No products in the cart.
Description
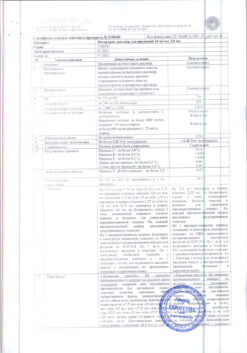
Pharmacotherapeutic group: antitumor agent, alkaloid
ATCode: LCD01
Pharmacological properties
Pharmacodynamics Paclitaxel is a semi-synthetic cytostatic anticancer drug from the taxane group. The mechanism of its action is connected with affecting the process of cell division through stimulation of assembly of intracellular structures – microtubules from dimeric tubulin molecules, stabilization of their structure, suppression of depolymerization and inhibition of dynamic reorganization which disrupts cell division in M-phase of cell cycle. In addition, paclitaxel induces the formation of abnormal clusters, or “bundles”, of microtubules throughout the cell cycle and causes the formation of multiple star-shaped clusters of microtubules during mitosis. Perimental evidence suggests it has mutagenic and embryotoxic properties and causes decreased reproductive function. Pharmacokinetics Paclitaxel plasma concentration after intravenous administration decreases according to biphasic kinetics. Paclitaxel pharmacokinetics were determined after infusions of the drug at doses of 135 and 175 mg/m2 for 3 and 24 hours. The half-life and total clearance of paclitaxel are variable and depend on the dose and duration of administration: from 13.0-52.7 hours, 12.2 to 23.8 L/m/m2 respectively. The average volume of distribution is 198 to 688 L/m2. No paclitaxel cumulation has been observed with repeated courses of treatment. The binding to plasma proteins averages 89%. Studies in vitro on hepatic microsomes revealed that paclitaxel is metabolized in the liver with the participation of the CYP2C8 isoenzyme to 6-alpha-hydroxypaclitaxel and the CYP3A4 isoenzyme to 3-parahydroxypaclitaxel and 6-alpha, 3-parahydroxypaclitaxel. Extracted. After an intravenous infusion of paclitaxel (15-275 mg/m2) for 1, 6, or 24 hours, 1.3-12.6% of the administered dose was excreted unchanged by the kidneys. After a 3-hour infusion of radioactively labeled paclitaxel at doses of 225-250 mg/m2 for 120 hours, 14% of the radioactivity was excreted by the kidneys, 71% by the gut, and 5% of the injected radioactivity was excreted unchanged, the rest being metabolites, mainly 6-alpha-hydroxypaclitaxel.
Indications
Indications
Ovarian cancer
First-line therapy in combination with platinum antineoplastic agents in patients with advanced ovarian cancer or residual tumor (>1 cm) after initial laparotomy;
second-line therapy in patients with metastatic ovarian cancer after standard therapy has not led to a positive result.
Breast cancer
adjuvant therapy in patients with metastases in the lymph nodes after standard combination chemotherapy;
first-line therapy in patients with late-stage cancer or metastatic cancer after disease relapse within 6 months after the start of adjuvant therapy with anthracycline drugs, in the absence of contraindications for their use;
first-line therapy in patients with late-stage or metastatic breast cancer in combination with anthracycline drugs in the absence of contraindications for their use, or in combination with trastuzumab in patients with immunohistochemically confirmed 2+ or 3+ HER-2 levels;
Second-line therapy in patients with advanced or metastatic cancer who have progressed after combination chemotherapy. Previous therapy should include anthracycline drugs in the absence of contraindications for their use.
Non-small cell lung cancer
First-line therapy in combination with cisplatin or as monotherapy in patients who are not planned for surgery and/or radiation therapy.
Kaposi’s sarcoma due to AIDS
second line therapy.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: antitumor agent, alkaloid
ATX code: L01CD01
Pharmacological properties
Pharmacodynamics
Paclitaxel is a cytostatic anticancer drug from the group of taxanes, obtained semisynthetically.
The mechanism of its action is associated with the influence on the process of cell division by stimulating the assembly of intracellular structures – microtubules from dimeric tubulin molecules, stabilizing their structure, suppressing depolymerization and inhibiting dynamic reorganization, which disrupts cell division in the M-phase of the cell cycle.
In addition, paclitaxel induces the formation of abnormal clusters, or “bundles,” of microtubules throughout the cell cycle and causes the formation of multiple star-shaped clusters of microtubules during mitosis.
According to experimental data, it has mutagenic and embryotoxic properties and causes a decrease in reproductive function.
Pharmacokinetics
The concentration of paclitaxel in blood plasma after intravenous administration decreases in accordance with biphasic kinetics.
The pharmacokinetics of paclitaxel was determined after infusions of the drug at doses of 135 and 175 mg/m2 for 3 and 24 hours. The half-life and total clearance of paclitaxel are variable and depend on the dose and duration of administration: from 13.0 to 52.7 hours, from 12.2 to 23.8 l/h/m2, respectively.
The average volume of distribution ranges from 198 to 688 l/m2.
With multiple courses of treatment, no accumulation of paclitaxel was observed.
The binding to plasma proteins averages 89%. In vitro studies on liver microsomes revealed that paclitaxel is metabolized in the liver with the participation of the CYP2C8 isoenzyme to 6-alpha-hydroxypaclitaxel and the CYP3A4 isoenzyme to 3-parahydroxypaclitaxel and 6-alpha, 3-paradihydroxypaclitaxel.
Excretion. After intravenous infusion of paclitaxel (15-275 mg/m2) over 1, 6 or 24 hours, 1.3-12.6% of the administered dose was excreted unchanged by the kidneys. After a 3-hour infusion of radiolabeled paclitaxel in doses of 225-250 mg/m2 for 120 hours, 14% of the radioactivity was excreted by the kidneys, 71% by the intestines, 5% of the administered radioactivity was excreted unchanged, the rest were metabolites, mainly 6-alphahydroxypaclitaxel.
Special instructions
Special instructions
The use of Paclitaxel-Teva should be under the supervision of a physician experienced in working with anticancer chemotherapy drugs.
Because drug extravasation is possible during administration, careful monitoring of the infusion area is recommended for signs of possible infiltration.
Paclitaxel-Teva should be used as a diluted solution. Before administering the drug, patients should be premedicated with glucocorticosteroids and H1 blockers.
and H2-histamine receptors. If Paclitaxel-Teva is used in combination with cisplatin, Paclitaxel-Teva should be administered first followed by cisplatin.
Anaphylaxis and serious hypersensitivity reactions
Less than 1% of patients, despite premedication, experienced serious hypersensitivity reactions during treatment with Paclitaxel-Teva. The frequency and severity of such reactions did not depend on the dose or schedule of administration of the drug. With the development of severe reactions, the most common symptoms observed were suffocation, hot flashes, chest pain, tachycardia, as well as abdominal pain, pain in the limbs, increased sweating, and increased blood pressure.
If severe hypersensitivity reactions develop, the administration of Paclitaxel-Teva should be stopped immediately and, if necessary, symptomatic treatment should be prescribed; in such cases, repeated courses of treatment with the drug should not be prescribed.
Reactions at the injection site
During intravenous administration of the drug, the following usually mild reactions at the injection site were observed: swelling, pain at the injection site, erythema, tenderness at the injection site, induration at the injection site, hemorrhages, which can lead to the development of cellulite. Such reactions were observed more often with a 24-hour infusion than with a 3-hour infusion. In some cases, the onset of such reactions was observed both during the infusion and 7-10 days after it.
Intra-arterial administration of paclitaxel should be avoided as severe tissue reactions were observed following intra-arterial administration in local tolerability studies in animals.
Myelosuppression
Suppression of bone marrow function (mainly neutropenia) depends on the dose and regimen of the drug and is the main toxic reaction that limits the dose of the drug. For example, when cisplatin is administered at a dose of 75 mg/m2 and Paclitaxel-Teva at a dose of 175 mg/m2 as a 3-hour infusion, severe neurotoxicity is observed more often than when Paclitaxel-Teva is administered at a dose of 135 mg/m2 as a 24-hour infusion, i.e. The duration of infusion has a more significant effect on the risk of developing myelosuppression than the dose. In patients with a history of previous radiotherapy, neutropenia developed less frequently and to a milder extent, and did not worsen as the drug accumulated in the body. In patients with ovarian cancer, the risk of renal failure is higher when using the combination of Paclitaxel-Teva + cisplatin compared to cisplatin monotherapy. Infections were very common and sometimes fatal, including sepsis, pneumonia and peritonitis. Urinary and upper respiratory tract infections were noted as the most common complicated infections. At least one opportunistic infection has been reported in immunosuppressed patients, patients with HIV infection, and patients with AIDS-related Kaposi’s sarcoma.
The use of maintenance therapy, including granulocyte colony-stimulating factor, is recommended for patients who have experienced severe neutropenia.
A decrease in platelet count below 100,000/µl was observed at least once during the entire period of therapy with Paclitaxel-Teva; sometimes the platelet count was below 50,000/µl. There were also cases of bleeding, most of which were local, and the frequency of their occurrence was not associated with the dose of Paclitaxel-Teva and the administration schedule. When using the drug Paclitaxel-Teva, it is necessary to regularly monitor your blood count. The drug should not be prescribed to patients with a neutrophil count of less than 1500/μL and less than 1000/μL in patients with Kaposi’s sarcoma due to AIDS, and with a platelet count of less than 100,000/μL (75,000/μL in patients with Kaposi’s sarcoma due to AIDS).
If severe neutropenia (less than 500/μl) or severe peripheral neuropathy develops during treatment with Paclitaxel-Teva, in subsequent courses of treatment it is recommended to reduce the dose by 20% (in patients with Kaposi’s sarcoma due to AIDS – by 25%).
Effect on the cardiovascular system
The decrease, increase in blood pressure and bradycardia observed during the administration of Paclitaxel-Teva are usually asymptomatic and in most cases do not require treatment. A decrease in blood pressure and bradycardia were usually observed during the first 3 hours of infusion. ECG abnormalities in the form of repolarization disorders such as sinus tachycardia, sinus bradycardia and early extrasystole were also noted. In severe cases, treatment with Paclitaxel-Teva should be suspended or discontinued. Monitoring vital signs is recommended, especially during the first hour of drug infusion. If Paclitaxel-Teva is used in combination with trastuzumab or doxorubicin for the treatment of metastatic breast cancer, monitoring of cardiac function is recommended.
Cases of severe cardiac conduction disturbances have been reported during treatment with Paclitaxel-Teva. If symptoms of cardiac conduction disturbances are detected, patients should be prescribed appropriate therapy along with constant ECG monitoring of the cardiovascular system.
Effect on the nervous system
The frequency and severity of nervous system disorders were generally dose-related. Peripheral neuropathy, usually moderate, was often observed during treatment with Paclitaxel-Teva. The incidence of peripheral neuropathy increased as the drug accumulated in the body. Cases of paresthesia and hyperesthesia were often observed. If severe neuropathy is noted, it is recommended to reduce the dose by 20% in subsequent courses of treatment (in patients with Kaposi’s sarcoma due to AIDS – by 25%). Peripheral neuropathy may be a reason to discontinue therapy with Paclitaxel-Teva. Symptoms of neuropathy decreased or completely disappeared within several months after stopping drug therapy. The development of neuropathy during previous therapy is not a contraindication for the use of Paclitaxel-Teva.
Rarely, abnormal optic nerve evoked potentials have been reported in patients with permanent optic nerve damage.
Possible exposure to ethanol contained in Paclitaxel-Teva should be taken into account.
Effect on the gastrointestinal tract
Mild to moderate cases of nausea/vomiting, diarrhea, and mucositis were very common in all patients. Cases of mucositis development depended on the drug administration regimen and were more often observed with a 24-hour infusion than with a 3-hour infusion.
Rare cases of neutropenic enterocolitis (typhlitis), despite co-administration of granulocyte colony-stimulating factor, have been observed in patients receiving Paclitaxel-Teva as monotherapy and in combination with other chemotherapy drugs.
Liver failure
Patients with liver failure represent a risk group due to the severity of side effects, especially grade 3-4 myelosuppression. The patient’s condition should be closely monitored and, if necessary, consider adjusting the dose of the drug.
Radiation pneumonitis has been reported with concomitant radiation therapy.
Patients should use reliable methods of contraception during treatment with Paclitaxel-Teva and for at least 3 months after the end of therapy.
There is no information on the treatment of patients with initial severe cholestasis with the drug. In patients with severe liver dysfunction, paclitaxel therapy is prohibited.
Vaccination
When used together, Paclitaxel-Teva and live viral vaccines may potentiate the replication of the vaccine virus and/or side effects when using vaccines may increase, since normal protective mechanisms may be inhibited due to the use of Paclitaxel-Teva. Vaccination with live viral vaccines in patients using the drug Paclitaxel-Teva can lead to the development of severe infections. The patient’s immune response when administered such a vaccine may be reduced.
The use of live vaccines in such patients should be avoided and specialist advice should be obtained.
Fertility
Taking into account the possible mutagenic effect of Paclitaxel-Teva, patients of both sexes should be advised to use effective contraception during therapy with Paclitaxel-Teva and for 6 months after the end of therapy. Also, due to a possible decrease in fertility in men, cryopreservation of sperm may be recommended for the possibility of conceiving a child in the future.
Influence on the ability to drive vehicles and machinery
Paclitaxel-Teva contains ethanol, so during the treatment period you should refrain from driving or operating potentially dangerous machinery.
Premedication given to the patient before the administration of Paclitaxel-Teva may also have a negative effect on the ability to concentrate.
Active ingredient
Active ingredient
Paclitaxel
Composition
Composition
1 ml of the drug contains: active ingredient paclitaxel 6 mg; excipients: macrogol glyceryl ricinoleate 527 mg, anhydrous citric acid 2 mg, absolute ethanol 396 mg (up to 0.933 g, equivalent to 1 ml).
Pregnancy
Pregnancy
The drug is contraindicated for use during pregnancy and breastfeeding.
Contraindications
Contraindications
Hypersensitivity to paclitaxel or any component of the drug, especially to macrogol glyceryl ricinoleate (polyoxyethylated castor oil);
the initial neutrophil count is less than 1500/μl of blood in patients with solid tumors;
the initial or registered during treatment neutrophil content is less than 1000/μl of blood in patients with Kaposi’s sarcoma caused by AIDS;
concomitant serious uncontrolled infections in patients with Kaposi’s sarcoma;
pregnancy and breastfeeding;
children’s age (there is insufficient data on the safety and effectiveness of the drug).
With caution
Thrombocytopenia (less than 100,000/μl of blood), liver failure, acute infectious diseases (including herpes zoster, chicken pox, herpes), severe coronary heart disease, myocardial infarction (history), arrhythmias.
Side Effects
Side Effects
Side effects of paclitaxel are generally the same in frequency and severity when treating ovarian cancer, breast cancer, non-small cell lung cancer, or Kaposi’s sarcoma. However, in patients with Kaposi’s sarcoma caused by AIDS, when using the drug, infections (including opportunistic ones), suppression of hematopoiesis, and febrile neutropenia are observed more often than usual and are more severe.
Side effects with monotherapy:
The incidence of side effects is given according to the following scale: very common (≥10), common (≥100, but ˂ 1/10), uncommon (≥1000, but ˂ 1/100), rare (≥10,000, but ˂ 1/1000), very rare (˂ 10,000), frequency unknown (cannot be estimated using available data).
From the hematopoietic organs: very often – myelosuppression, neutropenia, anemia, thrombocytopenia, leukopenia, fever, bleeding; rarely* – febrile neutropenia; very rarely* – acute myeloid leukemia, myelodysplastic syndrome; frequency unknown – disseminated intravascular coagulation syndrome
From the immune system: very often – minor hypersensitivity reactions, mainly manifested in the form of hyperemia (“flushes”) and skin rash; uncommon – severe hypersensitivity reactions requiring treatment (for example, decreased blood pressure (BP), angioedema, respiratory dysfunction, generalized urticaria, edema, back pain, chills, tachycardia, abdominal pain, pain in the extremities, profuse sweating); rarely* – anaphylactic reactions (including fatal ones); very rarely* – anaphylactic shock.
From the nervous system: very often – neurotoxicity (mainly peripheral neuropathy); rarely* – motor neuropathy (leading to slight weakness of the limbs); very rarely* – confusion, autonomic neuropathy, manifested by paralytic ileus and orthostatic hypotension, grand mal seizures, convulsions, encephalopathy, dizziness, headache, ataxia.
From the cardiovascular system: very often – changes in the ECG, decreased blood pressure; often – bradycardia; uncommon – increased blood pressure, thrombosis, thrombophlebitis, cardiomyopathy, asymptomatic ventricular tachycardia, tachycardia with bigeminy, atrioventricular block and fainting, myocardial infarction; rarely – heart failure; very rarely* – atrial fibrillation, supraventricular tachycardia, shock.
From the respiratory system: rarely* – shortness of breath, pleural effusion, respiratory failure, interstitial pneumonia, pulmonary fibrosis, pulmonary embolism; very rarely* – cough.
From the gastrointestinal tract: very often – nausea, vomiting, diarrhea, mucositis; rarely* – intestinal obstruction, intestinal perforation, ischemic colitis, pancreatitis; very rarely* – thrombosis of the mesenteric artery, pseudomembranous colitis, neutropenic colitis, esophagitis, constipation, ascites, anorexia.
From the liver and biliary tract: very rarely* – hepatonecrosis (fatal), hepatic encephalopathy (fatal).
From the organ of vision: very rarely* – reversible damage to the optic nerve and/or visual impairment (atrial fibrillation or ocular migraine); frequency unknown* – macular edema, photopsia, destruction of the vitreous body of the eye.
From the organ of hearing: very rarely* – hearing loss, tinnitus, vertigo (vestibular vertigo), ototoxicity.
From the skin and subcutaneous tissues: very often – alopecia; often – temporary minor changes in the skin and nails; rarely* – itching, rash, erythema, phlebitis, inflammation of subcutaneous fatty tissue, skin exfoliation, skin necrosis and fibrosis, skin lesions resembling the effects of radiation therapy; very rarely* – Stevens-Johnson syndrome, epidermal necrolysis, exudative erythema multiforme, exfoliative dermatitis, urticaria, onycholysis; frequency unknown* – scleroderma, cutaneous lupus erythematosus, palmoplantar erythrodysesthesia syndrome.
From the musculoskeletal system: very often – arthralgia, myalgia; frequency unknown* – systemic lupus erythematosus.
Local reactions: often – local swelling, pain, erythema, induration.
From laboratory parameters: often – increased activity of aspartate aminotransfer (AST), increased activity of alkaline phosphatase; infrequently – increased bilirubin concentration; rarely* – increased serum creatinine concentration.
Other: very often – secondary infections (in isolated cases – fatal); infrequently – septic shock; rarely* – pneumonia, sepsis, peritonitis, asthenia, general malaise, fever, dehydration, peripheral edema; frequency unknown* – tumor lysis syndrome.
Side effects with combination therapy:
Paclitaxel-Teva + cisplatin for 1st line treatment of ovarian cancer
The incidence and severity of neurotoxicity, arthralgia/myalgia and hypersensitivity are higher compared to cyclophosphamide and cisplatin therapy. On the contrary, manifestations of myelosuppression are observed less frequently and are less pronounced than with the use of cyclophosphamide and cisplatin.
Manifestations of severe neurotoxicity when used in combination with cisplatin at a dose of 75 mg/m2 are observed less frequently when using Paclitaxel-Teva at a dose of 135 mg/m2 as a 24-hour infusion than when administered at a dose of 175 mg/ml2 as a 3-hour infusion.
Paclitaxel-Teva + trastuzumab for the treatment of breast cancer
When using Paclitaxel-Teva in combination with trastuzumab for first-line treatment of metastatic breast cancer, the following side effects were observed more often than with Paclitaxel-Teva monotherapy: heart failure, infections, chills, fever, cough, rash, arthralgia, tachycardia, diarrhea, increased blood pressure, nosebleeds, acne, herpes rashes, accidental injuries, insomnia, rhinitis, sinusitis, reactions at the injection site.
The use of Paclitaxel-Teva in combination with trastuzumam in 2nd line therapy (after anthracycline drugs) led to an increase in the frequency and severity of cardiac events (in rare cases, fatal) compared with Paclitaxel-Teva monotherapy. In most cases, side effects were reversible after appropriate treatment.
Paclitaxel-Teva + doxorubicin for the treatment of breast cancer
Cases of congestive heart failure have been reported in patients who have not previously received chemotherapy. In patients who had previously received courses of chemotherapy, especially with the use of anthracyclines, cardiac dysfunction, a decrease in left ventricular ejection fraction, and insufficiency of ventricular function were often observed. In rare cases, myocardial infarction has been reported.
Paclitaxel-Teva + radiation therapy
Cases of radiation pneumonitis have been reported in patients who were simultaneously prescribed Paclitaxel-Teva and radiation therapy.
*Note: Post-marketing data on side effects are indicated with an asterisk.
Interaction
Interaction
Cisplatin
When paclitaxel is recommended for first-line chemotherapy for ovarian cancer, the drug must be administered before cisplatin. In this case, the safety profile of paclitaxel does not differ from that of monotherapy. When paclitaxel is administered after cisplatin, myelosuppression is more pronounced, and paclitaxel clearance is 20% lower than when cisplatin is administered after paclitaxel.
Doxorubicin
When using paclitaxel in combination with doxorubicin, the concentration of doxorubicin and its active metabolite, doxorubicinol, in the blood serum may increase. Side effects such as neutropenia and stomatitis are more pronounced when paclitaxel is used before doxorubicin is administered, as well as when the infusion is longer than recommended.
Substrates, inducers and inhibitors of CYP2C8 and CYP3A4 isoenzymes
Paclitaxel is metabolized by the CYP2C8 and CYP3A4 isoenzymes, so caution should be exercised when using paclitaxel during treatment with substrates (for example, midazolam, buspirone, felodipine, lovastatin, eletripan, sildenafil, simvastatin, triazolam, repaglinide and rosiglitazone), inducers (for example, rifampicin, carbamazepine, phenytoin, efavirenz, nevirapine) or inhibitors (for example, erythromycin, fluoxetine, gemfibrozil, ketoconazole, ritonavir, indinavir, nelfinavir) of these isoenzymes.
The results of studies of the pharmacokinetics of paclitaxel in patients with Kaposi’s sarcoma who received concomitant therapy with several drugs indicate a significant decrease in the systemic clearance of paclitaxel with simultaneous use of nelfinavir and ritonavir, but not indinavir. There is insufficient information regarding the interaction of paclitaxel with other protease inhibitors. Therefore, paclitaxel should be administered with caution to patients receiving concomitant therapy with protease inhibitors.
Other interactions
An increased risk of developing fatal systemic vaccine disease may occur when administered concomitantly with live vaccines. The use of live vaccines in immunosuppressed patients is not recommended.
Overdose
Overdose
Symptoms: suppression of bone marrow function, peripheral neuropathy, mucositis.
Treatment: symptomatic. There is no known antidote to paclitaxel.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C in the original packaging (pack).
Keep out of the reach of children!
Shelf life
Shelf life
2 years.
Do not use after expiration date.
Manufacturer
Manufacturer
Farmahemi B.V., Netherlands
Additional information
| Shelf life | 2 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ° C in the original package (pack). Keep out of reach of children! |
| Manufacturer | Pharmahemi B.V., The Netherlands |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Pharmahemi B.V. |
Other forms…
Related products
Buy Paclitaxel-Teva, 6 mg/ml 50 ml with delivery to USA, UK, Europe and over 120 other countries.