No products in the cart.
Roaccutane, 10 mg capsules 30 pcs
€56.32 €48.81
Description
Pharmacotherapeutic group: Acne treatment
ATX code [D10BA01]
Pharmacological action
Retinoid for the systemic treatment of acne
Isotretinoin is the stereoisomer of fully transretinoic acid (tretinoin).
The exact mechanism of action of Roaccutan® is not yet clear, but it has been established that improvement in the clinical picture of severe acne is associated with suppression of sebaceous gland activity and histologically confirmed reduction in their size. In addition, the anti-inflammatory effect of isotretinoin on the skin has been proven.
Hyperkeratosis of the epithelial cells of the hair follicle and sebaceous glands leads to the sloughing of root cells in the gland duct and to the blockage of the latter by keratin and excess sebum. This is followed by formation of a comedon and in some cases inflammatory process.
Roaccutane® inhibits the proliferation of sebocytes and works on acne by restoring normal cell differentiation. Sebum is a major substrate for Propionibacterium acnes growth, so reducing sebum production suppresses bacterial duct colonization.
Pharmacokinetics
Because the kinetics of isotretinoin and its metabolites are linear, plasma concentrations during therapy can be predicted from data obtained after a single dose. This property of the drug also indicates that it does not affect the activity of hepatic enzymes involved in drug metabolism.
Is absorption
The absorption of isotretinoin from the gastrointestinal tract varies. The absolute bioavailability of isotretinoin has not been determined because there is no human formulation for intravenous use. However, extrapolation of data obtained in an experiment in dogs suggests rather low and variable systemic bioavailability.
In acne patients, maximum plasma concentrations (Smax) in equilibrium after fasting administration of 80 mg of isotretinoin were 310 ng/mL (range 188-473 ng/mL) and were reached after 2-4 hours. Plasma concentrations of isotretinoin are approximately 1.7 times higher than blood concentrations, due to poor isotretinoin penetration into erythrocytes.
Eating isotretinoin with food increases bioavailability by a factor of 2 compared to fasting.
Distribution
Isotretinoin binds strongly (99.9%) to plasma proteins, primarily to albumin, so that in a wide range of therapeutic concentrations the free (pharmacologically active) fraction of the drug is less than 0.
The volume of distribution of isotretinoin in humans has not been determined because there is no intravenous dosage form.
The isotretinoin blood equilibrium concentrations (Cmin ss) in patients with severe acne who received 40 mg of the drug twice daily ranged from 120 to 200 ng/ml.
The 4-oxo-isotretinoin concentrations in these patients were 2.5 times greater than those of isotretinoin. There is insufficient data on tissue penetration of isotretinoin in humans. Concentrations of isotretinoin in the epidermis are half as high as in serum.
Metabolism
The three main metabolites found in plasma after oral administration are 4-oxo-isotretinoin, tretinoin (fully transretinoic acid) and 4-oxo-retinoin. The main metabolite is 4-oxo-isotretinoin, whose plasma concentrations in equilibrium are 2.5 times higher than those of the original drug. Less significant metabolites have also been found, including also glucuronides, but the structure of not all metabolites has been established.
The metabolites of isotretinoin have biological activity confirmed in several laboratory tests. Thus, the clinical effects of the drug in patients may be the result of the pharmacological activity of isotretinoin and its metabolites.
Because in vivo isotretinoin and tretinoin (fully transretinoic acid) are reversibly converted to each other, the metabolism of tretinoin is related to that of isotretinoin. 20-30% of the dose of isotretinoin is metabolized by isomerization.
In human isotretinoin pharmacokinetics, enterohepatic circulation may play a significant role.
In vitro metabolism studies have shown that several cytochrome P450 (CYP) enzymes are involved in the conversion of isotretinoin to 4-oxo isotretinoin and tretinoin. None of the isoforms appears to play a dominant role. Roaccutane® and its metabolites have no significant effect on CYP enzyme activity.
After oral administration of radioactively labeled isotretinoin, approximately equal amounts are detected in the urine and feces. The terminal phase elimination half-life for the unchanged drug in acne patients averages 19 hours. The terminal phase half-life for 4-oxo-isotretinoin appears to be longer, averaging 29 hours.
Isotretinoin refers to natural (physiological) retinoids. Endogenous retinoid concentrations are restored approximately 2 weeks after stopping Roaccutane®.
Pharmacokinetics in special clinical cases
Because isotretinoin is contraindicated in patients with hepatic impairment, there are limited data on the pharmacokinetics of the drug in this group of patients.
Indications
Indications
Acne that does not respond to other types of therapy. Severe forms of acne (nodulocystic, conglobate acne or acne with risk of scarring).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Acne treatment agent
ATX code [D10BA01]
Pharmacological action
Retinoid for systemic treatment of acne
Isotretinoin is a stereoisomer of all-trans retinoic acid (tretinoin).
The exact mechanism of action of the drug Roaccutane® has not yet been clarified, but it has been established that the improvement in the clinical picture of severe forms of acne is associated with suppression of the activity of the sebaceous glands and a histologically confirmed decrease in their size. In addition, isotretinoin has been shown to have anti-inflammatory effects on the skin.
Hyperkeratosis of epithelial cells of the hair follicle and sebaceous gland leads to desquamation of corneocytes into the gland duct and to blockage of the latter with keratin and excess sebaceous secretion. This is followed by the formation of a comedone and, in some cases, the addition of an inflammatory process.
Roaccutane® suppresses the proliferation of sebocytes and acts on acne, restoring the normal process of cell differentiation. Sebum is the main substrate for the growth of Propionibacterium acnes, so reducing sebum production inhibits bacterial colonization of the duct.
Pharmacokinetics
Since the kinetics of isotretinoin and its metabolites is linear, its plasma concentrations during therapy can be predicted based on data obtained after a single dose. This property of the drug also suggests that it does not affect the activity of liver enzymes involved in the metabolism of drugs.
Suction
Absorption of isotretinoin from the gastrointestinal tract varies. The absolute bioavailability of isotretinoin was not determined, since there is no release form of the drug for intravenous use in humans. However, extrapolation of data obtained in an experiment in dogs suggests a rather low and variable systemic bioavailability.
In patients with acne, maximum plasma concentrations (Cmax) at steady state after taking 80 mg of isotretinoin on an empty stomach were 310 ng/ml (range 188-473 ng/ml) and were achieved after 2-4 hours. Plasma concentrations of isotretinoin are approximately 1.7 times higher than blood concentrations due to poor penetration of isotretinoin into red blood cells.
Taking isotretinoin with food increases bioavailability by 2 times compared to taking it on an empty stomach.
Distribution
Isotretinoin is highly (99.9%) bound to plasma proteins, mainly albumin, so that over a wide range of therapeutic concentrations, the free (pharmacologically active) fraction of the drug is less than 0.1% of its total amount.
The volume of distribution of isotretinoin in humans has not been determined because there is no dosage form available for intravenous administration.
Equilibrium concentrations of isotretinoin in the blood (Cmin ss) in patients with severe acne who took 40 mg of the drug 2 times a day ranged from 120 to 200 ng/ml.
The concentrations of 4-oxo-isotretinoin in these patients were 2.5 times higher than those of isotretinoin. There is insufficient data on the penetration of isotretinoin into tissues in humans. Concentrations of isotretinoin in the epidermis are two times lower than in serum.
Metabolism
After oral administration, three main metabolites are found in plasma: 4-oxo-isotretinoin, tretinoin (all-trans retinoic acid) and 4-oxo-retinoin. The main metabolite is 4-oxo-isotretinoin, whose plasma concentrations at steady state are 2.5 times higher than the concentrations of the parent drug. Less significant metabolites have also been discovered, including glucuronides, but the structure of not all metabolites has been established.
Isotretinoin metabolites have biological activity confirmed in several laboratory tests. Thus, the clinical effects of the drug in patients may be the result of the pharmacological activity of isotretinoin and its metabolites.
Because isotretinoin and tretinoin (all-transretinoic acid) are reversibly converted into each other in vivo, the metabolism of tretinoin is related to the metabolism of isotretinoin. 20-30% of the isotretinoin dose is metabolized by isomerization.
Enterohepatic circulation may play a significant role in the pharmacokinetics of isotretinoin in humans.
In vitro metabolic studies have shown that several cytochrome P450 (CYP) enzymes are involved in the conversion of isotretinoin to 4-oxo-isotretinoin and tretinoin. Apparently, none of the isoforms plays a dominant role. Roaccutane® and its metabolites do not have a significant effect on the activity of enzymes of the CYP system.
Removal
After oral administration of radiolabeled isotretinoin, approximately equal amounts are found in urine and feces. The terminal phase half-life for unchanged drug in patients with acne averages 19 hours. The terminal phase half-life for 4-oxo-isotretinoin appears to be longer, averaging 29 hours.
Isotretinoin is a natural (physiological) retinoid. Endogenous concentrations of retinoids are restored approximately 2 weeks after the end of taking Roaccutane®.
Pharmacokinetics in special clinical situations
Since isotretinoin is contraindicated in patients with impaired liver function, data on the pharmacokinetics of the drug in this group of patients are limited.
Renal failure does not affect the pharmacokinetics of isotretinoin.
Special instructions
Special instructions
Roaccutane should only be prescribed by physicians, preferably dermatologists, who are experienced in the use of systemic retinoids and are aware of the drug’s teratogenicity risk. Both female and male patients should be given a copy of the Patient Information Leaflet.
To avoid accidental exposure of the drug to the body of other people, donated blood should not be taken from patients who are receiving or have recently (1 month) received Roaccutane.
It is recommended to monitor liver function and liver enzymes before treatment, 1 month after treatment, and then every 3 months or as indicated. A transient and reversible increase in liver transaminases was noted, in most cases within normal values. If the level of liver transaminases exceeds the norm, it is necessary to reduce the dose of the drug or discontinue it.
Fasting serum lipid levels should also be determined before treatment, 1 month after initiation, and then every 3 months or as indicated. Typically, lipid concentrations normalize after dose reduction or discontinuation of the drug, as well as with diet. It is necessary to monitor a clinically significant increase in triglyceride levels, since their rise above 800 mg/dL or 9 mmol/L can be accompanied by the development of acute pancreatitis, possibly fatal. In case of persistent hypertriglyceridemia or symptoms of pancreatitis, Roaccutane should be discontinued.
In rare cases, depression, psychotic symptoms, and very rarely, suicide attempts have been described in patients treated with Roaccutane. Although their causal relationship with the use of the drug has not been established, special caution should be exercised in patients with a history of depression and all patients should be monitored for the occurrence of depression during treatment with the drug, if necessary, referring them to an appropriate specialist. However, discontinuation of Roaccutane may not lead to the disappearance of symptoms and further observation and treatment by a specialist may be required.
In rare cases, at the beginning of therapy, an exacerbation of acne is observed, which resolves within 7-10 days without adjusting the dose of the drug.
Several years after the use of Roaccutane for the treatment of dyskeratosis, at a total course dose and duration of therapy higher than those recommended for the treatment of acne, bone changes developed, including premature closure of the epiphyseal growth plates, hyperostosis, calcification of ligaments and tendons. Therefore, when prescribing the drug to any patient, the ratio of possible benefits and risks should first be carefully assessed.
Patients receiving Roaccutane are recommended to use moisturizing ointment or body cream, lip balm to reduce dry skin and mucous membranes at the beginning of therapy.
During post-marketing surveillance with the use of the drug Roaccutane, cases of severe skin reactions, such as erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis, have been described. These events can be serious and can lead to disability, life-threatening conditions, hospitalization or death. Patients receiving Roaccutane require careful monitoring to identify severe skin reactions and, if necessary, consider discontinuing the drug.
While taking Roaccutane, pain in muscles and joints and an increase in serum creatinine phosphokinase are possible, which may be accompanied by a decrease in tolerance to intense physical activity.
Deep chemical dermoabrasion and laser treatment should be avoided in patients receiving Roaccutane, as well as for 5-6 months after the end of treatment due to the possibility of increased scarring in atypical places and the occurrence of hyper- and hypopigmentation. During treatment with Roaccutane and for 6 months after it, hair removal using wax applications cannot be performed due to the risk of epidermal detachment, scar development and dermatitis.
Since some patients may experience a decrease in night vision acuity, which sometimes persists even after the end of therapy, patients should be informed about the possibility of this condition, advising them to exercise caution when driving at night. Visual acuity must be carefully monitored.
Dryness of the conjunctiva of the eyes, corneal opacities, deterioration of night vision and keratitis usually disappear after discontinuation of the drug. If the mucous membrane of the eyes is dry, you can use applications of a moisturizing eye ointment or an artificial tear preparation. Patients with dry conjunctiva should be monitored for possible development of keratitis. Patients with vision complaints should be referred to an ophthalmologist and consider the advisability of discontinuing Roaccutane. If you are intolerant to contact lenses, you should use glasses during therapy.
Exposure to sunlight and UV rays should be limited. If necessary, use sunscreen with a high protection factor of at least 15 SPF.
Rare cases of the development of benign intracranial hypertension (“pseudotumor cerebri”) have been described, incl. when used in combination with tetracyclines. In such patients, Roaccutane should be discontinued immediately.
During therapy with Roaccutane, inflammatory bowel disease may occur. In patients with severe hemorrhagic diarrhea, Roaccutane should be immediately discontinued.
Rare cases of anaphylactic reactions that occurred only after previous external use of retinoids have been described. Severe allergic reactions dictate the need to discontinue the drug and carefully monitor the patient.
Patients at high risk (with diabetes, obesity, chronic alcoholism or lipid metabolism disorders) may require more frequent laboratory monitoring of glucose and lipid levels when treated with Roaccutane.
If diabetes is present or suspected, more frequent monitoring of glycemia is recommended.
Active ingredient
Active ingredient
Isotretinoin
Composition
Composition
One 10 mg capsule contains:
active substance:
isotretinoin – 10 mg;
excipients:
soybean oil – 107.92 mg,
yellow beeswax – 7.68 mg,
soybean oil hydrogenated – 7.68 mg,
soybean oil, partially hydrogenated – 30.72 mg;
capsule shell: glycerol 85% – 31.275 mg, gelatin – 75.64 mg, Karion 83 (hydrolyzed potato starch, mannitol, sorbitol) – 8.065 mg, red iron oxide dye (E172) – 0.185 mg, titanium dioxide (E171) – 1.185 mg;
ink for writing on the capsule: shellac, black iron oxide dye (E172); Ready-made ink Opacode Black S-1-27794 can be used.
Pregnancy
Pregnancy
Isotretinoin is a drug with a strong teratogenic effect. If pregnancy occurs while a woman is taking isotretinoin orally (at any dose and even for a short time), there is a very high risk of giving birth to a child with developmental defects.
Roaccutane® is contraindicated in women of childbearing age unless the woman’s condition meets all of the following criteria:
– she must have severe acne that is resistant to conventional treatments;
– she must accurately understand and follow the doctor’s instructions;
– she must be informed by the doctor about the danger of pregnancy during treatment with the drug
Roaccutane® within one month after it and urgent consultation if pregnancy is suspected:
– she must be warned about the possible ineffectiveness of contraceptives;
– she must confirm that she understands the essence of the precautionary measures;
– she must understand the need and continuously use effective methods of contraception for one month before treatment with Roaccutane®, during treatment and for a month after its completion (see section “Interaction with other drugs”); it is advisable to use 2 different methods of contraception at the same time, including barrier;
– she must have received a negative result from a reliable pregnancy test within 11 days before starting the drug; A pregnancy test is strongly recommended monthly during treatment and 5 weeks after the end of therapy;
– she should begin treatment with Roaccutane® only on the 2-3 day of the next normal menstrual cycle;
– she must understand the need for mandatory visits to the doctor every month;
– when being treated for a relapse of the disease, she must constantly use the same effective methods of contraception for one month before starting treatment with Roaccutane®, during treatment and for a month after its completion, as well as undergo the same reliable pregnancy test;
– she must fully understand the need for precautions and confirm her understanding and desire to use reliable methods of contraception, which were explained to her by the doctor.
Use of contraception as directed above during treatment with isotretinoin should be recommended even in women who do not routinely use contraception due to infertility (except in patients who have had a hysterectomy), amenorrhea, or who report not being sexually active.
The doctor must be sure that:
– the patient has a severe form of acne (nodulocystic, conglobate acne or acne with a risk of scarring); acne that does not respond to other types of therapy;
– a negative result from a reliable pregnancy test was obtained before starting the drug, during therapy and 5 weeks after the end of therapy; the dates and results of the pregnancy test must be documented;
– the patient uses at least 1, preferably 2 effective methods of contraception, including a barrier method, for one month before starting treatment with Roaccutane®, during treatment and for a month after its completion;
– the patient is able to understand and fulfill all of the above requirements for pregnancy protection;
– the patient meets all of the above conditions.
Pregnancy test
According to current practice, a pregnancy test with a minimum sensitivity of 25 mIU/ml should be performed in the first 3 days of the menstrual cycle:
Before starting therapy:
To rule out possible pregnancy, the result and date of the initial pregnancy test must be recorded by a doctor before starting contraception. In patients with irregular menstruation, the timing of a pregnancy test depends on sexual activity and should be performed 3 weeks after unprotected intercourse. The doctor should inform the patient about contraceptive methods.
A pregnancy test is carried out on the day of prescription of the drug Roaccutane® or 3 days before the patient’s visit to the doctor. The specialist should record the test results. The drug can only be prescribed to patients receiving effective contraception for at least 1 month before starting therapy with Roaccutane®.
During therapy:
The patient must visit the doctor every 28 days. The need for monthly pregnancy testing is determined in accordance with local practice and taking into account sexual activity and previous menstrual irregularities. If indicated, a pregnancy test is performed on the day of the visit or three days before the visit to the doctor, the test results must be recorded.
End of therapy:
5 weeks after the end of therapy, a test is performed to exclude pregnancy.
A prescription for Roaccutane® for a woman capable of childbearing can be issued only for 30 days of treatment; continuation of therapy requires a new prescription of the drug by a doctor. It is recommended to take a pregnancy test, write a prescription and receive the drug on the same day.
The drug Roaccutane® should be dispensed at the pharmacy only within 7 days from the date of issuing the prescription.
Full information about teratogenic risk and strict adherence to measures to prevent pregnancy should be provided to both men and women. For male patients
Existing data suggest that in women, exposure to the drug from the semen and seminal fluid of men taking Roaccutane® is not sufficient to cause the teratogenic effects of Roaccutane®.
Men should exclude the possibility of other persons, especially women, taking the drug.
If, despite the precautions taken, pregnancy does occur during treatment with Roaccutane® or within a month after its end, there is a high risk of very severe fetal malformations (in particular, from the central nervous system, heart and large blood vessels). In addition, the risk of spontaneous miscarriages increases.
If pregnancy occurs, therapy with Roaccutane® is discontinued. The advisability of maintaining it should be discussed with a doctor specializing in teratology.
Severe congenital malformations of the fetus in humans associated with the use of Roaccutane® have been documented, including hydrocephalus, microcephaly, cerebellar malformations, anomalies of the external ear (microtia, narrowing or absence of the external auditory canal), microphthalmia, cardiovascular anomalies (tetralogy of Fallot, transposition of the great vessels, septal defects), malformations of the face (cleft palate), thymus gland, pathology of the parathyroid glands.
Because isotretinoin is highly lipophilic, it is very likely that it passes into breast milk. Due to possible side effects, Roaccutane® should not be prescribed to nursing mothers.
Contraindications
Contraindications
Pregnancy, breastfeeding, liver failure, hypervitaminosis A, severe hyperlipidemia, concomitant therapy with tetracyclines.
Hypersensitivity to the drug or its components.
Children’s age up to 12 years.
Side Effects
Side Effects
Most of the side effects of Roaccutane are dose dependent. As a rule, when prescribing the recommended doses, the benefit-risk ratio, taking into account the severity of the disease, is acceptable for the patient. Side effects are usually reversible after dose adjustment or drug discontinuation, but some may persist after treatment is stopped.
Symptoms associated with hypervitaminosis A: dry skin, mucous membranes, incl. lips (cheilitis), nasal cavity (bleeding), hypopharynx (hoarseness), eyes (conjunctivitis, reversible corneal opacity and contact lens intolerance).
Skin and its appendages: rash, itching, facial erythema/dermatitis, sweating, pyogenic granuloma, paronychia, onychodystrophy, increased proliferation of granulation tissue, persistent thinning of hair, reversible hair loss, fulminant forms of acne, hirsutism, hyperpigmentation, photosensitivity, photoallergy, easy skin trauma. At the beginning of treatment, acne may worsen and persist for several weeks.
Musculoskeletal system: muscle pain with or without increased serum CPK levels, joint pain, hyperostosis, arthritis, calcification of ligaments and tendons, other bone changes, tendinitis.
Central nervous system and mental sphere: behavioral disturbances, depression, headache, increased intracranial pressure (“pseudotumor cerebri”: headache, nausea, vomiting, blurred vision, papilledema), seizures.
Sense organs: isolated cases of impaired visual acuity, photophobia, impaired dark adaptation (reduced twilight visual acuity), rarely – impaired color vision (passing after discontinuation of the drug), lenticular cataract, keratitis, blepharitis, conjunctivitis, eye irritation, papilledema (as a manifestation of intracranial hypertension); hearing loss at certain sound frequencies.
Gastrointestinal tract: nausea, diarrhea, inflammatory bowel diseases (colitis, ileitis), bleeding; pancreatitis (especially with concomitant hypertriglyceridemia above 800 mg/dl). Rare cases of pancreatitis with a fatal outcome have been described.
Transient and reversible increase in the activity of liver transaminases, isolated cases of hepatitis. In many of these cases, the changes did not go beyond the normal range and returned to initial values during treatment, however, in some situations there was a need to reduce the dose or discontinue Roaccutane.
Respiratory organs: rarely – bronchospasm (more often in patients with a history of bronchial asthma).
Blood system: anemia, decreased hematocrit, leukopenia, neutropenia, increased or decreased platelet count, accelerated ESR.
Laboratory indicators: hypertriglyceridemia, hypercholesterolemia, hyperuricemia, decreased levels of high-density lipoproteins, rarely – hyperglycemia. Cases of newly diagnosed diabetes mellitus have been reported while taking Roaccutane. In some patients, especially those involved in intense physical activity, isolated cases of increased CK activity in the serum have been described.
Immune system: local or systemic infections caused by gram-positive pathogens (Staphylococcus aureus).
Other: lymphadenopathy, hematuria, proteinuria, vasculitis (Wegener’s granulomatosis, allergic vasculitis), systemic hypersensitivity reactions, glomerulonephritis.
Interaction
Interaction
Due to a possible increase in the symptoms of hypervitaminosis A, the simultaneous administration of Roaccutane and vitamin A should be avoided.
Since tetracyclines can also cause increased intracranial pressure, their use in combination with Roaccutane is contraindicated.
Isotretinoin may reduce the effectiveness of progesterone preparations, so contraceptives containing low doses of progesterone should not be used.
Combined use with topical keratolytic or exfoliative drugs for the treatment of acne is contraindicated due to the possible increase in local irritation.
Overdose
Overdose
In case of overdose, signs of hypervitaminosis A may appear.
In the first few hours after an overdose, gastric lavage may be necessary.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C, protected from light and moisture. Keep out of the reach of children.
Shelf life
Shelf life
3 years.
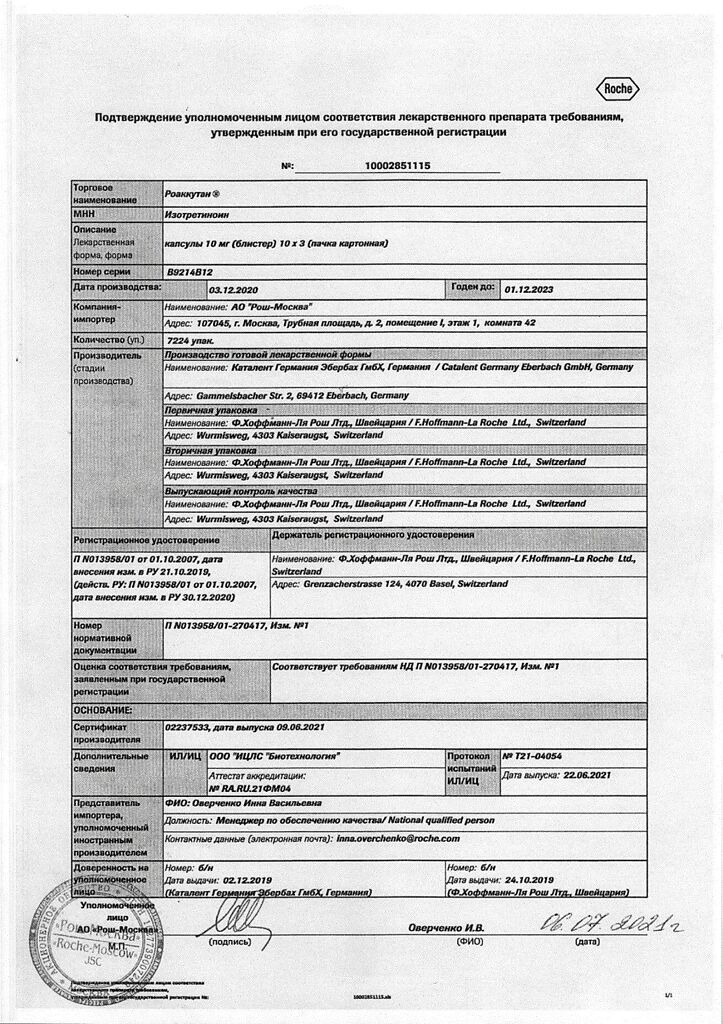
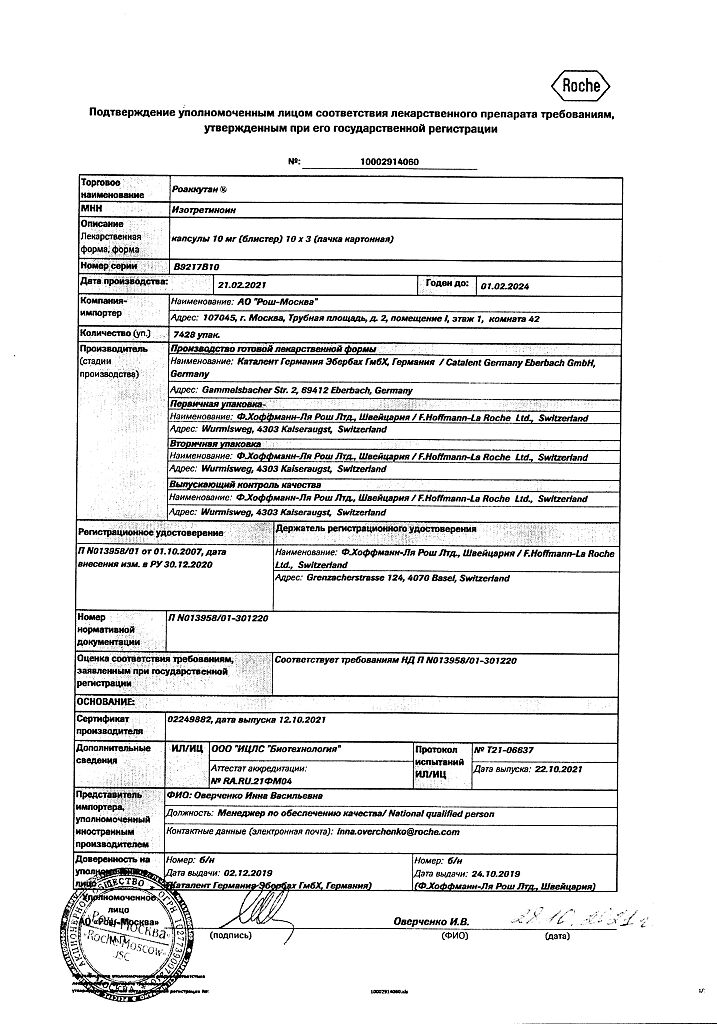
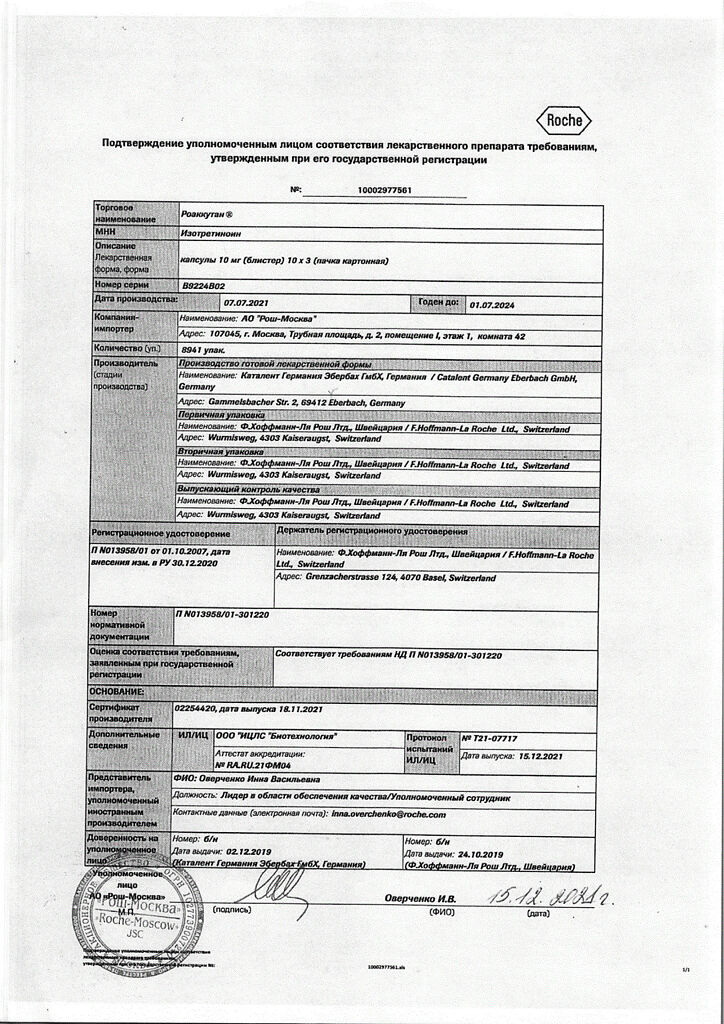
Manufacturer
Manufacturer
Catalent Germany Eberbach GmbH, Germany
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store at temperatures under 25 ° C, protected from light and moisture.Keep out of reach of children. |
| Manufacturer | Catalent Germany Eberbach GmbH, Germany |
| Medication form | capsules |
| Brand | Catalent Germany Eberbach GmbH |
Other forms…
Related products
Buy Roaccutane, 10 mg capsules 30 pcs with delivery to USA, UK, Europe and over 120 other countries.