No products in the cart.
Reduxin Forte, 850 mg+15 mg 90 pcs
€237.79 €216.09
Description
Pharmacotherapeutic group
Hypoglycemic agent of oral biguanide group. An agent for the treatment of obesity.
ATX code: A08A and A10BA02
Pharmacodynamics
Metformin
. An oral hypoglycemic drug of the biguanide group, reduces hyperglycemia without resulting in hypoglycemia. Unlike sulfonylurea derivatives, it does not stimulate insulin secretion and does not cause hypoglycemic effect in healthy people. Increases the sensitivity of peripheral receptors to insulin and glucose utilization by cells. Inhibits gluconeogenesis in the liver. Delays absorption of carbohydrates in the intestine and stimulates the production of GTP-1 (physiological regulator of appetite).
Metformin stimulates glycogen synthesis by acting on glycogen synthase. It increases transport capacity of all types of membrane glucose transporters. In addition, it has a favorable effect on lipid metabolism: it decreases concentrations of total cholesterol, low-density lipoproteins and triglycerides.
During metformin administration body weight remains stable or decreases moderately.
Sibutramine
It is a prodrug and shows its effect in vivo due to metabolites (primary and secondary amines) that inhibit monoamine reuptake (serotonin, noradrenaline and dopamine). The increase of neurotransmitters in synapses increases the activity of central 5NT-serotonin and adrenergic receptors and contributes to the physiological regulation of appetite by increasing the feeling of satiety and reducing the need for food, as well as increasing thermoproduction (internal energy expenditure). By activating β-adrenoceptors indirectly, sibutramine affects brown adipose tissue. Reduction of body weight when taking sibutramine is accompanied by an increase in serum concentration of high density lipoproteins (HDL) and a decrease in triglycerides, total cholesterol, low density lipoproteins (LDL) and uric acid.
Sibutramine and its metabolites do not affect the release of monoamines, do not inhibit monoamine oxidase (MAO); They have no affinity to a large number of neurotransmitter receptors, including serotonin receptors (5-HT1, 5-HT1A, 5-HT1B, 5-HT2C), adrenergic (β1, β2, β3, α1, α2), dopamine (D1, D2), muscarinic, histamine (H1), benzodiazepine and glutamate NMDA receptors.
Simultaneous use of metformin and sibutramine increases the effectiveness of therapy in obese patients. By regulating appetite, reducing hunger, increasing energy expenditure and regulating lipid and carbohydrate metabolism, Reduxin® Forte reduces human body weight and restores metabolic health.
Clinical efficacy and safety (Results of clinical studies)
In a clinical study in Reduxin® Forte group the percentage of patients who achieved clinically significant weight loss ≥5% during 3 months of therapy (early response rate to therapy) exceeded 90%. During 6 months of therapy 91.67% of patients in the Reduxin® Forte group achieved a weight loss of 10% or more. The decrease of body weight was accompanied by clinically significant reduction of waist circumference and improvement of lipid profile, which proves the effectiveness of the drug in reducing the risk of complications and meets the main objectives of treatment of obesity.
No negative effect of Reduxin® Forte on the cardiovascular system parameters was observed during the study in patients with obesity.
Pharmacokinetics
absorption
After oral administration metformin is completely absorbed from the GI tract. With concomitant food intake, metformin absorption is reduced and delayed. Absolute bioavailability is 50-60%. Maximum plasma concentration (Cmax) is approximately 2 µg/ml or 15 µmol and is reached after 2.5 hours.
Distribution
Metformin is rapidly distributed in body tissues. Virtually not bound to plasma proteins.
Metabolism
Subject to little metabolism.
Elimation
It is excreted by the kidneys. Metformin clearance in healthy subjects is 400 mL/min (4 times higher than creatinine clearance (CK)), indicating active tubular secretion.
The half-life (T1/2) is approximately 6.5 h.
Pharmacokinetics in special clinical cases
In patients with renal insufficiency T1/2 is increased, there is a risk of metformin cumulation in the body.
Sibutramine
absorption
After oral administration, it is rapidly absorbed from the GI tract by at least 77 %. During “primary passage” through the liver, it undergoes biotransformation under the influence of CYP3A4 isoenzyme to form two active metabolites (monodesmethylsibutramine (M1) and didesmethylsibutramine (M2)). After a single dose of 15 mg, maximum blood concentration (Cmax) of monodesmethylsibutramine (M1) is 4 ng/ml (3.2-4.8 ng/ml), didesmethylsibutramine (M2) – 6.4 ng/ml (5.6-7.2 ng/ml). Cmax is reached in 1.2 h (sibutramine), 3-4 h (active metabolites). Simultaneous intake of food decreases Cmax of metabolites by 30% and increases the time to reach it by 3 hours without changing the area under the curve “concentration-time” (AUC).
Distribution
Rapidly distributed in tissues. Protein binding is 97% (sibutramine) and 94% (M1 and M2). Equilibrium concentration of active metabolites in blood is reached within 4 days after the start of treatment and is approximately 2 times higher than the concentration in plasma after a single dose.
Metabolism and excretion
Active metabolites undergo hydroxylation and conjugation with the formation of inactive metabolites, which are excreted mainly by the kidneys. The half-life of sibutramine is 1.1 h, M1 – 14 h, M2 – 16 h.
Pharmacokinetics in special clinical cases
The currently available data do not indicate the existence of clinically significant differences in pharmacokinetics in men and women.
Pharmacokinetics in the elderly
Pharmacokinetics in elderly healthy individuals (mean age 70 years) is similar to that in young adults.
Renal failure
Renal failure has no effect on the AUC of active metabolites M1 and M2, except for metabolite M2 in patients with end-stage renal failure on dialysis.
Hepatic failure
Patients with moderate hepatic failure after a single dose of sibutramine have a 24% higher AUC of active M1 and M2 metabolites than in healthy subjects.
Indications
Indications
The drug Reduxin® Forte is indicated for correcting body weight and improving lipid and carbohydrate metabolism in patients:
with a body mass index (BMI) of more than 30 kg/m2 (nutritional obesity);
with a BMI of 27 kg/m2 or more in combination with type 2 diabetes mellitus and dyslipidemia;
with a BMI of 30 kg/m2 or more with prediabetes and additional risk factors for developing type 2 diabetes mellitus, in whom lifestyle changes did not allow achieving adequate glycemic control.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Hypoglycemic agent of the biguanide group for oral use. Drug for the treatment of obesity.
ATX code: A08A and A10BA02
Pharmacodynamics
Metformin
An oral hypoglycemic drug from the biguanide group, reduces hyperglycemia without leading to the development of hypoglycemia. Unlike sulfonylurea derivatives, it does not stimulate insulin secretion and does not cause a hypoglycemic effect in healthy people. Increases the sensitivity of peripheral receptors to insulin and the utilization of glucose by cells. Inhibits gluconeogenesis in the liver. Delays the absorption of carbohydrates in the intestine and stimulates the production of GLP-1 (a physiological regulator of appetite).
Metformin stimulates glycogen synthesis by acting on glycogen synthase. Increases the transport capacity of all types of membrane glucose transporters. In addition, it has a beneficial effect on lipid metabolism: it reduces the concentration of total cholesterol, low-density lipoproteins and triglycerides.
While taking metformin, the patient’s body weight either remains stable or decreases moderately.
Sibutramine
It is a prodrug and exhibits its effect in vivo due to metabolites (primary and secondary amines) that inhibit the reuptake of monoamines (serotonin, norepinephrine and dopamine). An increase in the content of neurotransmitters in synapses increases the activity of central 5HT-serotonin and adrenergic receptors, promotes the physiological regulation of appetite by increasing the feeling of satiety and reducing the need for food, as well as increasing thermal production (internal energy expenditure). By indirectly activating β3-adrenergic receptors, sibutramine acts on brown adipose tissue. Weight loss when taking sibutramine is accompanied by an increase in serum concentrations of high-density lipoproteins (HDL) and a decrease in the concentrations of triglycerides, total cholesterol, low-density lipoproteins (LDL) and uric acid.
Sibutramine and its metabolites do not affect the release of monoamines and do not inhibit monoamine oxidase (MAO); do not have affinity for a large number of neurotransmitter receptors, including serotonin (5-HT1, 5-HT1A, 5-HT1B, 5-HT2C), adrenergic (β1, β2, β3, α1, α2), dopamine (D1, D2), muscarinic, histamine (H1), benzodiazepine and glutamate NMDA receptors.
The simultaneous use of metformin and sibutramine increases the effectiveness of therapy in obese patients. By regulating appetite, reducing hunger, increasing energy expenditure and regulating lipid and carbohydrate metabolism, Reduxin®Forte reduces human body weight and restores metabolic health.
Clinical efficacy and safety (Clinical trial results)
In a clinical study in the Reduxin® Forte group, the proportion of patients who achieved clinically significant weight loss ≥5% after 3 months of therapy (the proportion of early responders to therapy) exceeded 90%. Over 6 months of therapy, 91.67% of patients in the Reduxin® Forte group achieved a reduction in body weight of 10% or more. The decrease in body weight was accompanied by a clinically significant decrease in waist circumference and an improvement in the lipid profile, which proves the effectiveness of the drug in reducing the risk of complications and meets the main goals of obesity therapy.
During the study, there was no negative effect of the drug Reduxin® Forte on the parameters of the cardiovascular system when used in obese patients.
Pharmacokinetics
Suction
After taking the drug orally, metformin is quite completely absorbed from the gastrointestinal tract. With simultaneous food intake, the absorption of metformin is reduced and delayed. Absolute bioavailability is 50-60%. The maximum plasma concentration (Cmax) is approximately 2 µg/ml or 15 µmol and is achieved after 2.5 hours.
Distribution
Metformin is quickly distributed in body tissues. Practically does not bind to plasma proteins.
Metabolism
Metabolized to a small extent.
Removal
Excreted by the kidneys. Metformin clearance in healthy people is 400 ml/min (4 times higher than creatinine clearance (CC)), indicating active tubular secretion.
The half-life (T1/2) is approximately 6.5 hours.
Pharmacokinetics in special clinical situations
In patients with renal failure, T1/2 increases, and there is a risk of metformin accumulation in the body.
Sibutramine
Suction
After oral administration, it is quickly absorbed from the gastrointestinal tract by at least 77%. During the “primary passage” through the liver, it undergoes biotransformation under the influence of the CYP3A4 isoenzyme with the formation of two active metabolites (monodesmethylsibutramine (M1) and didesmethylsibutramine (M2)). After taking a single dose of 15 mg, the maximum blood concentration (Cmax) of monodesmethylsibutramine (M1) is 4 ng/ml (3.2-4.8 ng/ml), didesmethylsibutramine (M2) – 6.4 ng/ml (5.6-7.2 ng/ml). Cmax is reached after 1.2 hours (sibutramine), 3-4 hours (active metabolites). Simultaneous food intake reduces the Cmax of metabolites by 30% and increases the time to reach it by 3 hours, without changing the area under the concentration-time curve (AUC).
Distribution
Quickly distributed in tissues. Protein binding is 97% (sibutramine) and 94% (M1 and M2). The equilibrium concentration of active metabolites in the blood is achieved within 4 days after the start of treatment and is approximately 2 times higher than the concentration in the blood plasma after taking a single dose.
Metabolism and excretion
Active metabolites undergo hydroxylation and conjugation to form inactive metabolites, which are excreted primarily by the kidneys. The half-life of sibutramine is 1.1 hours, M1 – 14 hours, M2 – 16 hours.
Pharmacokinetics in special clinical situations
Currently available data do not indicate the existence of clinically significant differences in pharmacokinetics between men and women.
Pharmacokinetics in the elderly
Pharmacokinetics in elderly healthy people (average age 70 years) are similar to those in young people.
Kidney failure
Renal impairment does not affect the AUC of the active metabolites M1 and M2, except for the M2 metabolite in patients with end-stage renal disease on dialysis.
Liver failure
In patients with moderate hepatic impairment, after a single dose of sibutramine, the AUC of active metabolites M1 and M2 is 24% higher than in healthy people.
Special instructions
Special instructions
Lactic acidosis
Lactic acidosis is a rare but serious (high mortality unless promptly treated) complication that may occur due to accumulation of metformin. Cases of lactic acidosis when taking metformin occurred mainly in diabetic patients with severe renal failure.
Other associated risk factors should be taken into account, such as decompensated diabetes mellitus, ketosis, prolonged fasting, alcoholism, liver failure and any condition associated with severe hypoxia. This may help reduce the incidence of lactic acidosis.
The risk of developing lactic acidosis should be taken into account when nonspecific signs appear, such as muscle cramps accompanied by dyspeptic symptoms, abdominal pain and severe asthenia. Lactic acidosis is characterized by acidotic shortness of breath, abdominal pain and hypothermia followed by coma.
Diagnostic laboratory parameters are a decrease in blood pH (less than 7.25), lactate content in the blood plasma over 5 mmol/l, increased anion gap and lactate/pyruvate ratio. If metabolic acidosis is suspected, stop taking the drug and consult a doctor immediately.
Surgical operations
The use of Reduxin® Forte should be discontinued 48 hours before planned surgical operations and can be continued no earlier than 48 hours after, provided that during the examination, renal function was found to be normal.
Kidney function
Since metformin is excreted by the kidneys, before starting to take the drug Reduxin® Forte and regularly thereafter, it is necessary to determine CC: at least once a year in patients with normal renal function, and 2-4 times a year in elderly patients, as well as in patients with CC at the lower limit of normal.
Particular caution should be exercised in case of possible impairment of renal function in elderly patients, with simultaneous use of antihypertensive drugs, diuretics or non-steroidal anti-inflammatory drugs.
Patients are advised to continue to follow a diet with even carbohydrate intake throughout the day. Overweight patients are advised to continue to follow a hypocaloric diet (but not less than 1000 kcal/day).
It is recommended that routine laboratory tests be performed regularly to monitor diabetes mellitus.
It is recommended to exercise caution when using Reduxin® Forte in combination with insulin or other hypoglycemic agents (including sulfonylurea derivatives, repaglinide).
Treatment with Reduxin® Forte should be carried out as part of complex therapy for weight loss under the supervision of a physician with practical experience in the treatment of obesity. Complex therapy includes both changing diet and lifestyle, as well as increasing physical activity. An important component of therapy is to create the prerequisites for persistent changes in eating behavior and lifestyle, which are necessary to maintain the achieved weight loss even after drug therapy is discontinued. As part of therapy with Reduxin® Forte, patients need to change their lifestyle and habits in such a way as to ensure that the achieved weight loss is maintained after completion of treatment. Patients should be clear that failure to comply with these requirements will lead to repeated weight gain and repeated visits to their doctor.
In patients taking the drug Reduxin® Forte, it is necessary to measure blood pressure and heart rate. During the first 3 months of treatment, these parameters should be monitored every 2 weeks and then monthly. If during two consecutive visits an increase in resting heart rate ≥10 beats per minute or systolic/diastolic pressure ≥10 mmHg is detected. Art., it is necessary to stop treatment. In patients with arterial hypertension whose blood pressure is above 145/90 mm Hg during antihypertensive therapy. Art., this control should be carried out especially carefully and, if necessary, at shorter intervals. In patients whose blood pressure exceeded 145/90 mmHg twice during repeated measurements. Art., treatment with Reduxin® Forte should be suspended (see section “Side effects”, subsections “Heart disorders”, “Vascular disorders”).
In patients with sleep apnea, blood pressure must be monitored especially carefully.
The simultaneous administration of drugs that increase the QT interval requires special attention. These drugs include H1-histamine receptor blockers (astemizole, terfenadine); antiarrhythmic drugs that increase the QT interval (amiodarone, quinidine, flecainide, mexiletine, propafenone, sotalol); gastrointestinal motility stimulator cisapride; pimozide, sertindole and tricyclic antidepressants. This also applies to conditions that can lead to an increase in the QT interval, such as hypokalemia and hypomagnesemia (see section “Interaction with other drugs”).
The interval between taking MAO inhibitors (including furazolidone, procarbazine, selegiline) and Reduxin® Forte should be at least 2 weeks.
Although a connection has not been established between taking sibutramine and the development of primary pulmonary hypertension, however, given the well-known risk of drugs in this group, with regular medical monitoring it is necessary to pay special attention to symptoms such as progressive dyspnea (breathing difficulty), chest pain and swelling in the legs.
If you miss a dose of Reduxin® Forte, you should not take a double dose of the drug at the next dose; it is recommended to continue taking the drug according to the prescribed regimen.
When taking sibutramine and other serotonin reuptake inhibitors together, there is an increased risk of bleeding. In patients predisposed to bleeding or taking drugs that affect hemostasis or platelet function, sibutramine should be used with caution.
Although there is no clinical evidence of addiction to sibutramine, the patient’s history of drug dependence should be assessed and attention should be paid to possible signs of drug abuse.
Impact on the ability to drive vehicles and machinery
Taking the drug Reduxin® Forte may limit the ability to drive vehicles and machines. During the period of use of the drug Reduxin® Forte, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Metformin, Sibutramine
Composition
Composition
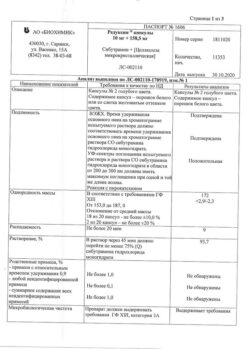
Each 850 mg + 10 mg tablet contains:
Active ingredients:
metformin hydrochloride – 850.0 mg; sibutramine hydrochloride monohydrate – 10.0 mg;
Excipients:
microcrystalline cellulose, croscarmellose sodium, povidone K-25, magnesium stearate;
Film coating excipients:
Ready-made system for coating Opadry II 85F30656 blue (polyvinyl alcohol, macrogol, titanium dioxide, talc, brilliant blue dye with aluminum varnish, indigo carmine dye with aluminum varnish, iron oxide yellow dye).
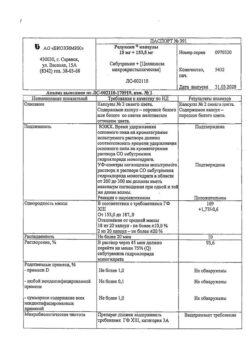
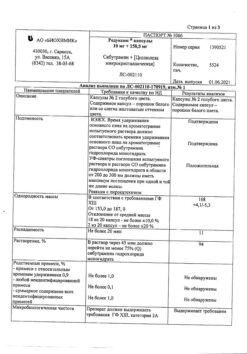
Each 850 mg + 15 mg tablet contains:
Active ingredients:
metformin hydrochloride – 850.0 mg; sibutramine hydrochloride monohydrate – 15.0 mg;
Excipients:
microcrystalline cellulose, croscarmellose sodium, povidone K-25, magnesium stearate;
Film coating excipients:
Ready-made coating system Opadry II 85F48105 white (polyvinyl alcohol, macrogol, talc, titanium dioxide).
Pregnancy
Pregnancy
Since to date there is not a sufficiently convincing amount of research regarding the safety of the effects of sibutramine on the fetus, this drug is contraindicated during pregnancy. Women of reproductive age should use contraceptives while taking Reduxin® Forte.
The use of Reduxin® Forte during breastfeeding is contraindicated.
Contraindications
Contraindications
hypersensitivity to the components of the drug;
diabetic ketoacidosis, diabetic precoma, diabetic coma;
impaired renal function (creatinine clearance (CC) less than 45 ml/min);
liver dysfunction;
acute conditions in which there is a risk of developing renal dysfunction: dehydration (with diarrhea, vomiting), severe infectious diseases, shock;
cardiovascular diseases (in history and currently): coronary heart disease (myocardial infarction (MI), angina pectoris), chronic heart failure in the stage of decompensation, occlusive diseases of peripheral arteries, tachycardia, arrhythmia, cerebrovascular diseases (stroke, transient cerebrovascular accidents);
uncontrolled arterial hypertension (blood pressure (BP) above 145/90 mm Hg) (see also section “Special instructions”);
clinically pronounced manifestations of acute and chronic diseases that can lead to the development of tissue hypoxia (including respiratory failure, heart failure, acute MI);
chronic alcoholism, acute ethanol poisoning;
thyrotoxicosis;
benign prostatic hyperplasia;
pheochromocytoma;
angle-closure glaucoma;
extensive surgical operations and injuries (when insulin therapy is indicated);
lactic acidosis (including history);
established pharmacological or drug dependence;
pregnancy and breastfeeding;
age under 18 and over 65 years;
a period of less than 48 hours before and within 48 hours after radioisotope or x-ray studies with the introduction of iodine-containing contrast agent;
following a hypocaloric diet (less than 1000 kcal/day);
the presence of organic causes of obesity (for example, hypothyroidism);
serious eating disorders – anorexia nervosa or bulimia nervosa;
mental illness;
Gilles de la Tourette syndrome (generalized tics);
simultaneous use of MAO inhibitors (for example, phentermine, fenfluramine, dexfenfluramine, ethylamphetamine, ephedrine) or their use within 2 weeks before taking sibutramine and 2 weeks after stopping it; other drugs acting on the central nervous system, inhibiting the reuptake of serotonin (for example, antidepressants, antipsychotics); sleeping pills containing tryptophan, as well as other centrally acting drugs for weight loss or the treatment of mental disorders.
With caution
The drug should be used in the following conditions: history of arrhythmias; chronic circulatory failure; diseases of the coronary arteries (including a history), except for coronary heart disease (MI, angina); glaucoma, except angle-closure glaucoma; cholelithiasis; arterial hypertension (controlled and with a history); neurological disorders, including mental retardation and seizures (including history); epilepsy; impaired renal function (creatinine clearance 45-59 ml/min); history of motor and verbal tics; tendency to bleed; blood clotting disorders; taking medications that affect hemostasis or platelet function; persons over 60 years of age who perform heavy physical work, which is associated with an increased risk of developing lactic acidosis.
Side Effects
Side Effects
Determination of the frequency of side effects: very often (1/10), often (1/100, <1/10), infrequently (1/1000, <1/100), rarely (1/10,000,
<1/1000), very rare (<1/10,000). Side effects are presented in order of decreasing importance.Metformin
Metabolic and nutritional disorders: very rarely – lactic acidosis; with long-term use, the absorption of vitamin B12 may be reduced. Decreased vitamin B12 concentrations should be taken into account in patients with megaloblastic anemia.
Nervous system disorders: often – taste disturbance.
Gastrointestinal disorders: very often – nausea, vomiting, diarrhea, abdominal pain, lack of appetite.
Most often, these symptoms occur during the initial period of treatment and in most cases disappear spontaneously. Slowly increasing the dose may improve gastrointestinal tolerability.
Disorders of the liver and biliary tract: very rarely – impaired liver function, hepatitis; after discontinuation of metformin, these undesirable effects completely disappear.
Skin and subcutaneous tissue disorders: very rarely – skin reactions such as erythema, itching, rash.
Sibutramine
Most often, side effects occur at the beginning of treatment (in the first 4 weeks). Their severity and frequency weaken over time. Side effects are generally mild and reversible.
Nervous system disorders: very often – dry mouth and insomnia, often – headache, dizziness, anxiety, paresthesia, as well as changes in taste.
Cardiac disorders: often – tachycardia, palpitations.
Vascular disorders: increased blood pressure, vasodilation. There is a moderate rise in blood pressure at rest by 1-3 mmHg. Art. and a moderate increase in heart rate of 3-7 beats per minute. In some cases, a more pronounced increase in blood pressure and an increase in heart rate cannot be ruled out. Clinically significant changes in blood pressure and pulse are recorded mainly at the beginning of treatment (in the first 4-8 weeks).
Gastrointestinal disorders: very often – loss of appetite and constipation, often – nausea and exacerbation of hemorrhoids. If you are prone to constipation in the first days, monitoring the evacuation function of the intestines is necessary. If constipation occurs, stop taking it and take a laxative.
Skin and subcutaneous tissue disorders: often – increased sweating.
In isolated cases, the following clinically significant adverse events have been described during treatment with sibutramine: dysmenorrhea, edema, flu-like syndrome, skin itching, back pain, abdominal pain, paradoxical increase in appetite, thirst, rhinitis, depression, drowsiness, emotional lability, anxiety, irritability, nervousness, acute interstitial nephritis, bleeding, Henoch-Schönlein purpura (hemorrhages into the skin), convulsions, thrombocytopenia, transient increase in the activity of “liver” enzymes in the blood.
Use of the drug Reduxin® Forte in patients with high blood pressure: see sections “Contraindications” and “Special instructions”.
During post-marketing studies of sibutramine, additional adverse reactions were described as follows by organ system:
Immune system disorders: hypersensitivity reactions (from mild skin rashes and urticaria to angioedema (Quincke’s edema) and anaphylaxis).
Mental disorders: psychosis, states of suicidal ideation, suicide and mania. If such
occurs
conditions, the drug must be discontinued.
Nervous system disorders: seizures, short-term memory impairment.
Visual disturbances: blurred vision (“blurs before the eyes”). Cardiac disorders: atrial fibrillation.
Gastrointestinal disorders: diarrhea, vomiting.
Skin and subcutaneous tissue disorders: alopecia.
Renal and urinary tract disorders: urinary retention.
Genital and breast disorders: ejaculation/orgasm disorders, impotence, menstrual irregularities, uterine bleeding.
Interaction
Interaction
Metformin
Contraindicated combinations
Iodine-containing X-ray contrast agents: against the background of functional renal failure in patients with diabetes, radiological examination using iodine-containing X-ray contrast agents can cause the development of lactic acidosis. Treatment with metformin should be discontinued depending on renal function 48 hours before or during an X-ray examination using iodinated contrast agents and not resumed earlier than 48 hours after the examination, provided that during the examination renal function was found to be normal.
Combinations not recommended
Alcohol: with acute alcohol intoxication, the risk of developing lactic acidosis increases, especially in cases of:
malnutrition, low-calorie diet;
liver failure.
While taking the drug, you should avoid drinking alcohol and medications containing ethanol.
Combinations requiring caution
Danazol: simultaneous use of danazol is not recommended to avoid the hyperglycemic effect of the latter. If treatment with danazol is necessary and after discontinuation of the latter, a dose adjustment of metformin is required under the control of blood glucose concentrations.
Chlorpromazine: When taken in large doses (100 mg per day), it increases blood glucose concentrations, reducing insulin release. When treated with antipsychotics and after stopping the latter, dose adjustment of the drug is required under the control of blood glucose concentrations.
Glucocorticosteroids (GCS) of systemic and local action reduce glucose tolerance, increase the concentration of glucose in the blood, sometimes causing ketosis. When treating GCS and after stopping the latter, dose adjustment of metformin is required under the control of blood glucose concentrations.
Diuretics: Concomitant use of loop diuretics may lead to the development of lactic acidosis due to possible functional renal failure. Metformin should not be prescribed if CC is below 60 ml/min.
Prescribed by injection, beta2-adrenergic agonists: increase the concentration of glucose in the blood due to stimulation of beta2-adrenergic receptors. In this case, monitoring of blood glucose concentration is necessary. If necessary, insulin administration is recommended.
When using the above drugs simultaneously, more frequent monitoring of blood glucose concentrations may be required, especially at the beginning of treatment. If necessary, the dose of metformin can be adjusted during treatment and after its cessation.
Angiotensin-converting enzyme inhibitors and other antihypertensive drugs may decrease blood glucose concentrations. If necessary, the dose of metformin should be adjusted.
The hypoglycemic effect of metformin can be reduced by phenothiazides, glucagon, estrogens, oral contraceptives, phenytoin, sympathomimetics, nicotinic acid, isoniazid, blockers of “slow” calcium channels, sodium levothyroxine. Concomitant use with cimetidine reduces the rate of elimination of metformin, which can lead to the development of lactic acidosis. In healthy volunteers, with the simultaneous use of metformin and propranolol, as well as with the use of metformin and ibuprofen, no changes in their pharmacokinetic parameters were observed. Metformin may reduce the effect of indirect anticoagulants.
Organic cation transporter substrates 1 and 2 (OST1 AND OST2)
Metformin is a substrate of the organic cations OCT1 and OCT2. When used together with metformin:
OCT1 inhibitors (such as verapamil) may reduce the hypoglycemic effect of metformin.
OCT1 inducers (such as rifampicin) may increase the absorption of metformin in the gastrointestinal tract and enhance its hypoglycemic effect.
OCT2 inhibitors (such as cimetidine, dolutegravir, ranolazine, trimethoprim, vandetanib, isavuconazole) may reduce the renal excretion of metformin and lead to an increase in its plasma concentration.
OCT1 and OCT2 inhibitors (such as crizotinib, olaparide) may reduce the hypoglycemic effect of metformin.
When metformin is used simultaneously with sulfonylurea derivatives, insulin, acarbose, and salicylates, hypoglycemia may develop.
Nifedipine increases the absorption and Cmax of metformin.
Cationic drugs (amiloride, digoxin, morphine, procainamide, quinidine, quinine, ranitidine, triamterene, trimethoprim and vancomycin) secreted in the renal tubules compete with metformin for tubular transport systems and may lead to an increase in its Cmax.
Sibutramine
Inhibitors of microsomal oxidation, incl. inhibitors of the CYP3A4 isoenzyme (ketoconazole, erythromycin, cyclosporine, etc.) increase plasma concentrations of sibutramine metabolites with an increase in heart rate and a clinically insignificant increase in the QT interval.
Rifampicin, macrolide antibiotics, phenytoin, carbamazepine, phenobarbital and dexamethasone can accelerate the metabolism of sibutramine.
The simultaneous use of several drugs that increase the level of serotonin in the blood plasma can lead to the development of serious interactions. The so-called serotonin syndrome can develop in rare cases when sibutramine is used simultaneously with selective serotonin reuptake inhibitors (drugs for the treatment of depression), with certain drugs for the treatment of migraines (sumatriptan, dihydroergotamine), with potent analgesics (pentazocine, pethidine, fentanyl), or antitussive drugs (dextromethorphan). Sibutramine does not affect the effect of oral contraceptives.
When sibutramine and alcohol were taken simultaneously, there was no increase in the negative effects of alcohol. However, alcohol is absolutely not compatible with the dietary measures recommended when taking sibutramine.
When used simultaneously with sibutramine, other drugs that affect hemostasis or platelet function increase the risk of bleeding. Drug interactions with the simultaneous use of sibutramine with drugs that increase blood pressure and heart rate have not been fully studied at present. This group of drugs includes decongestants, cough suppressants, cold and allergy medications that contain ephedrine or pseudoephedrine. Therefore, in cases of simultaneous use of these drugs with sibutramine, caution should be exercised.
The combined use of sibutramine with drugs for weight loss that act on the central nervous system or drugs for the treatment of mental disorders is contraindicated.
Overdose
Overdose
Metformin
Symptoms: when using metformin at a dose of 85 g (42.5 times the maximum daily dose), no hypoglycemia was observed, but the development of lactic acidosis was noted.
Significant overdose or associated risk factors can lead to the development of lactic acidosis.
Treatment: if signs of lactic acidosis appear, treatment with the drug must be stopped immediately, the patient must be urgently hospitalized and, after determining the lactate concentration, the diagnosis must be clarified. The most effective measure for removing lactate and metformin from the body is hemodialysis. Symptomatic treatment is also carried out.
Sibutramine
There are extremely limited data on sibutramine overdose. The most common adverse reactions associated with overdose: tachycardia, increased blood pressure, headache, dizziness. You should notify your doctor in case of suspected overdose.
Treatment: There is no special treatment or specific antidotes. It is necessary to carry out general measures: ensure free breathing, monitor the state of the cardiovascular system, and, if necessary, carry out supportive symptomatic therapy. Timely use of activated carbon, as well as gastric lavage, can reduce the intake of sibutramine in the body. Patients with high blood pressure and tachycardia can be prescribed β-blockers. The effectiveness of forced diuresis or hemodialysis has not been established. In case of overdose, you should immediately stop taking Reduxin® Forte.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25 ° C. The drug should be stored out of the reach of children.
Sibutramine belongs to the List of potent substances approved by Decree of the Government of the Russian Federation of December 29, 2007 No. 964.
Shelf life
Shelf life
3 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Biokhimik JSC, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store in a light-protected place at a temperature not exceeding 25 °С. The drug should be kept out of reach of children. Sibutramine belongs to the List of highly potent substances, approved by Decree of the Government of the Russian Federation № 964 of 29.12.2007. |
| Manufacturer | Biokhimik JSC, Russia |
| Medication form | pills |
| Brand | Biokhimik JSC |
Other forms…
Related products
Buy Reduxin Forte, 850 mg+15 mg 90 pcs with delivery to USA, UK, Europe and over 120 other countries.