No products in the cart.
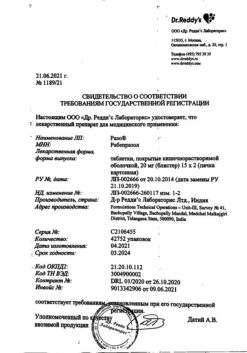
Rabeprazole, 20 mg 14 pcs
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 4660007705597
SKU: 350493
Categories: Medicine, Stomach, intestines, liver, Ulcer and gastritis
Description
An anti-ulcer drug, inhibitor of H+-K+-ATPase (proton pump). The mechanism of action is associated with inhibition of the enzyme H+-K+-ATPase in the parietal cells of the stomach, which leads to blocking the final stage of hydrochloric acid formation. This action is dose-dependent and results in inhibition of both basal and stimulated hydrochloric acid secretion regardless of the nature of the irritant.
Pharmacokinetics
After oral administration, it is absorbed from the gastrointestinal tract. At a dose of 20 mg, Cmax is reached after 3.5 h. Changes in Cmax and AUC are linear (in the dose range of 10 to 40 mg). Absolute bioavailability is about 52% due to the “first pass” effect through the liver. Bioavailability of rabeprazole does not increase with multiple dosing.
The absorption of rabeprazole is not affected by food intake and time of intake during the day.
The binding to plasma proteins is 97%.
Rabeprazole sodium undergoes a “first pass” effect. It is metabolized in the liver with the participation of CYP isoenzymes.
The main metabolites (thioether and carboxylic acid) and minor metabolites (sulfone, dimethylthioether and mercaptopuric acid conjugate) are present in low concentrations.
In healthy volunteers, T1/2 is about 1 h, total clearance is about 283 Approximately 90% is excreted with the urine primarily as two metabolites: mercaptopuric acid conjugate and carboxylic acid. In toxicological studies in laboratory animals, 2 additional unidentified metabolites were found. The remainder is excreted in the feces.
In patients with stable end-stage chronic renal failure requiring hemodialysis (CK less than 5 ml/min/1.73 m2), AUC and Cmax were 35% lower than in healthy volunteers. The average T1/2 of rabeprazole was 0.82 h in healthy volunteers, 0.95 h in patients during hemodialysis and 3.6 h after hemodialysis. In renal disease, clearance of rabeprazole in patients on hemodialysis was approximately 2 times higher than in healthy volunteers.
In patients with mild to moderate chronic hepatic impairment an increase in Cmax, T1/2, AUC was observed after a single dose of rabeprazole.
In the case of delayed CYP2C19 metabolism after taking rabeprazole at 20 mg/day for 7 days, the AUC and T1/2 were 1.9 and 1.6 respectively for extensive metabolism, while Cmax was only increased by 40%.
In elderly patients the excretion of rabeprazole is somewhat delayed.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Special Instructions
Special Instructions
Patient response to therapy with rabeprazole sodium does not exclude the presence of malignant tumors in the stomach.
Rabeprazole tablets should not be chewed or crushed. The tablets should be swallowed whole. It was found that neither time of day nor food intake influence activity of Rabeprazole sodium.
In a special study in patients with light or moderate liver dysfunction there was no significant difference of Rabeprazole sodium side effects frequency from that in healthy people of similar age and sex, but, nevertheless, it is recommended to be careful when first prescribing Rabeprazole sodium in patients with severe liver dysfunction. The AUC of rabeprazole sodium in patients with severe hepatic dysfunction is approximately twice as high as in healthy volunteers.
Patients with renal or hepatic dysfunction do not require dose adjustment of rabeprazole.
Hypomagnesemia
During treatment with PPIs for at least 3 months, cases of symptomatic and asymptomatic hypomagnesemia have rarely been reported. Most of these cases were reported one year after therapy. Serious adverse events were tetany, arrhythmias, and seizures. Most patients required treatment for hypomagnesemia, which included magnesium replacement and withdrawal of PPI therapy. In patients who will receive long-term treatment or who take PPIs with drugs such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care providers should monitor magnesium levels before starting PPI treatment and during treatment.
Patients should not take other acid-lowering agents such as H2-receptor blockers or PPIs concomitantly with rabeprazole.
Bone fractures
Observational studies suggest that PPI therapy may lead to an increased risk of osteoporosis-related fractures of the hip, wrist or spine. The risk of fractures was increased in patients receiving high doses of PPIs for a long time (a year or more).
Concomitant use of rabeprazole with methotrexate
According to literature data, concomitant use of PPI with methotrexate (especially in high doses) can lead to increased concentration of methotrexate and/or its metabolite hydroxy methotrexate and increase elimination half-life, which may lead to methotrexate toxicity. Temporary discontinuation of PPI therapy may be considered if high doses of methotrexate are necessary.
Clostridium difficile
PPI therapy may result in an increased risk of gastrointestinal infections such as Clostridium difficile.
Contraindications
Contraindications
Side effects
Side effects
Overdose
Overdose
Similarities
Similarities
Additional information
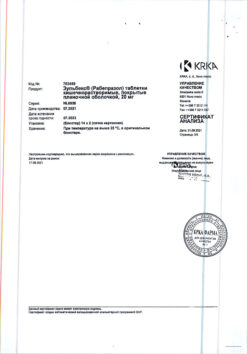
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In the dark place at a temperature not exceeding 25 ° C. Keep out of reach of children. |
| Manufacturer | Izvarino Pharma, Russia |
| Medication form | enteric soluble tablets |
| Brand | Izvarino Pharma |
Other forms…
Related products
Buy Rabeprazole, 20 mg 14 pcs with delivery to USA, UK, Europe and over 120 other countries.