No products in the cart.
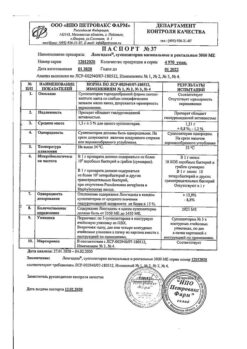
Pergoveris, lyophilizate 150 me+75 me
€1.00
Out of stock
(E-mail when Stock is available)
EAN: 4607069190794
SKU: 217893
Categories: Gynecology and Obstetrics, Infertility treatment IVF, Medicine
Description
Pergoveris® is a combined drug containing recombinant human FSH (folletropin alpha, p-FSHh) and recombinant human LH (lutropin alpha, p-LHhh). The drug is produced by genetically engineered method on Chinese hamster ovary cell culture.
The main role of FSH is to initiate folliculogenesis by acting on the granulosa cells of the developing follicle, whereas LH plays an important role in enhancing the production of estradiol by the mature follicle and inducing follicular maturation and ovulation at its peak. LH supports the functioning of the corpus luteum and thus ensures the onset and development of early pregnancy.
In the process of follicle development, FSH, together with estradiol, induces LH receptors on the membrane of granulosa cells.
The effect of LH on theca cells ensures the production of androgens for granulosa cells, where the transformation of androgens into estrogens takes place through the aromatase system. Thus, in the absence of LH, FSH can induce follicular growth, but estradiol synthesis is reduced. Without sufficient estradiol, the conditions for pregnancy are impaired, as well as cervical mucus secretion, endometrial growth and maturation of the full corpus luteum in response to human hCG (hCG) administration.
In clinical studies, the efficacy of a combination of follitropin alfa and lutropin alfa has been shown in hypogonadotropic hypogonadism in women.
In stimulating follicle development in women with anovulation with LH and FSH deficiency, the main effect of lutropin alfa is to increase estradiol secretion by follicles, whose growth is in turn stimulated by FSH.
. In women with hypogonadotropic hypogonadism and a serum LH concentration below 1.2 IU/L, daily use of a combination of lutropin alfa at 75 IU and follitropin alfa at 150 IU has been shown to result in adequate follicle development and increased estradiol synthesis, whereas a combination of lutropin alfa 25 IU and follitropin alfa 150 IU does not provide this effect.
Hence, when less than one vial of Pergoveris® per day is prescribed, LH activity may not be sufficient for full follicle development.
While the efficacy of p-LHF monotherapy in assisted reproductive technology (ART) has been proven, published results from clinical trials suggest the benefits of p-LHF supplementation in patients with insufficient (suboptimal) efficacy of p-LHF monotherapy.
The addition of p-LHF is intended to increase ovarian sensitivity to p-FSHh, to stimulate oestradiol secretion by the preovulatory follicle to induce endometrial growth, and to allow later luteinization of follicles, resulting in normalization of progesterone levels in the luteal phase.
Pharmacokinetics
Follitropin alfa and lutropin alfa administered in combination retain the same pharmacokinetic characteristics as they do individually.
Follitropin alfa
After IV administration, follitropin alfa is distributed in extracellular fluids, with an initial T1/2 of about 2 h from the body, whereas the final T1/2 is about 24 h. The Vss value is 10 L, the total clearance is 0.6 L/h. One eighth of the administered dose of follitropin alfa is excreted by the kidneys.
When administered by injection the absolute bioavailability is about 70%. After repeated injections, a threefold cumulation of the drug in blood is observed compared to a single injection. Stationary Css in the blood is reached within 3-4 days. It has also been shown that in women with suppressed endogenous gonadotropin secretion, follitropin alfa effectively stimulates follicle development and steroidogenesis despite inaccessibly low LH levels for quantitative measurement.
Lutropin alfa
After IV administration, lutropin alfa is rapidly distributed with an initial T1/2 of about 1 h, and excreted with a final T1/2 of about 10-12 h. Vss is 10 to 14 L. Lutropin alfa exhibits a linear pharmacokinetic profile, as evidenced by a direct proportional relationship of AUC to the administered dose. Total clearance is about 2 l/h, less than 5% of the dose is excreted by the kidneys.
The average retention time of the drug in the body is 5 hours.
After oral administration lutropin alfa is rapidly distributed in organs and tissues, the absolute bioavailability is about 60%; the final T1/2 is slightly prolonged. The pharmacokinetics of lutropin alfa with single administration is comparable with that with multiple administration, the degree of cumulation is minimal. No pharmacokinetic interaction was observed when lutropin alfa was administered concomitantly with follitropin alfa.
Indications
Indications
Stimulation of growth and maturation of follicles in women with severe LH and FSH deficiency; suboptimal response in patients with previously performed controlled ovarian stimulation (COS), which was characterized by either a small number of obtained preovulatory follicles/oocytes (less than 7), or the use of high doses of FSH (3000 IU or more/per 1 cycle), or the age of the patient (35 years and older), both individually and in combination, during an assisted reproductive technology (ART) program: in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), gamete/zygote transplantation into the fallopian tubes (GIFT/ZIFT).
Pharmacological effect
Pharmacological effect
The drug Pergoveris® is a combined drug containing recombinant human FSH (follitropin alfa, r-FSH) and recombinant human LH (lutropin alfa, r-LH). The drug is obtained by genetic engineering using a culture of Chinese hamster ovary cells.
The main role of FSH is to initiate folliculogenesis by acting on the granulosa cells of the developing follicle, while LH plays an important role in enhancing the production of estradiol by the mature follicle, inducing follicle maturation and ovulation at the peak of its activity. LH supports the functioning of the corpus luteum and, thereby, ensures the onset and development of pregnancy in the early stages.
During follicle development, FSH, together with estradiol, induces LH receptors on the membrane of granulosa cells.
The effect of LH on theca cells ensures the production of androgens for granulosa cells, where the transformation of androgens into estrogens occurs through the aromatase system. Thus, in the absence of LH, FSH can induce follicular growth, but the synthesis of estradiol is reduced. Without a sufficient amount of estradiol, the conditions for pregnancy are disrupted, as well as the secretion of cervical mucus, the growth of the endometrium and the maturation of a full-fledged corpus luteum in response to the administration of human hCG (hCG).
In clinical studies, the effectiveness of the combination of follitropin alfa and lutropin alfa was shown for hypogonadotropic hypogonadism in women.
When stimulating the development of follicles in women with anovulation with LH and FSH deficiency, the main effect of lutropin alfa is to increase the secretion of estradiol by the follicles, the growth of which, in turn, is stimulated by FSH.
It has been shown that in women with hypogonadotropic hypogonadism and serum LH concentrations below 1.2 IU/l, daily use of a combination of lutropin alfa at a dose of 75 IU and follitropin alfa at a dose of 150 IU leads to adequate development of follicles and an increase in the synthesis of estradiol, while the combination of lutropin alfa 25 IU and follitropin alfa 150 IU does not provides such an effect.
Thus, when prescribing less than one bottle of Pergoveris® per day, LH activity may be insufficient for the full development of follicles.
Although the effectiveness of r-FSH monotherapy when using assisted reproductive technologies (ART) has been proven, published results of clinical studies indicate the benefits of additional administration of r-FSH in patients with insufficient (suboptimal) effectiveness of r-FSH monotherapy.
The addition of r-LGH is intended to increase the sensitivity of the ovaries to r-FSH, to stimulate the secretion of estradiol by the preovulatory follicle, causing endometrial growth, and also to ensure later luteinization of the follicles, leading to normalization of progesterone levels in the luteal phase.
Pharmacokinetics
Follitropin alfa and lutropin alfa, administered in combination, retain the same pharmacokinetic characteristics as separately.
Follitropin alfa
After intravenous administration, follitropin alpha is distributed in extracellular fluids, and its initial T1/2 from the body is about 2 hours, while the final T1/2 is about 24 hours. The Vss value is 10 l, the total clearance is 0.6 l/h. One-eighth of the administered dose of follitropin alfa is excreted by the kidneys.
With subcutaneous administration, absolute bioavailability is about 70%. After repeated injections, a threefold accumulation of the drug in the blood is observed compared to a single injection. Steady-state Css in the blood is achieved within 3–4 days. It has also been shown that in women with suppressed secretion of endogenous gonadotropins, follitropin alfa effectively stimulates follicular development and steroidogenesis, despite LH levels that are inaccessibly low for quantitative measurement.
Lutropin alfa
After intravenous administration, lutropin alfa is quickly distributed with an initial T1/2 of about 1 hour, and is excreted from the body with a final T1/2 of about 10–12 hours. Vss is from 10 to 14 l. Lutropin alfa exhibits a linear pharmacokinetic profile, as evidenced by the direct proportionality of AUC to the administered dose. The total clearance is about 2 l/h, less than 5% of the dose is excreted by the kidneys.
The average retention time of the drug in the body is 5 hours.
After subcutaneous administration, lutropin alfa is quickly distributed in organs and tissues, absolute bioavailability is about 60%; the final T1/2 is somewhat lengthened. The pharmacokinetics of lutropin alfa with a single administration is comparable to that with repeated administration, the degree of accumulation is minimal. When lutropin alfa was coadministered with follitropin alfa, no pharmacokinetic interaction was observed.
Special instructions
Special instructions
The drug Pergoveris® contains active substances of gonadotropins, which can cause adverse reactions of varying severity, therefore the drug should be prescribed only by a doctor with appropriate specialization and experience in the treatment of infertility. The start of therapy should be preceded by an examination of the infertile couple, in particular, studies should be carried out to exclude hypothyroidism, adrenal insufficiency, hyperprolactinemia, hypothalamic-pituitary tumors.
To administer gonadotropin therapy, the attending physician must have the necessary equipment and sufficient time to monitor the patient.
Safe and effective therapy with Pergoveris® requires regular monitoring of follicular development using ultrasound, and, if possible, monitoring of serum estradiol concentrations.
In patients with porphyria, as well as in the presence of porphyria in relatives, careful monitoring is required during therapy with Pergoveris®. If the condition worsens or the first signs of this disease appear, it may be necessary to discontinue therapy.
Pergoveris® contains less than 1 mmol (23 mg) sodium in 1 dose, that is, it is not a significant source of sodium.
The drug Pergoveris® contains 30 mg of sucrose per dose, which should be taken into account when prescribing the drug to patients with concomitant diabetes mellitus.
With ovarian stimulation, the risk of ovarian hyperstimulation increases due to the possibility of an excessive estrogen response and multiple follicular development.
The minimum effective dose should be used.
It is known that there is individual variability in response to the treatment of r-FSH/r-LHch, incl. insufficient response in some patients. In clinical studies, the use of a combination of lutropin alfa and follitropin alfa led to an increase in the sensitivity of the ovaries to gonadotropins. If it is necessary to increase the dose of r-FSH, it is recommended to increase it by 37.5–75 IU of follitropin alfa every 7–14 days.
OHSS must be differentiated from uncomplicated ovarian enlargement. Clinical symptoms of OHSS may appear with increasing severity. Characterized by a significant increase in the size of the ovaries, high levels of sex hormones, increased vascular permeability, leading to the accumulation of fluid in the abdominal, pleural and, less commonly, pericardial cavities.
The following symptoms are most typical for severe OHSS: pain and a feeling of fullness in the abdomen, a marked increase in the size of the ovaries, increased body weight, shortness of breath, oliguria, gastrointestinal symptoms (nausea, vomiting, diarrhea); Hypovolemia, hemoconcentration, electrolyte imbalance, ascites, hemoperitonium, pleural effusion, acute respiratory distress syndrome, and thromboembolic disorders occur.
In very rare cases, severe OHSS may be complicated by ovarian torsion, pulmonary embolism, ischemic stroke, or myocardial infarction.
If hCG is not administered to induce ovulation, an excessive ovarian response will cause significant hyperstimulation to develop in rare cases.
Therefore, if the ovaries respond excessively to stimulation, hCG is not prescribed, and patients are advised to abstain from coitus or use barrier methods of contraception for at least 4 days.
OHSS can progress rapidly (from a day to several days) to a severe condition, so after administration of hCG, observation for at least two weeks is necessary.
To minimize the risk of OHSS and multiple pregnancies, ultrasound and assessment of serum estradiol concentrations are regularly used. During anovulation, the risk of developing OHSS increases with an estradiol concentration of >900 pg/ml (3300 pmol/ml) and the presence of more than 3 follicles with a diameter of at least 14 mm.
Strict adherence to the recommended dosage of Pergoveris® and follitropin alfa, as well as careful monitoring of therapy, minimizes the risk of developing OHSS and multiple pregnancies.
When pregnancy occurs, the severity of OHSS may worsen and its duration may increase. Most often, OHSS occurs after cessation of hormonal therapy and reaches its maximum 7–10 days after this. As a rule, OHSS disappears spontaneously with the onset of menstruation.
If severe OHSS develops, gonadotropin therapy, if still ongoing, should be discontinued. The patient should be hospitalized and given OHSS-specific therapy.
Patients with polycystic ovary syndrome are at higher risk of developing OHSS.
Multiple pregnancy
The frequency of multiple pregnancies and births with ovulation induction is higher compared to natural conception; the most common option for multiple births is twins. To minimize the risk of multiple pregnancies, careful monitoring of the ovarian response is necessary.
With ART, the risk of multiple pregnancy is mainly related to the number of embryos transferred, their viability and the age of the patient.
Miscarriage
The incidence of miscarriage after ovulation induction and ART programs is higher than in the population.
Ectopic pregnancy
Patients with a history of fallopian tube disease have an increased risk of ectopic pregnancy. The chance of an ectopic pregnancy after assisted reproductive technology is 2 to 5%, compared to 1 to 1.5% in the general population.
Neoplasms of the reproductive system
There are reports of benign and malignant neoplasms of the ovary and other reproductive organs in women after undergoing numerous and varied courses of infertility treatment. To date, no connection has been established between gonadotropin therapy and an increased risk of neoplasms in infertility.
Congenital malformations
The incidence of congenital anomalies after the use of assisted reproductive technology programs may be slightly higher than during natural pregnancy and childbirth. However, it is unknown whether this is due to factors causing the couple’s infertility or directly to ART procedures.
Based on data from clinical studies and post-marketing monitoring, there is no evidence that the use of gonadotropins in the treatment of infertility increases the risk of developing congenital anomalies in the offspring of patients.
Thromboembolic complications
In patients with recent or current thromboembolic diseases, as well as at a probable risk of their occurrence, the use of gonadotropins may increase this risk or complicate the course of these diseases. For patients in this group, the benefits of therapy must be weighed against the possible risks. It should be noted that pregnancy itself carries an increased risk of thromboembolic disorders.
Patients should be aware of the above risks before starting therapy. If OHSS or multiple pregnancy occurs immediately, a decision to discontinue therapy should be considered.
The patient must inform the doctor about all types of allergic reactions, as well as about all drugs used before starting treatment with Pergoveris®.
Active ingredient
Active ingredient
Follitropin alfa, Lutropin alfa
Composition
Composition
Active ingredients:
follitropin alpha 150 IU (11 mcg);
lutropin alfa 75 IU (3 mcg);
Excipients:
sucrose – 30 mg,
sodium hydrogen phosphate dihydrate – 1.11 mg,
sodium dihydrogen phosphate monohydrate – 0.45 mg,
methionine – 0.1 mg,
polysorbate 20 – 0.05 mg,
concentrated phosphoric acid – up to pH 6.5–7.5,
sodium hydroxide – up to pH 6.5–7.5
Pregnancy
Pregnancy
Pergoveris® is contraindicated for use during pregnancy and breastfeeding.
Contraindications
Contraindications
hypersensitivity to any of the active or excipients or their combination;
tumors of the hypothalamus and/or pituitary gland;
voluminous neoplasms or ovarian cysts not caused by polycystic ovary syndrome;
uterine and/or other gynecological bleeding of unknown etiology;
ovarian cancer, uterine cancer, breast cancer;
pregnancy and lactation;
primary ovarian failure;
developmental anomalies of the female genital organs incompatible with pregnancy;
fibroid tumors of the uterus, incompatible with pregnancy.
Side Effects
Side Effects
From the side of the central nervous system: very often – headache; often – drowsiness.
From the genital organs and mammary gland: very often – ovarian cysts; often – ovarian hyperstimulation syndrome (OHSS) of mild severity (accompanied by pain in the lower abdomen, nausea, vomiting, weight gain, enlargement of the ovaries, including due to the formation of cysts); often – OHSS of moderate severity (in addition to pain in the lower abdomen, nausea, vomiting, weight gain in the body and ovaries, shortness of breath, oliguria, ascites, pleural effusion, fluid accumulation in the pericardial cavity may be noted).
Detailed information is in the “Special Instructions” section; often – pain in the mammary glands; pelvic pain; uncommon – severe form of OHSS (may be accompanied by severe forms of ascites, pleural effusion, accumulation of fluid in the pericardial cavity, oliguria, acute respiratory distress syndrome and pulmonary embolism (very rare). Detailed information is in the section “Special instructions”; rarely – torsion of an ovarian cyst (as a complication of OHSS).
From the gastrointestinal tract: often – abdominal pain, nausea, vomiting, diarrhea, abdominal colic, flatulence.
From the heart and blood vessels: very rarely – thromboembolism, usually associated with severe OHSS.
From the respiratory system: very rarely – worsening or exacerbation of asthma in patients with bronchial asthma.
From the immune system: very rarely – systemic allergic reactions of varying severity (redness of the skin, urticaria, rash, facial swelling, difficulty breathing, generalized edema, anaphylaxis, fever, arthralgia).
Local reactions: very often – reactions of varying severity at the injection site (pain, redness, bruising, swelling).
Interaction
Interaction
There have been no reports of incompatibility between Pergoveris® and other medicinal products.
Mixing Pergoveris® with any other drug in the same syringe is not allowed, with the exception of follitropin alfa.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in original packaging
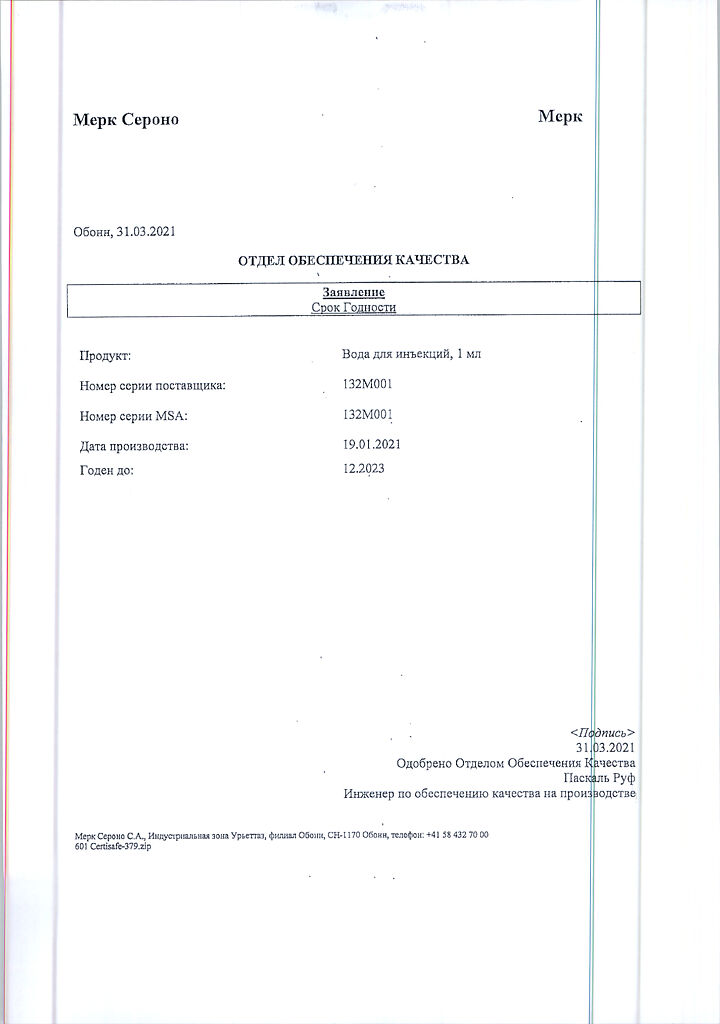
Shelf life
Shelf life
3 years
Manufacturer
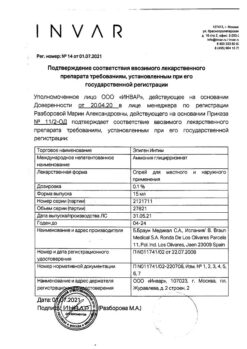
Manufacturer
Merck Serono S.A., Switzerland
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C, in the original package |
| Manufacturer | Merck Serono S.A., Switzerland |
| Medication form | lyophilizate |
| Brand | Merck Serono S.A. |
Related products
Gynecology and Obstetrics
Gynecology and Obstetrics
Gynecology and Obstetrics
Prepidil, intracervical gel 0.5 mg/3 g syringes with catheter
Buy Pergoveris, lyophilizate 150 me+75 me with delivery to USA, UK, Europe and over 120 other countries.