CPK activity during treatment or discontinuation of statins, including rosuvastatin.
There were no signs of increased effects on skeletal muscles when taking rosuvastatin and concomitant therapy. However, an increased incidence of myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibric acid derivatives (including gemfibrozil), cyclosporine, nicotinic acid in lipid-lowering doses >1 g/day, azole antifungals, protease inhibitors and macrolide antibiotics. Gemfibrozil increases the risk of developing myopathy when taken concomitantly with certain HMG-CoA reductase inhibitors, therefore the simultaneous use of gemfibrozil and rosuvastatin is not recommended. The ratio of expected benefits and potential risks should be carefully weighed when using the drug Rozart and fibrates or nicotinic acid in lipid-lowering doses >1 g/day together.
Taking the drug Rozart at a dose of 40 mg simultaneously with fibrates is contraindicated (see sections Interaction with other drugs and Contraindications).
During treatment, especially during the period of dose adjustment of the drug Rozart, the lipid profile should be monitored every 2-4 weeks and, according to it, the dose of the drug should be changed if necessary. The drug Rosart should not be taken by patients with acute and severe symptoms of myopathy or with the presence of risk factors predisposing to the development of impaired renal function and secondary rhabdomyolysis (for example, sepsis, arterial hypotension, major surgical interventions, trauma, severe metabolic disorders, severe endocrine disorders and severe disturbances of water and electrolyte balance, uncontrolled convulsions).
Effect on liver function
Like other HMG-CoA reductase inhibitors, rosuvastatin should be used with caution in patients who abuse alcohol and/or have a history of liver disease. It is recommended to determine liver function indicators before starting therapy and 3 months after starting therapy. Taking Rozart should be stopped or the dose reduced if the level of hepatic transaminase activity in the blood serum is 3 times higher than the ULN.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, treatment of underlying diseases should be carried out before starting treatment with Rozart. During post-marketing surveillance of rosuvastatin, the frequency of reports of the development of serious liver dysfunction (expressed mainly in increased activity of hepatic transaminases) was higher when taking a dose of 40 mg.
Ethnic groups
During pharmacokinetic studies among patients of the Mongoloid race, compared with Caucasians, an increase in the systemic concentration of rosuvastatin was noted (see section Dosage and Administration and Pharmacokinetics).
HIV protease inhibitors
During co-administration of rosuvastatin and a combination of various HIV protease inhibitors with ritonavir, an increase in the systemic concentration of rosuvastatin is observed. The decrease in blood lipid concentrations should be carefully assessed, and the possible increase in rosuvastatin in the blood plasma should also be taken into account at the beginning of treatment and during the period of increasing the dose of Rozart in patients with HIV taking HIV protease inhibitors. Concomitant use of HIV protease inhibitors is not recommended without dosage adjustment of rosuvastatin (see Dosage and Administration and Interactions with Other Drugs).
Interstitial lung disease
Isolated cases of interstitial lung disease have been reported with the use of certain HMG-CoA reductase inhibitors, especially over long periods of time. Manifestations of the disease may include shortness of breath, non-productive cough and deterioration in general health (weakness, weight loss and fever). If interstitial lung disease is suspected, therapy with HMG-CoA reductase inhibitors should be discontinued.
Diabetes mellitus type II
Some evidence suggests that HMG-CoA reductase inhibitors increase blood glucose concentrations and increase the likelihood of developing type 2 diabetes in some patients. However, this risk is outweighed by the ability of HMG-CoA reductase inhibitors to reduce the risk of vascular complications, so this fact is not a reason to interrupt treatment with rosuvastatin. It is necessary to establish clinical observation and conduct a biochemical blood test according to national standards in patients at risk of developing hyperglycemia (blood glucose concentration 5.6-6.9 mmol/l, body mass index >30 kg/m2, triglyceridemia, arterial hypertension). One study of rosuvastatin reported an overall incidence of diabetes mellitus of 2.8% in the rosuvastatin group and 2.3% in the placebo group, primarily in patients with fasting glucose 5.6 – 6.9 mmol/L.
Lactose intolerance
The drug Rozart should not be taken by patients with lactose intolerance, lactase deficiency and glucose-galactose malabsorption, since it contains lactose monohydrate.
Impact on the ability to drive vehicles and machinery.
No studies have been conducted to study the effect of rosuvastatin on the ability to drive vehicles and operate machinery. Patients should be careful when driving vehicles and engaging in potentially hazardous activities, as dizziness may occur during therapy.
Active ingredient
Active ingredient
Rosuvastatin
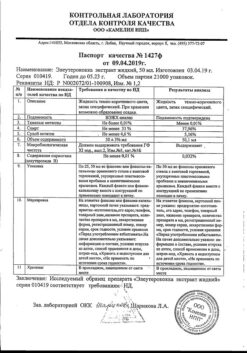
Composition
Composition
1 tablet 5 mg contains:
Active ingredient: rosuvastatin calcium 5.21 mg (in terms of rosuvastatin 5.00 mg);
Excipients: microcrystalline cellulose, type 102 11.55 mg, crospovidone, type A 3.50 mg, calcium hydrogen phosphate dihydrate 17.15 mg, lactose monohydrate 31.71 mg, magnesium stearate 0.88 mg;
Opadry white II 33G28435 ≈ 2.10 mg (hypromellose-2910 0.8400 mg, titanium dioxide 0.5250 mg, lactose monohydrate 0.4410 mg, macrogol-3350 0.1680 mg, triacetin 0.1260 mg).
1 tablet 10 mg contains:
Active ingredient: rosuvastatin calcium 10.42 mg (in terms of rosuvastatin 10.00 mg);
Excipients: microcrystalline cellulose, type 102 23.10 mg, crospovidone, type A 7.00 mg, calcium hydrogen phosphate dihydrate 34.30 mg, lactose monohydrate 63.42 mg, magnesium stearate 1.76 mg;
Opadry pink II 33G240007 ≈ 4.20 mg (hypromellose-2910 1.6800 mg, titanium dioxide 1.0441 mg, lactose monohydrate 0.8820 mg, macrogol-3350 0.3360 mg, triacetin 0.2520 mg, carmine red dye 0.0059 mg).
1 tablet 20 mg contains:
Active ingredient: rosuvastatin calcium 20.84 mg (in terms of rosuvastatin 20.00 mg);
Excipients: microcrystalline cellulose, type 102 46.20 mg, crospovidone, type A 14.00 mg, calcium hydrogen phosphate dihydrate 68.60 mg, lactose monohydrate 126.84 mg, magnesium stearate 3.52 mg;
Opadry pink II 33G240007 ≈ 8.40 mg (hypromellose-2910 3.3600 mg, titanium dioxide 2.0882 mg, lactose monohydrate 1.7640 mg, macrogol-3350 0.6720 mg, triacetin 0.5040 mg, carmine red dye 0.0118 mg).
1 tablet 40 mg contains:
Active ingredient: rosuvastatin calcium 41.68 mg (in terms of rosuvastatin 40.00 mg);
Excipients: microcrystalline cellulose, type 102 92.40 mg, crospovidone, type A 28.00 mg, calcium hydrogen phosphate dihydrate 137.20 mg, lactose monohydrate 253.68 mg, magnesium stearate 7.04 mg;
Opadry pink II 33G240007 ≈ 16.80 mg (hypromellose-2910 6.7200 mg, titanium dioxide 4.1765 mg, lactose monohydrate 3.5280 mg, macrogol-3350 1.3440 mg, triacetin 1.0080 mg, carmine red dye 0.0235 mg).
Pregnancy
Pregnancy
The drug Rozart is contraindicated during pregnancy and lactation.
The use of the drug Rozart in women of reproductive age is possible only if reliable methods of contraception are used and if the patient is informed about the possible risk of treatment to the fetus.
Since cholesterol and substances synthesized from cholesterol are important for fetal development, the potential risk of inhibiting HMG-CoA reductase outweighs the benefit of using the drug during pregnancy. If pregnancy is diagnosed during therapy with Rozart, the drug should be stopped immediately, and patients should be warned about the potential risk to the fetus.
There are no data regarding the excretion of rosuvastatin in breast milk, therefore, if it is necessary to use the drug during lactation, taking into account the possibility of adverse events in infants, the issue of stopping breastfeeding should be decided.
Contraindications
Contraindications
Contraindications for the drug Rozart in daily doses of 5, 10 and 20 mg:
Hypersensitivity to rosuvastatin or other components of the drug;
Liver diseases in the active phase, including a persistent increase in serum activity of “liver” transaminases (more than 3 times compared to the upper limit of normal (ULN));
Severe renal dysfunction (creatinine clearance less than 30 ml/min);
Myopathy;
Concomitant use of cyclosporine;
Use in women of reproductive age who do not use adequate methods of contraception;
Pregnancy and breastfeeding period;
Age up to 18 years (efficacy and safety have not been established);
Lactose intolerance, lactase deficiency, glucose-galactose malabsorption (the drug contains lactose monohydrate).
Contraindications for the drug Rozart in a daily dose of 40 mg:
Hypersensitivity to rosuvastatin or other components of the drug;
Liver diseases in the active phase, including a persistent increase in the serum activity of “liver” transaminases (more than 3 times compared to ULN);
Myopathy;
Concomitant use of cyclosporine;
Use in women of reproductive age who do not use adequate methods of contraception;
Pregnancy and breastfeeding period;
Age up to 18 years (efficacy and safety have not been established);
Lactose intolerance, lactase deficiency, glucose-galactose malabsorption (the drug contains lactose monohydrate);
Myotoxicity due to a history of taking other HMG-CoA reductase inhibitors or fibrates;
Hypothyroidism;
Renal failure of severe and moderate severity (creatinine clearance less than 60 ml/min);
Excessive alcohol consumption;
Conditions that can lead to increased plasma concentrations of rosuvastatin;
Concomitant use of fibrates;
Use in patients of the Mongoloid race;
Family or personal history of hereditary muscle diseases.
WITH CAUTION
For the drug Rozart in a daily dose of 5, 10 and 20 mg:
The presence of risk factors for the development of myopathy and/or rhabdomyolysis – renal failure (creatinine clearance more than 30 ml/min), hypothyroidism, personal or family history of hereditary muscle diseases and a previous history of myotoxicity when using other HMG-CoA reductase inhibitors or fibrates; excessive alcohol consumption, age over 70 years; conditions in which an increase in plasma concentration of rosuvastatin is noted; racial affiliation (Mongoloid race), simultaneous
use with fibrates, history of liver disease, sepsis, hypotension, major surgery, trauma, severe metabolic, endocrine or fluid-electrolyte disorders or uncontrolled epilepsy.
For the drug Rozart in a daily dose of 40 mg:
Presence of risk factors for the development of myopathy and/or rhabdomyolysis – renal failure (creatinine clearance more than 60 ml/min), age over 70 years; history of liver disease, sepsis, hypotension, major surgery, trauma, severe metabolic, endocrine or fluid-electrolyte disorders or uncontrolled epilepsy.
Use during pregnancy and breastfeeding
The drug Rozart is contraindicated during pregnancy and lactation.
The use of the drug Rozart in women of reproductive age is possible only if reliable methods of contraception are used and if the patient is informed about the possible risk of treatment to the fetus.
Since cholesterol and substances synthesized from cholesterol are important for fetal development, the potential risk of inhibiting HMG-CoA reductase outweighs the benefit of using the drug during pregnancy. If pregnancy is diagnosed during therapy with Rozart, the drug should be stopped immediately, and patients should be warned about the potential risk to the fetus.
There are no data regarding the excretion of rosuvastatin in breast milk, therefore, if it is necessary to use the drug during lactation, taking into account the possibility of adverse events in infants, the issue of stopping breastfeeding should be decided.
Side Effects
Side Effects
According to clinical studies of rosuvastatin, as well as data from its post-marketing use, the following adverse reactions were observed in patients.
The incidence of adverse reactions is given in accordance with the following classification: very often (³1/10); often (³1/100, <1/10); uncommon (³1/1000, <1/100); rare (³1/10000, <1/1,000); very rare (< 1/10000); frequency unknown (cannot be determined from available data).
Blood and lymphatic system disorders: rarely – thrombocytopenia.
Immune system disorders: rarely – hypersensitivity reactions, including angioedema.
Endocrine system disorders: often – diabetes mellitus1.
Mental disorders: frequency unknown – depression.
Nervous system disorders: often – headache, dizziness, asthenic syndrome; very rarely – polyneuropathy, memory loss; frequency unknown – peripheral neuropathy, sleep disorders, including insomnia and nightmares.
Disorders of the respiratory system, chest and mediastinal organs: frequency unknown – cough, shortness of breath.
Gastrointestinal disorders: often – constipation, nausea, abdominal pain; rarely – pancreatitis; frequency unknown – diarrhea.
Disorders of the liver and biliary tract: rarely – increased activity of “liver” transaminases; very rarely – hepatitis, jaundice;
Disorders of the skin and subcutaneous tissues: infrequently – itching, rash, urticaria; frequency unknown – Stevens-Johnson syndrome.
Musculoskeletal and connective tissue disorders: often – myalgia; rarely – myopathy (including myositis), rhabdomyolysis, lupus-like syndrome, muscle rupture; very rarely – arthralgia; frequency unknown – immune-mediated necrotizing myopathy; tendon damage, sometimes with ruptures,
Renal and urinary tract disorders: very rarely – hematuria.
Disorders of the genital organs and breast: very rarely – gynecomastia.
General disorders and disorders at the injection site: often – asthenic syndrome; frequency unknown – peripheral edema.
1Frequency depends on the presence of risk factors (fasting blood glucose concentration >5.6 mmol/l, body mass index >30 kg/m2, elevated TG concentration, history of arterial hypertension).
As with the use of other HMG-CoA reductase inhibitors, the incidence of adverse reactions is dose-dependent; side effects are usually mild and go away on their own.
Effect on kidney function
In patients receiving rosuvastatin, urine dipstick analysis revealed proteinuria, predominantly tubular. Changes in urinary protein (from none or trace amounts to ++ or more) were observed in less than 1% of patients receiving 10-20 mg rosuvastatin and in approximately 3% of patients receiving 40 mg rosuvastatin. A slight change in the amount of protein in the urine (from none or trace amounts to +) was noted with a dose of 20 mg. In most cases, proteinuria decreases or disappears during therapy and does not indicate the onset of acute or progression of existing kidney disease.
Hematuria has been observed in patients receiving rosuvastatin, and available data show a low incidence of this adverse reaction.
Effect on the musculoskeletal system
When using all doses of rosuvastatin, and especially when taking doses exceeding 20 mg, the development of myalgia, myopathy, including myositis, and in rare cases, rhabdomyolysis with
development of acute renal failure or without it.
When taking rosuvastatin, a dose-dependent increase in creatine phosphokinase (CPK) activity was observed. In most cases it was minor, asymptomatic and temporary. If CPK activity increases (more than 5 times compared to ULN), therapy should be suspended (see section Special instructions).
Effect on liver function
In a small number of patients, when using rosuvastatin, a dose-dependent increase in the activity of “liver” transaminases is observed. In most cases it is small, asymptomatic and temporary.
When using some HMG-CoA reductase inhibitors,
sexual dysfunction, isolated cases of interstitial lung disease have been recorded (see section Special instructions).
The frequency of reports of the development of rhabdomyolysis, serious impairment of renal and liver function (expressed mainly in increased activity of “liver” transaminases) is higher when taking a dose of rosuvastatin 40 mg.
Interaction
Interaction
The effect of the use of other drugs on rosuvastatin
Transport protein inhibitors
Rosuvastatin binds to certain transport proteins, in particular OATP1B1 and BCRP. Concomitant use of drugs that are inhibitors of these transport proteins may be accompanied by an increase in plasma concentrations of rosuvastatin and an increased risk of developing myopathy (see Table 1 and sections “Dosage and Administration” and “Special Instructions”).
Cyclosporine
With simultaneous use of rosuvastatin and cyclosporine, the AUC of rosuvastatin was on average 7 times higher than the value observed in healthy volunteers (see Table 1). Rosuvastatin does not affect the plasma concentration of cyclosporine. Rosuvastatin is contraindicated in patients taking cyclosporine (see section “Contraindications”).
Human immunodeficiency virus (HIV) protease inhibitors
Although the exact mechanism of interaction is unknown, concomitant use of HIV protease inhibitors and rosuvastatin may result in a significant increase in rosuvastatin exposure (see Table 1). A pharmacokinetic study of co-administration of 20 mg rosuvastatin with a combination drug containing two HIV protease inhibitors (400 mg lopinavir/100 mg ritonavir) in healthy volunteers resulted in approximately two-fold and five-fold increases in rosuvastatin AUC(0-24) and Cmax, respectively. Therefore, the simultaneous use of rosuvastatin and HIV protease inhibitors is not recommended (see Table 1 and sections “Method of administration and dosage”, “Special instructions”).
Gemfibrozil and other lipid-lowering drugs
The simultaneous use of rosuvastatin and gemfibrozil leads to an increase in Cmax in blood plasma and AUC of rosuvastatin by 2 times (see section “Special instructions”). Based on specific interaction data, a pharmacokinetically significant interaction between rosuvastatin and fenofibrate is not expected, but a pharmacodynamic interaction is possible.
Gemfibrozil, fenofibrate, other fibrates and lipid-lowering doses of nicotinic acid increased the risk of myopathy when used concomitantly with HMG-CoA reductase inhibitors, possibly due to the fact that these drugs can cause myopathy when used in monotherapy (see section “Special Instructions”). When taking rosuvastatin simultaneously with gemfibrozil, fibrates, nicotinic acid in lipid-lowering doses (more than 1 g/day), an initial dose of the drug of 5 mg is recommended for patients. It is contraindicated to take rosuvastatin at a dose of 40 mg simultaneously with fibrates (see sections “Contraindications”, “Method of administration and dosage”, “Special instructions”).
Ezetimibe
Simultaneous use of rosuvastatin at a dose of 10 mg and ezetimibe at a dose of
10 mg in patients with hypercholesterolemia resulted in an increase in rosuvastatin AUC (see Table 1). An increased risk of side effects due to the pharmacodynamic interaction between rosuvastatin and ezetimibe cannot be excluded.
Antacids
The simultaneous use of rosuvastatin and antacid suspensions containing magnesium hydroxide and aluminum hydroxide leads to a decrease in the concentration of rosuvastatin in the blood plasma by approximately 50%. This effect is less pronounced if antacids are used 2 hours after taking rosuvastatin. The clinical significance of this interaction has not been studied.
Erythromycin
The simultaneous use of rosuvastatin and erythromycin led to a decrease in rosuvastatin AUC by 20% and rosuvastatin Cmax by 30%. This interaction may occur as a result of increased intestinal motility caused by erythromycin.
Cytochrome P450 isoenzymes
The results of studies conducted in vivo and in vitro showed that rosuvastatin is neither an inhibitor nor an inducer of cytochrome P450 isoenzymes. In addition, rosuvastatin is a weak substrate for these isoenzymes. Therefore, interaction of rosuvastatin with other drugs at the metabolic level involving cytochrome P450 isoenzymes is not expected. There was no clinically significant interaction between rosuvastatin and fluconazole (an inhibitor of CYP2C9 and CYP3A4 isoenzymes) and rosuvastatin with ketoconazole (an inhibitor of CYP2A6 and CYP3A4 isoenzymes).
Fusidic acid
No studies have been conducted to study the interaction of rosuvastatin and fusidic acid. As with other statins, there have been post-marketing reports of rhabdomyolysis with co-administration of rosuvastatin and fusidic acid. Careful monitoring of patients is necessary. If necessary, it is possible to temporarily stop taking rosuvastatin.
Interaction with drugs requiring dose adjustment of rosuvastatin (see Table 1)
If it is necessary to use rosuvastatin in combination with other drugs that increase the exposure of rosuvastatin, the dose of rosuvastatin should be adjusted. You should read the instructions for use of these drugs before prescribing them together with rosuvastatin. The initial dose of rosuvastatin should be 5 mg once daily if the exposure (AUC) of rosuvastatin is expected to increase by 2-fold or more. The maximum daily dose of rosuvastatin should also be adjusted so that the expected exposure to rosuvastatin does not exceed that of a 40 mg dose taken without concomitant administration of drugs that interact with rosuvastatin. For example, when used simultaneously with gemfibrozil, the maximum daily dose of rosuvastatin is 20 mg (increased exposure by 1.9 times), when used with the combination of ritonavir/atazanavir – 10 mg (increased exposure by 3.1 times).
Table 1. Effect of co-prescribed medicinal products on rosuvastatin exposure (AUC, in descending order of magnitude) according to published clinical studies.
Dosage regimen of the interacting drug
Rosuvastatin dosage regimen
Change in AUC
rosuvastatin
Cyclosporine 75-200 mg 2 times a day, 6 months
10 mg once a day, 10 days
7.1x magnification
Regorafenib 160 mg once daily, 14 days
5 mg once
3.8x magnification
Atazanavir 300 mg/ritonavir 100 mg once a day, 8 days
10 mg once
3.1x magnification
Simeprevir 150 mg once a day, 7 days
10 mg once
2.8x magnification
Velpatasvir 100 mg once daily
10 mg once
2.7x magnification
Ombitasvir 25 mg / paritaprevir 150 mg / ritonavir 100 mg once daily / dasabuvir 400 mg twice daily, 14 days
5 mg once
2.6x magnification
Grazoprevir 200 mg/elbasvir 50 mg once daily, 11 days
10 mg once
2.3x magnification
Glecaprevir 400 mg/pibrentasvir 120 mg once daily, 7 days
5 mg once a day, 7 days
2.2x magnification
Lopinavir 400 mg/ritonavir 100 mg 2 times a day, 17 days
20 mg once, 7 days
2.1x magnification
Clopidogrel 300 mg (loading dose), then 75 mg after 24 hours
20 mg once
2.0x magnification
Gemfibrozil 600 mg 2 times a day, 7 days
80 mg
once
1.9x magnification
Eltrombopag 75 mg once daily, 10 days
10 mg once
1.6x magnification
Darunavir 600 mg/ritonavir 100 mg 2 times a day, 7 days
10 mg once a day, 7 days
1.5 times magnification
Tipranavir 500 mg/ritonavir 200 mg 2 times a day, 11 days
10 mg once
1.4x magnification
Dronedarone 400 mg twice daily
No data
1.4x magnification
Itraconazole 200 mg once a day, 5 days
10 mg or 80 mg once
1.4x magnification
Ezetimibe 10 mg once daily, 14 days
10 mg once a day, 14 days
1.2 times magnification
Fosamprenavir 700 mg/ritonavir 100 mg 2 times a day, 8 days
10 mg once
No changes
Aleglitazar 0.3 mg, 7 days
40 mg, 7 days
No changes
Silymarin 140 mg 3 times a day, 5 days
10 mg once
No changes
Fenofibrate 67 mg 3 times a day, 7 days
10 mg, 7 days
No changes
Rifampin 450 mg once a day, 7 days
20 mg once
No changes
Ketoconazole 200 mg 2 times a day, 7 days
80 mg once
No changes
Fluconazole 200 mg once a day, 11 days
80 mg once
No changes
Erythromycin 500 mg 4 times a day, 7 days
80 mg once
28% reduction
Baikalin 50 mg 3 times a day, 14 days
20 mg once
47% reduction
The effect of rosuvastatin on other drugs
Vitamin K antagonists
Initiating rosuvastatin therapy or increasing the dose of the drug in patients receiving concomitant vitamin K antagonists (eg, warfarin) may lead to an increase in the international normalized ratio (INR). Discontinuation of rosuvastatin or reduction in its dose may lead to a decrease in INR. In such cases, INR monitoring is recommended.
Oral contraceptives/hormone replacement therapy (HRT)
Concomitant use of rosuvastatin and oral contraceptives increases the AUC of ethinyl estradiol and AUC of norgestrel by 26% and 34%, respectively. This increase in plasma concentration should be taken into account when selecting the dose of oral contraceptives. There are no pharmacokinetic data on the simultaneous use of rosuvastatin and HRT; therefore, the occurrence of a similar effect cannot be excluded. However, this combination was widely used during clinical trials and was well tolerated by patients.
Other medicines
No clinically significant interaction between rosuvastatin and digoxin is expected.
Overdose
Overdose
When taking several daily doses simultaneously, the pharmacokinetic parameters of rosuvastatin do not change.
Treatment: there is no specific treatment; symptomatic therapy and measures aimed at maintaining the function of vital organs and systems under the control of liver function and CPK activity are carried out. It is unlikely that hemodialysis will be effective.
Storage conditions
Storage conditions
Store at a temperature not exceeding 30 °C. Keep out of the reach of children!
Shelf life
Shelf life
2 years. Do not use after expiration date.
Manufacturer
Manufacturer
Actavis Ltd, Malta
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 30 ° C. Keep out of reach of children! |
| Manufacturer | Actavis Ltd, Malta |
| Medication form | pills |
| Brand | Actavis Ltd |
Other forms…
Related products
Buy Rosart, 40 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.