No products in the cart.
Pragisan, 200 mg capsules 10 pcs
€7.23 €6.03
Out of stock
(E-mail when Stock is available)
Description
Pragisan is a gestagen, a corpus luteum hormone. Binding to receptors on the surface of target organ cells, it penetrates the nucleus where, by activating DNA, it stimulates RNA synthesis. It promotes the transition of the uterine mucosa from the proliferation phase caused by follicular hormone to the secretory phase, and after fertilization to the state necessary for the development of the fertilized egg. It reduces the excitability and contractility of the uterine muscles and fallopian tubes and stimulates the development of mammary gland terminal elements.
Stimulating protein lipase, increases fat stores, increases glucose utilization by increasing the concentration of basal and stimulated insulin, promotes the accumulation of glycogen in the liver, increases the production of aldosterone; In small doses accelerates, and in large – suppresses production of gonadotropic hormones of the pituitary gland; reduces azotemia, increases excretion of nitrogen in the urine. Activates the growth of the secretory division of mammary gland acini and induces lactation. Promotes the development of normal endometrium.
Pharmacokinetics
In oral administration
p> Absorption
Micronized progesterone is well absorbed in the gastrointestinal tract. The plasma concentration of progesterone increases gradually during the first hour, Cmax is noted 1-3 h after administration.
Metabolism
Metabolized in the liver with the participation of the CYP 2C19 isoenzyme. The main metabolites that are determined in blood plasma are 20-alpha-hydroxy-delta-4-alpha-pregnanolone and 5-alpha-dihydroprogesterone.
Excretion
Extracted in the urine as metabolites. 95% of these are glucuronconjugated metabolites, mainly 3-alpha, 5-beta-pregnandiol (pregnandione). These metabolites, which are determined in plasma and urine, are similar to substances produced during physiological corpus luteum secretion.
In vaginal administration
Intake
Absorption is rapid; progesterone accumulates in utero; high plasma concentrations of progesterone are observed 1 h after administration. Cmax progesterone in blood plasma is reached 2-6 hours after administration. When administered in doses of 100 mg 3 times/day, the average concentration is maintained for 24 hours. When administered in doses greater than 200 mg/day, the progesterone concentration corresponds to the first trimester of pregnancy.
Metabolism
Metabolized with the formation of predominantly 3-alpha, 5-beta-pregnandiol. The plasma concentration of 5-beta-pregnandiol is not increased.
Elimination
Extracted in the urine as metabolites, the main part is 3-alpha, 5-beta-pregnandiol (pregnandion).
Indications
Indications
Disorders associated with progesterone deficiency.
Oral route of administration:
infertility due to luteal insufficiency;
premenstrual syndrome;
menstrual irregularities due to ovulation or anovulation disorders;
fibrocystic mastopathy;
premenopause;
hormone replacement therapy for peri- and postmenopause (in combination with estrogen-containing drugs).
Vaginal route of administration:
hormone replacement therapy in case of progesterone deficiency with non-functioning (absent) ovaries (egg donation);
luteal phase support during preparation for in vitro fertilization;
luteal phase support in spontaneous or induced menstrual cycle;
premature menopause;
hormone replacement therapy (in combination with estrogen drugs);
infertility due to luteal insufficiency;
prevention of habitual and threatened abortion due to progestin deficiency;
prevention of uterine fibroids;
prevention of endometriosis.
Pharmacological effect
Pharmacological effect
Prajisan is a gestagen, a hormone of the corpus luteum. By binding to receptors on the surface of cells of target organs, it penetrates into the nucleus, where, activating DNA, it stimulates RNA synthesis. Promotes the transition of the uterine mucosa from the proliferation phase caused by follicular hormone to the secretory phase, and after fertilization – to the state necessary for the development of a fertilized egg. Reduces the excitability and contractility of the muscles of the uterus and fallopian tubes, stimulates the development of the end elements of the mammary gland.
By stimulating protein lipase, it increases fat reserves, increases glucose utilization, increasing the concentration of basal and stimulated insulin, promotes the accumulation of glycogen in the liver, increases the production of aldosterone; in small doses it accelerates, and in large doses it suppresses the production of gonadotropic hormones of the pituitary gland; reduces azotemia, increases nitrogen excretion in urine. Activates the growth of the secretory section of the acini of the mammary glands and induces lactation. Promotes the development of normal endometrium.
Pharmacokinetics
When taken orally
Suction
Micronized progesterone is well absorbed from the gastrointestinal tract. The concentration of progesterone in the blood plasma gradually increases during the first hour, Cmax is observed 1-3 hours after administration.
Metabolism
Metabolized in the liver with the participation of the CYP 2C19 isoenzyme. The main metabolites that are detected in blood plasma are 20-alpha-hydroxy-delta-4-alpha-pregnanolone and 5-alpha-dihydroprogesterone.
Removal
Excreted in urine in the form of metabolites. 95% of them are glucurone-conjugated metabolites, mainly 3-alpha, 5-beta-pregnanediol (pregnandione). These metabolites, which are determined in blood plasma and urine, are similar to substances formed during the physiological secretion of the corpus luteum.
For vaginal insertion
Suction
Absorption occurs quickly; progesterone accumulates in the uterus; a high concentration of progesterone in the blood plasma is observed 1 hour after administration. Cmax of progesterone in blood plasma is achieved 2-6 hours after administration. When the drug is administered at a dose of 100 mg 3 times/day, the average concentration is maintained for 24 hours. When administered in doses of more than 200 mg/day, the concentration of progesterone corresponds to the first trimester of pregnancy.
Metabolism
Metabolized to form predominantly 3-alpha, 5-beta-pregnanediol. Plasma concentrations of 5-beta-pregnanediol do not increase.
Removal
It is excreted in the urine in the form of metabolites, the main part being 3-alpha, 5-beta-pregnanediol (pregnandione).
Special instructions
Special instructions
The drug should not be used for contraception.
With long-term treatment with progesterone, periodic medical examinations (including liver function tests) are necessary; Treatment should be discontinued if there are abnormalities in diagnostic liver function tests or if cholestatic jaundice occurs. When using estrogen and/or progestagen-containing drugs, cases of the development of chloasma have been reported, especially in patients with a history of chloasma during a previous pregnancy. In women prone to developing chloasma, exposure of the skin to natural or artificial UV irradiation may cause or worsen chloasma.
Patients with a history of depression should be monitored, and if severe depression develops, the drug should be discontinued. Patients with concomitant cardiovascular diseases or a history of them should also be observed periodically by a physician.
When treated with progesterone, fluid retention may occur, which can affect the course of epilepsy, migraine, bronchial asthma, heart or kidney failure; such patients should be carefully monitored.
Impact on the ability to drive vehicles and operate machinery
When taken orally, caution must be exercised when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Progesterone
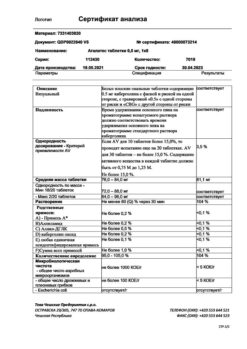
Composition
Composition
Active ingredient:
progesterone 200 mg;
Excipients:
peanut butter,
soy lecithin.
Composition of the capsule shell:
sorbitol solution 70% (uncrystallized), glycerol, gelatin, titanium dioxide, purified water.
Pregnancy
Pregnancy
The use of Prajisan during pregnancy is not contraindicated. However, there is a potential risk to the fetus (especially males) when using progesterone in the first 4 months of pregnancy. The use of micronized progesterone in the II-III trimesters of pregnancy can lead to the development of liver diseases in pregnant women. Numerous epidemiological studies have not revealed cases of fetal abnormalities when using progesterone during pregnancy.
Progesterone passes into breast milk. Data on the use of the drug during lactation are insufficient to assess the potential risk to the infant.
Contraindications
Contraindications
For oral and vaginal use
thrombophlebitis, thromboembolic disorders, intracranial hemorrhage or a history of these conditions;
bleeding from the genital tract of unknown origin;
incomplete abortion;
porphyria;
established or suspected malignant neoplasms of the mammary glands or genital organs;
hypersensitivity to the components of the drug, incl. to peanut butter, soy.
For oral use (optional)
Severe liver diseases currently (including cholestatic jaundice, hepatitis, hepatocellular carcinoma, Dubin-Johnson, Rotor syndromes) or in history, if liver function indicators have not returned to normal values.
The drug should be prescribed with caution for diseases of the cardiovascular system, arterial hypertension, chronic renal failure, diabetes mellitus, bronchial asthma, epilepsy, migraine, depression, hyperlipoproteinemia.
Side Effects
Side Effects
By oral route of administration
“Breakthrough” bleeding or shortening of the normal menstrual cycle, tension in the mammary glands (usually in the first month of treatment).
Drowsiness, transient dizziness (usually 1-3 hours after administration), nausea. These side effects can be reduced by reducing the dose, changing the drug regimen, or switching to the vaginal route of administration. These effects are usually the first signs of an overdose.
Feeling tired, migraine, headache, skin rash, itching, jaundice, fluid retention.
For oral and vaginal routes of administration
Allergic reactions (urticaria, anaphylactic shock).
Interaction
Interaction
When administered orally
With prolonged concomitant use, barbiturates, carbamazepine, hydantoin or rifampicin may reduce the effectiveness of progesterone.
Although data are limited, it is suggested that activated charcoal and griseofulvin may also reduce the effectiveness of the drug.
Progesterone may increase the therapeutic, pharmacological or toxic effects of cyclosporine, theophylline and troleandomycin.
For vaginal use
Interaction with intravaginal use has not been assessed. The simultaneous administration of other intravaginal drugs should be avoided to avoid interfering with the release and absorption of progesterone.
Overdose
Overdose
Symptoms: drowsiness, transient dizziness, shortening of the normal menstrual cycle.
Treatment: dose reduction or correction of the regimen, for example, in case of drowsiness and dizziness – 200 mg is taken at bedtime from the 12th to the 14th day of the cycle or switch to the vaginal route of administration: in the case of a shortened menstrual cycle – start treatment later in the cycle, for example from the 19th day, instead of the 17th. If necessary, carry out symptomatic treatment.
Storage conditions
Storage conditions
At temperatures below 25 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Sun Pharmaceutical Industries Ltd, India
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At temperatures below 25 °C |
| Manufacturer | Sun Pharmaceutical Industries Ltd, India |
| Medication form | capsules |
| Brand | Sun Pharmaceutical Industries Ltd |
Related products
Buy Pragisan, 200 mg capsules 10 pcs with delivery to USA, UK, Europe and over 120 other countries.