No products in the cart.
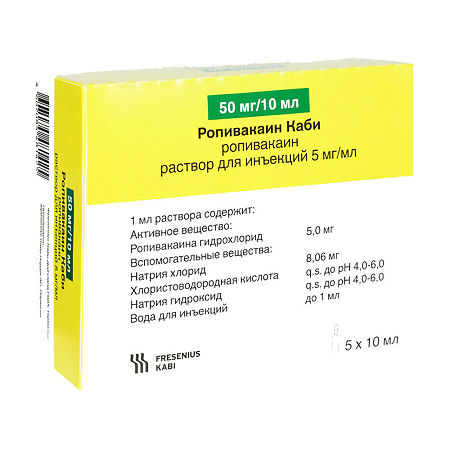
Ropivacaine Cabi, 5 mg/ml 10 ml 5 pcs
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 4607085481425
SKU: 336730
Categories: Anesthesia and resuscitation, Anesthesia solutions, Medicine
Description
A long-acting local anesthetic of the amide type, which is a pure enantiomer. It has both anesthetic and analgesic effect. By reversibly blocking potential-dependent Na+-channels it prevents generation of impulses in the endings of sensitive nerves and conduction of impulses along the nerve fibers. Signs of CNS toxicity precede signs of cardiovascular toxicity because they are observed at lower concentrations of the drug in plasma. Ropivacaine has a wide therapeutic range (range between therapeutic and toxic doses).
In vivo studies on animals have shown that ropivacaine has less toxic effects on the myocardium compared to bupivacaine. Indirect cardiovascular effects (arterial hypotension, bradycardia) may occur after epidural administration of ropivacaine and are due to the resulting sympathetic blockade.
The onset and duration of anesthesia with Ropivacaine Cabi depend on the concentration and site of administration of the drug.
Indications
Indications
At concentrations of 7.5 mg/1 ml and 10 mg/1 ml, Ropivacaine Cabi is used v adults and children over 12 years of age for the following indications:
Anesthesia in surgical procedures:
Intraarticular injection in knee arthroscopy.
At a concentration of 2 mg/1 ml, Ropivacaine Kabi is used for the following indications:
Capitation of acute pain syndrome in adults and children over 12 years of age.
Active ingredient
Active ingredient
How to take, the dosage
How to take, the dosage
For perineural administration (spinal and conduction anesthesia)
Intravenous catheters must be inserted before large blockades can be performed.
Ropivacaine Kabi is administered slowly or by increasing successive doses of the drug at a rate of 25-50 mg/min.
In order to prevent the anesthetic from entering the vessel, aspiration testing should always be performed prior to and during the administration of the drug. Accidental intravascular injection is recognized by a temporary increase in heart rate.
The following table is a guide to dosage selection for intrathecal blockade, acute pain relief, and peripheral nerve blocks. A minimum dosage sufficient to produce an effective block should be used. The clinical professional’s experience and knowledge of the patient’s physical condition is important in deciding which dose to use.
Ropivacaine Kabi dosing recommendations for adults and children older than 12 years (see Table 2). Table 2)
Table 2
Indications
Intrathecal blockade; surgical interventions
The dosing recommendations for Ropivacaine Kabi for children 1 to 12 years of age (see Table 3. Table 3)
Table 3
Indications
Acute pain syndrome management (intraoperative and postoperative); 5 0.5-0.6 2.5-3
The doses listed in the table are considered sufficient to achieve a reliable blockade and are indicative when using the drug in adults because there is individual variability.There is individual variability in the rate of block and its duration.
Intrathecal administration of ropivacaine hydrochloride has not been studied for anesthesia in caesarean section.
Individual differences occur with respect to the onset of the blockade and its duration.
The values in the Dose column represent an estimated average range of required doses. Please refer to the standard manuals for information about factors that affect block technique and individual patient characteristics.
In the absence of sufficient clinical evidence, we do not recommend the use of Ropivacaine Cabi in children less than 1 year of age.
Interaction
Interaction
This medicinal product should not be mixed with other medicinal products.
The concomitant use of Ropivacaine Cabi with local anesthetics, drugs structurally similar to local amide anesthetics or drugs depressing the central nervous system (CNS) may increase the toxic effects of the drugs.
In alkaline solutions, ropivacaine hydrochloride may precipitate because it is weakly soluble at pH >6.0).
Special Instructions
Special Instructions
Anesthesia must be performed by experienced specialists, in specially equipped rooms. The availability of equipment and medications for resuscitation measures is mandatory. The patient must have an intravenous catheter inserted before the conductive blocks are started.
The clinician must be familiar with precautions and have adequate experience in diagnosing and treating possible side effects, systemic toxicity and other complications, such as irreversible subarachnoid injection, which can cause severe spinal block with apnea and hypotension.
Convulsions are more likely to occur after brachial plexus block and epidural block. This can most likely be the result of accidental intravascular administration or rapid absorption at the injection site.
Peripheral nerve blocks may require large volumes of local anesthetic to areas with many vessels, often near major vessels, increasing the risk of intravascular injection and/or rapid systemic absorption, which can lead to high plasma concentrations.
Some local anesthetic procedures, such as head and neck injections, may be associated with an increased incidence of serious adverse reactions, regardless of the anesthetic used. Care must be taken to prevent injection in the area of inflammation.
Elderly and debilitated patients, patients with intracardiac conduction block of degree II and III, and patients with severe renal insufficiency require special attention, but local anesthesia is often indicated for these patients.
There have been isolated reports of cardiac arrest when using ropivacaine for epidural anesthesia or peripheral nerve block, especially after accidental intravascular injection in elderly patients and patients with comorbid heart disease.
In some cases, resuscitation measures may be difficult. If cardiac arrest, effective resuscitation may take a long time.
Ropivacaine is metabolized in the liver and therefore should be used with caution in patients with liver disease; repeated doses may need to be reduced due to delayed excretion.
There is usually no need to adjust the dosage in patients with renal and hepatic impairment during single or short-term therapy. However, acidosis and decreased plasma protein concentrations, often seen in patients with chronic renal failure, may increase the risk of systemic intoxication.
Spinal anesthesia may result in decreased blood pressure (BP) and bradycardia. Administration of vasoconstrictors or increased circulating blood volume may reduce the risk of these side effects. Arterial hypotension should be promptly corrected by administration of 5-10 mg of ephedrine; if necessary, the administration may be repeated.
Possible cross-sensitivities with other amide-type anesthetics should be taken into account – the type of local anesthetic should be taken into account.
Patients on a sodium-restricted diet should take into account the sodium content of the drug.
The use of the drug in concentrations above 5 mg/ml, as well as intrathecal administration of Ropivacaine Kabi in children has not been studied.
Ropivacaine Kabi Injection Solution may have porphyrinogenic properties and should only be used in patients diagnosed with acute porphyria if there is no safer alternative. If patients are hypersensitive, necessary precautions should be taken.
Indicate, if necessary, special precautions for the disposal of unused medications
The unused solution must be disposed of in accordance with the current drug disposal requirements of the hospital in question.
Potentially hazardous activities requiring increased attention and rapid psychomotor reactions should be refrained from, as motor function, motor coordination and reaction speed are temporarily impaired.
Contraindications
Contraindications
With caution
Elderly patients, patients in a weakened state or patients with severe comorbidities, including Grade II and III intracardiac conduction blockages (sinoatrial, atrioventricular, intraventricular), advanced liver disease, severe hepatic failure, severe chronic renal failure, acute porphyria, during therapy of hypovolemia, frail patients, elderly, childhood, pregnancy and during lactation.
The use of regional anesthesia is preferable for these groups of patients. When performing “large” blocks, in order to reduce the risk of severe adverse events, it is recommended to stabilize the patient’s condition beforehand and to adjust the anesthetic dose.
Caution should be exercised when injecting local anesthetics into the head and neck region because of the possible increased frequency of serious adverse events.
Patients on a sodium-restricted diet should consider the sodium content of the drug.
Side effects
Side effects
Adverse reactions to Ropivacaine Kabi are similar to those to other amide-type local anesthetics. Adverse reactions must be distinguished from physiological effects of the block itself, such as hypotension and bradycardia during subdural anesthesia, or effects associated with the technique of drug administration (e.g., spinal hematoma, local nerve damage, headache after subdural puncture, meningitis and epidural abscess).
Side effects common to local anesthetics
Central and peripheral nervous system disorders
Neuropathy and spinal cord dysfunction (anterior spinal artery syndrome, arachnoiditis, cauda equina syndrome) are possible, usually related to the technique of regional anesthesia rather than the action of the drug.
The accidental intrathecal administration of a dose in excess of the recommended dose may result in complete spinal block. Serious complications are possible with systemic overdose and unintentional intravascular administration of the drug (see section “Overdose”).
Acute systemic toxicity
Ropivacaine Kabi may cause acute systemic toxic reactions if high doses are used or if its blood concentration rises rapidly if the drug is inadvertently administered intravascularly or in overdose (see “Pharmacological properties” and “Overdose”).
The most frequently reported side effects of the drug
A variety of side effects have been reported, with the vast majority not related to the anesthetic agent used but to the regional anesthetic technique.
The most frequently reported adverse effects (>1%) were the following, which were considered to be clinically significant regardless of whether a causal relationship with anesthetic use was established: decreased BP*, nausea, bradycardia, vomiting, paresthesia, increased body temperature, headache, urinary retention, dizziness, chills, increased BP, tachycardia, hypoesthesia, anxiety.
The incidence of adverse effects is as follows: Very common – >1/10; common – >1/100 to <1/10; infrequent – >1/1000 to <1/100; rare – >1/10,000 to <1/1,000; very rare – <1/10,000; unknown – cannot be determined based on available data.
Nervous system disorders: frequent – headache, paresthesia, dizziness; infrequent – anxiety, symptoms of CNS toxicity (seizures, grand convulsive seizures, peroral paresthesia, tongue numbness, hyperacusis, tinnitus, visual disturbances, dysarthria, muscle twitching, tremor)*, hypoesthesia.
Chronic disorders: very common – decreased BP (hypotension); common – bradycardia, tachycardia, increased BP; infrequent – syncope; rare – cardiac arrest, arrhythmia.
Disorders of the respiratory system, thorax and mediastinum: infrequent – dyspnea, difficulty in breathing.
Gastrointestinal disorders: very common – nausea; common – vomiting.
River and urinary tract disorders: frequently – urinary retention.
General disorders and disorders with administration: frequently – back pain, hyperthermia, chills; infrequently – hypothermia; rarely – allergic reactions (anaphylactic reactions. angioedema and urticaria).
* These symptoms are usually associated with accidental intravascular administration, overdose, or rapid absorption.
a – Hypotension in children is common (>1/100).
b – Vomiting in children is very common (>1/10).
Overdose
Overdose
Acute systemic toxicity
Inadvertent intravascular administration during plexus blocks or other peripheral blockages has resulted in cases of seizures.
If an intrathecal epidural dose of anesthetic is inappropriately administered, a complete spinal block may occur.
The accidental intravascular administration of anesthetic may cause an immediate toxic reaction.
In case of overdose during regional anesthesia, symptoms of a systemic toxic reaction appear delayed 15-60 minutes after injection due to a slow increase in plasma concentration of the local anesthetic.
Systemic toxicity is primarily manifested by symptoms of the central nervous system (CNS) and cardiovascular system (CVS). These reactions are caused by high concentrations of the local anesthetic in the blood, which may occur due to (accidental) intravascular administration, overdose or exceptionally high adsorption from highly vascularized areas.
CNS reactions are similar for all amide-type local anesthetics, whereas cardiovascular reactions are more dependent on the injected drug and its dose.
Central nervous system
The central nervous system manifestations of systemic toxicity develop gradually: first there are visual disturbances, numbness around the mouth, tongue numbness, hyperacusis, tinnitus, dizziness. Dysarthria, tremors and muscle twitching are more serious manifestations of systemic toxicity and may precede the appearance of generalized seizures (these signs should not be mistaken for the patient’s neurotic behavior). With progression of intoxication there may be loss of consciousness, seizures lasting from several seconds to several minutes, accompanied by respiratory disorders, rapid development of hypoxia and hypercapnia due to increased muscle activity and inadequate ventilation. In severe cases, respiratory arrest may even occur. Arising acidosis, hyperkalemia, hypocalcemia increase toxic effects of anesthetic.
Thereafter, due to redistribution of the anesthetic from the CNS and its subsequent metabolism and excretion, there is a fairly rapid recovery of function, unless a large dose of the drug was administered.
Cardiovascular system
Cardiovascular system disorders are signs of more serious complications. Decreased BP, bradycardia, arrhythmias, and in some cases even cardiac arrest can occur due to high systemic concentrations of local anesthetics. In rare cases, cardiac arrest is not accompanied by preceding CNS symptoms. In studies on volunteers, intravenous infusion of ropivacaine resulted in inhibition of conduction and cardiac contractility.
The cardiovascular symptoms are usually preceded by CNS toxicity that may not be seen if the patient is under sedation (benzodiazepines or barbiturates) or general anesthesia.
In children, early signs of systemic toxicity of local anesthetics may be more difficult to detect due to difficulties in describing symptoms in children or when regional anesthesia is combined with general anesthesia.
The treatment of acute toxicity
In case of the first signs of acute systemic toxicity, the drug should be stopped immediately.
In case of convulsions and CNS depression symptoms, the patient requires adequate treatment to maintain oxygenation, arrest convulsions, maintain cardiovascular activity. Oxygenation with oxygen should be provided, and if necessary, transfer to artificial lung ventilation. If seizures do not stop after 15-20 seconds, anticonvulsants should be used: sodium thiopental 1-3 mg/kg IV (provides rapid relief of seizures) or diazepam 0.1 mg/kg IV (action is slower compared to that of sodium thiopental). Suxamethonium 1 mg/kg quickly stops seizures, but intubation and ventilatory support are required.
In case of depressed cardiovascular activity (decreased BP, bradycardia) intravenous injection of 5-10 mg of ephedrine is necessary, repeat the injection after 2-3 minutes if necessary. If circulatory failure or cardiac arrest develops, standard resuscitation measures should be started immediately. It is vital to maintain optimal oxygenation, ventilation and blood circulation, and to correct acidosis. Longer resuscitation interventions may be necessary in cardiac arrest.
In therapy of systemic toxicity in children, doses should be adjusted according to the patient’s age and body weight.
Additional information
| Shelf life | Polypropylene ampoules – 3 years. Do not use the product after the expiration date printed on the package. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ° C. Do not freeze. Store out of the reach of children. |
| Manufacturer | Fresenius Kabi Deutschland GmbH, Germany |
| Medication form | solution for injection |
| Brand | Fresenius Kabi Deutschland GmbH |
Related products
Buy Ropivacaine Cabi, 5 mg/ml 10 ml 5 pcs with delivery to USA, UK, Europe and over 120 other countries.