No products in the cart.
Description
Pharmacodynamics
Antitumor drug from the group of synthetic anthracycline antibiotics. It penetrates into cells quickly, localizes mainly in nucleus. On molecular level epirubicin can form a complex with DNA by intercalation between main nucleotide pairs, which leads to disruption of DNA, RNA and protein synthesis.
Intercalation in DNA is the trigger mechanism for DNA cleavage by topoisomerase II, leading to severe disruption of the tertiary structure of DNA. Epirubicin (like doxorubicin) can be involved in oxidation/reduction reactions to form highly active and highly toxic free radicals.
Pharmacokinetics
Distribution
After IV administration, epirubicin is rapidly distributed in body tissues; it does not penetrate the BBB in detectable amounts.
Metabolism
Epirubicin is extensively biotransformed primarily in the liver. The main established metabolites are epirubicinol, which has some degree of antitumor activity, and glucuronides of epirubicin and epirubicinol. The 4′-0-glucuronidation distinguishes epirubicin from doxorubicin and may account for its lower toxicity.
Elimination
After IV administration of the drug (at a dose of 60-150 mg/m2) to patients with normal hepatic and renal function, epirubicin levels decrease in a three-exponential manner with a slow terminal phase lasting 30-40 h. The T1/2 of epirubicinol corresponds to that of epirubicin. Epirubicin is excreted primarily through the liver: about 38% of the administered dose is found within 24 hours in the bile in the form of epirubicin (19%), epirubicinol and other metabolites. 9-12% of the dose is excreted in the urine (both as metabolites and unchanged). After 72 h approximately 43% of the administered dose is detected in the bile and approximately 16% in the urine.
Indications
Indications
Active ingredient
Active ingredient
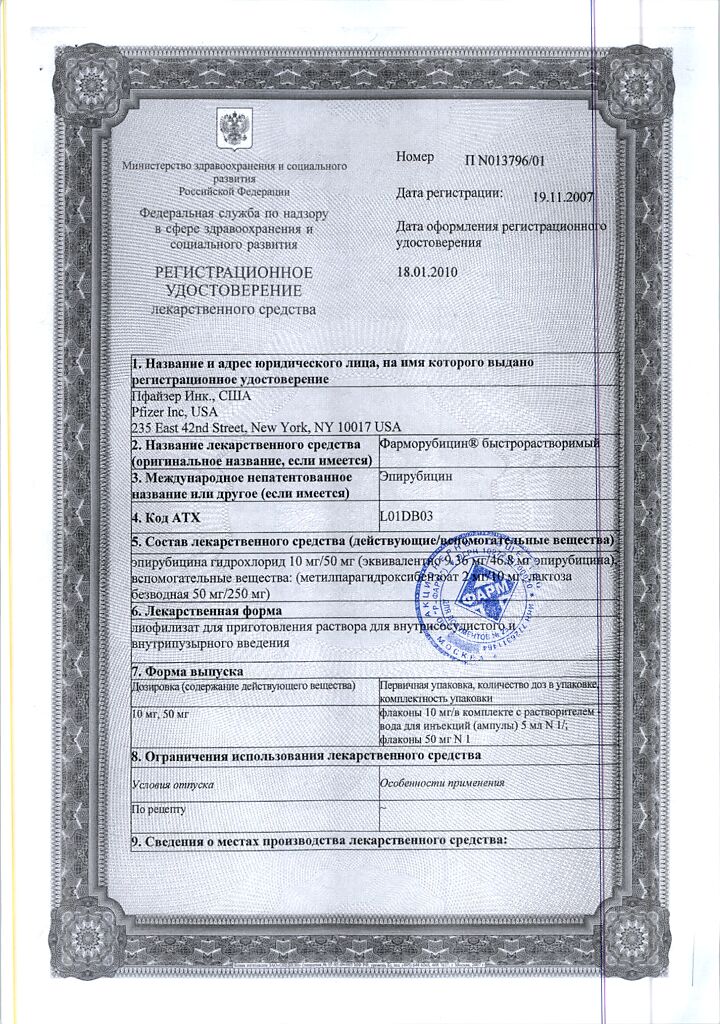
Composition
Composition
1 vial contains:
Active ingredients:
Epirubicin hydrochloride 50 mg, corresponding to an epirubicin content of 46.8 mg.
Auxiliary substances:
Methylparahydroxybenzoate,
Anhydrous.
In a vial of 50 mg of lyophilizate.
There is 1 vial in the carton pack.
How to take, the dosage
How to take, the dosage
The drug is used both as monotherapy and in combination with other cytostatics in different doses depending on the therapy regimen. Individual selection of the dose should be guided by the data of specialized literature.
When administered intravenously as monotherapy, the recommended standard dose per cycle for adults is 60-90 mg/m2 every 3-4 weeks. The total dose of the drug per cycle can be administered either at one time or divided into several injections over 2-3 consecutive days.
If the drug is used in combination with other antitumor drugs, the recommended dose per cycle should be reduced accordingly.
In individual cases, the drug may be used in higher doses of 90-120 mg/m2 once at 3-4 week intervals.
Repeated administration of the drug is possible only when all signs of toxicity (especially hematological and gastrointestinal) have disappeared.
Patients with impaired renal function and serum creatinine levels greater than 5 mg/dL should be given the drug in reduced doses.
In patients with impaired liver function, if serum bilirubin concentration is 1.2-3 mg/dL or AST value is 2-4 times the upper limit of normal, the administered dose of the drug should be reduced by 50% of the recommended dose. If the serum bilirubin concentration is more than 3 mg/dL or the AST value exceeds the upper limit by more than 4 times, the dose should be reduced by 75% of the recommended dose.
Patients who have previously received massive antitumor therapy and who have tumor infiltration of the bone marrow are recommended to receive the drug at lower doses or to increase the interval between cycles.
In elderly patients, standard doses and regimens may be used for initial therapy.
In order to reduce the risk of thrombosis and extravasation, Pharmorubicin rapidly soluble is recommended to be administered through a tube IV infusion system during a drip infusion of 0.9% sodium chloride solution or 5% glucose solution. The duration of infusion should be from 3 to 20 minutes, depending on the dose of the drug and the volume of the infusion solution.
To treat superficial tumors of the bladder, 8 weekly instillations of the drug in the bladder in a dose of 50 mg (dissolved in 25-50 ml of physiological solution) are recommended. In case of symptoms of local toxic effect (chemical cystitis manifested by dysuria, polyuria, nycturia, painful urination, hematuria, bladder discomfort, necrosis of the bladder wall) the dose should be reduced to 30 mg.
In the treatment of bladder cancer in situ, depending on individual tolerance, the dose of the drug may be increased to 80 mg.
In order to prevent recurrence after transurethral resection of superficial tumors, 4 weekly instillations of 50 mg followed by 11 monthly instillations at the same dose are recommended.
Pharmorubicin rapidly soluble should be instilled through a catheter and left inside the bladder for 1 hour. During instillation, the patient should turn over to ensure even exposure of the solution to the bladder mucosa. To avoid excessive dilution of the drug with urine, the patient should be warned to refrain from drinking for 12 hours before instillation. The patient should empty the bladder at the end of the instillation procedure.
Particular attention should be given to problems associated with catheterization (including urinary tract obstruction due to massive intravesical tumors).
In hepatocellular cancer, to provide intense local effects and simultaneously reduce overall toxic effects, Pharmorubicin fast-acting can be administered intra-arterially into the main hepatic artery at a dose of 60-90 mg/m2 at intervals of 3 weeks to 3 months or at doses of 40-60 mg/m2 at intervals of 4 weeks.
Interaction
Interaction
In coadministration of Pharmorubicin fast-acting may increase the toxic effects of other anticancer drugs, especially the myelotoxic effect and the effect on the gastrointestinal tract.
When concomitant use of Pharmorubicin rapidly soluble with other potentially cardiotoxic or cardioactive drugs (calcium channel blockers), cardiac activity should be monitored throughout treatment.
When used together, cimetidine prolongs the half-life of epirubicin (this combination is not recommended).
Pharmaceutical Interactions
Pharmorubicin should not be mixed with other drugs.
Pharmorubicin should not be allowed in contact with solutions that have an alkaline reaction, as this may lead to hydrolysis of epirubicin.
Pharmorubicin rapidly soluble should not be mixed with heparin because of their chemical incompatibility, which results in a precipitate.
Special Instructions
Special Instructions
Pharmorubicin fast-acting should only be administered under the supervision of qualified physicians experienced in antitumor therapy.
In order to reduce the risk of toxic cardiac damage, regular monitoring of cardiac function, including evaluation of left ventricular ejection fraction by EchoCG or multichannel radioisotope angiography (MCRA) and ECG monitoring, is recommended before and during therapy with Pharmorubicin rapidly soluble. If signs of chronic cardiotoxicity are detected, the drug should be discontinued immediately.
Acute cardiotoxicity in most cases is reversible and usually does not indicate withdrawal of the drug. Late (delayed) toxicity (cardiomyopathy) depends on the cumulative dose; therefore, the cumulative dose of Pharmorubicin fast-acting (900-1000 mg/m2) may be exceeded only in exceptional cases. Risk factors of cardiotoxicity include: cardiovascular diseases (including latent forms), radiation therapy of the mediastinum (ongoing or previous), anthracycline or anthracenedione therapy in the history, concomitant administration of other drugs with negative inotropic effect. Cardiotoxic manifestations usually develop against the background of therapy or within 2 months after its termination, but in some cases there may be delayed side effects (several months or even years after therapy termination).
Hematologic parameters (number of leukocytes, platelets and other blood cells, hemoglobin content) and hepatic function tests should be evaluated before and during each cycle of therapy (especially when using the drug in high doses).
In case of the first signs of extravasation (burning or soreness at the injection site) the infusion should be stopped immediately, and then the drug should be resumed in another vein. If necessary, local symptomatic therapy (including ice packs) should be carried out.
Pharmorubicin fast-acting may cause hyperuricemia due to rapid lysis of tumor cells, therefore, patients should have their uric acid, potassium, calcium and creatinine levels determined during therapy. To reduce the risk of complications associated with tumor lysis syndrome and to prevent hyperuricemia, adequate hydration of the patient, correction of acid-base balance (alkalinization) and prophylactic administration of allopurinol should be provided.
Men and women receiving Pharmorubicin fast-acting should use reliable contraceptive methods.
The rules for handling cytotoxic substances must be followed when handling the drug. It is recommended to treat surfaces contaminated with the drug with diluted solution of sodium hypochlorite (with a chlorine content of 1%). In case of accidental contact of the powder or solution with skin, it is required to wash immediately with soap and water or sodium bicarbonate solution, in case of eye contact it is necessary to rinse the eye with plenty of water for 15 minutes.
Contraindications
Contraindications
For intravenous administration:
For insertion into the bladder:
Side effects
Side effects
Blood system disorders: leukopenia, neutropenia (usually transient, reaching its lowest level 10-14 days after drug administration; recovery of the blood picture is usually observed by 21 days), thrombocytopenia, anemia.
Cardiovascular system disorders: manifestations of early (acute) cardiotoxicity – sinus tachycardia and/or abnormalities on ECG (nonspecific ST segment and T-wave changes), possibly tachyarrhythmias, including ventricular extrasystole and ventricular tachycardia, and bradycardia, AV-blockade, Gis bundle branch block (these phenomena are not always a prognostic factor for the subsequent development of delayed cardiotoxicity, they are rarely clinically significant and usually do not require cancellation of therapy with the drug). The manifestations of late (delayed) cardiotoxicity include decreased left ventricular ejection fraction and/or development of symptoms of congestive heart failure, such as dyspnea, pulmonary edema, orthostatic edema, cardiomegaly and hepatomegaly, oligouria, ascites, exudative pleurisy, galloping rhythm. Pericarditis and myocarditis are possible. The most severe form of anthracycline-induced cardiomyopathy is life-threatening congestive heart failure, which limits the cumulative dose of the drug. Thromboembolic complications are possible, including pulmonary embolism (in some cases fatal).
In the digestive system: anorexia, stomatitis, nausea, vomiting, hyperpigmentation of the oral mucosa, esophagitis, abdominal pain or burning sensation, gastric erosions, bleeding from the stomach, colitis, diarrhea; increased liver transaminase activity and serum bilirubin level.
Urinary system disorders: urine staining red for 1-2 days after drug administration; hyperuricemia is possible.
An organ of vision: conjunctivitis, keratitis.
Endocrine system disorders: amenorrhea (usually at the end of treatment ovulation is restored, but premature menopause may develop); oligospermia, azoospermia (in some cases sperm count is restored to normal levels, this may occur several years after treatment ends); hot flashes in the face.
Dermatological reactions: alopecia, rash, itching, sudden redness of the skin, hyperpigmentation of the skin and nails, photosensitization, hypersensitivity of previously exposed skin.
Others: malaise, asthenia, fever, chills, anaphylactic reactions, acute lympholeukemia, myeloleukemia.
Local reactions: erythematous striation along the course of the vein into which the infusion was made; then there may be local phlebitis or thrombophlebitis; phlebosclerosis, especially if repeatedly injected into a small vein. Local soreness, severe cellulitis, and tissue necrosis may occur if the drug enters the surrounding tissue.
Side effects possible with intra-arterial administration: in addition to systemic toxicity – gastric and duodenal ulcer (probably due to reflux into the gastric artery); narrowing of the bile ducts due to drug-induced sclerosing cholangitis.
Overdose
Overdose
Symptoms: severe myelosuppression (mainly leukopenia and thrombocytopenia), toxic gastrointestinal manifestations (mucositis), acute cardiac complications.
Treatment: symptomatic therapy is carried out. The antidote to epirubicin is unknown.
Pregnancy use
Pregnancy use
The drug is contraindicated in pregnancy and lactation.
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | In a light-protected place, at 2-8 °C |
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | solution for infusion |
| Brand | Pfizer |
Related products
Buy Pharmorubicin fast-soluble, lyophilizate, 50 mg with delivery to USA, UK, Europe and over 120 other countries.