No products in the cart.
Description
- Ovarian cancer (first-line therapy in combination with platinum drugs and second-line therapy for metastases after standard therapy with no positive result);
- Breast cancer (as first- and second-line therapy as well as adjuvant treatment);
- Kaposi’soma in AIDS patients (second-line therapy, after ineffective therapy with liposomal anthracyclines).
.
Indications
Indications
Ovarian cancer (first-line therapy in combination with platinum drugs and second-line therapy for metastases after standard therapy that did not produce a positive result);
breast cancer (as first and second line therapy, as well as adjuvant treatment);
non-small cell lung cancer (first-line therapy for patients who are not planned for surgery and/or radiation therapy /in combination with cisplatin/);
Kaposi’s sarcoma in patients with AIDS (second-line therapy, after ineffective therapy with liposomal anthracyclines).
Special instructions
Special instructions
The use of Paclitaxel-Ebeve should be under the supervision of a physician experienced in working with anticancer chemotherapy drugs.
If severe hypersensitivity reactions develop, the administration of Paclitaxel-Ebeve should be stopped immediately and symptomatic therapy should be started, and the drug should not be re-administered.
If Paclitaxel-Ebeve is used in combination with cisplatin, Paclitaxel-Ebeve should be administered first followed by cisplatin.
When working with Paclitaxel-Ebeve, you must be careful (as when working with other cytotoxic substances), use gloves and avoid contact with the skin or mucous membranes. In case of contact with skin, wash thoroughly with soap and water; In case of contact with eyes, use large amounts of water.
Control of laboratory parameters
During treatment, it is necessary to regularly monitor the peripheral blood picture, blood pressure, heart rate and number of respirations (especially during the first hour of infusion).
ECG monitoring should be carried out before starting therapy and regularly during treatment.
If AV conduction disturbances develop during repeated administrations, continuous ECG monitoring is necessary.
Use in pediatrics
The safety and effectiveness of Paclitaxel-Ebeve in children has not been established. Use in pediatrics is contraindicated.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Due to the likelihood of side effects such as headache, dizziness, drowsiness, during the treatment period, patients should refrain from engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Precautions for handling and disposal of unused drug
Caution must be exercised when working with Paclitaxel-Ebeve. The drug should be diluted under aseptic conditions in a specially designated room. This should be done by trained personnel. It is necessary to take all measures to prevent the paclitaxel solution from coming into contact with the skin and mucous membranes, in particular the use of protective clothing (gown, cap, mask, goggles and disposable gloves). Shortness of breath, chest pain, a burning sensation in the throat, and nausea have been reported when inhaling vapors or spray solutions of paclitaxel.
If paclitaxel comes into contact with the skin or mucous membranes, rinse thoroughly with soap and water or (eyes) with plenty of water.
The drug should not be frozen, as this may cause sediment to form. This precipitate usually dissolves when the vial is warmed to room temperature (25°C). If the solution in a previously frozen vial remains cloudy or there is an insoluble precipitate in it, the drug cannot be used and such a vial must be destroyed. The prepared solution for infusion does not need protection from light.
Residues of the drug and all instruments and materials used to prepare the infusion solution and administer Paclitaxel-Ebeve should be disposed of in accordance with standard hospital cytotoxic waste disposal procedures, taking into account applicable hazardous waste disposal regulations.
Active ingredient
Active ingredient
Paclitaxel
Composition
Composition
1 ml contains:
Active ingredients:
paclitaxel 6 mg.
Excipients:
macrogol glyceryl ricinoleate (polyoxyethylated castor oil) – 522.396 mg,
ethanol – 401.664 mg.
The bottle contains 16.7 ml of concentrate.
There is 1 bottle in a cardboard package.
Contraindications
Contraindications
Hypersensitivity to the components of the drug;
hypersensitivity to other drugs, the dosage form of which includes polyoxyethylene castor oil;
initial neutrophil count less than 1500/μl in patients with solid tumors;
the initial (or registered during treatment) neutrophil content is less than 1000/μl for Kaposi’s sarcoma in patients with AIDS;
pregnancy;
lactation (breastfeeding);
children’s age (safety and effectiveness have not been established).
With caution: used in patients with suppression of bone marrow hematopoiesis (including after chemotherapy or radiation therapy), liver failure, acute infectious diseases (including herpes zoster, chicken pox, herpes), severe ischemic heart disease, with a history of myocardial infarction, and arrhythmia.
Side Effects
Side Effects
The frequency and severity of side effects are dose-dependent.
Determination of the frequency of side effects:
very often – > 10%;
often – from 1 to 10%;
infrequently – from 0.1% to 1%;
rarely – from 0.01 to 0.1%;
very rarely – less than 0.01%.
From the hematopoietic system: very often – myelosuppression, neutropenia, thrombocytopenia, anemia, leukopenia, bleeding; rarely – febrile neutropenia; very rarely – acute myeloid leukemia, myelodysplastic syndrome.
From the nervous system: very often – neurotoxic effects (mainly peripheral neuropathy), paresthesia; rarely – motor neuropathy (moderate weakness of the distal muscles, difficulty performing precise movements); very rarely – autonomic neuropathy (leading to paralytic ileus and orthostatic hypotension), grand mal seizures, convulsions, encephalopathy, dizziness, headache, confusion, ataxia.
From the cardiovascular system: often – bradycardia, decreased blood pressure; uncommon – cardiomyopathy, asymptomatic ventricular tachycardia, AV block, fainting, increased blood pressure, myocardial infarction, vascular thrombosis, thrombophlebitis; very rare – atrial fibrillation, supraventricular tachycardia, shock.
From the senses: very rarely – damage to the optic nerve and/or visual impairment (atrial fibrillation), hearing loss, tinnitus, dizziness.
From the respiratory system: rarely – shortness of breath, pleural effusion, interstitial pneumonia, pulmonary fibrosis, pulmonary embolism, respiratory failure, radiation pneumonitis in patients simultaneously undergoing radiation therapy; very rare – cough.
From the digestive system: very common – nausea, vomiting, diarrhea, inflammation of the mucous membranes; rarely – pancreatitis, intestinal perforation, ischemic colitis; very rarely – anorexia, constipation, mesenteric thrombosis, pseudomembranous colitis, esophagitis, ascites, neutropenic colitis, liver necrosis, hepatic encephalopathy (there are isolated reports of death).
From the skin and skin appendages: very often – alopecia; often – transient slight changes in nails and skin (pigmentation disorders, discoloration of the nail bed); rarely – itching of the skin, rashes, erythema; very rarely – Stevens-Johnson syndrome (ulceration of the mucous membrane of the mouth, throat, eyes, genitals, other areas of the skin and mucous membranes), epidermal necrolysis, erythema multiforme, exfoliative dermatitis, urticaria, onycholysis.
From the musculoskeletal system: very often – arthralgia, myalgia.
From the immune system: very common – infections (mainly of the urinary tract and upper respiratory tract); uncommon – serious hypersensitivity reactions requiring therapeutic measures (namely, decreased blood pressure, angioedema, respiratory distress syndrome, generalized urticaria, chills, back pain, chest pain, tachycardia, abdominal pain, pain in the extremities, severe sweating, increased blood pressure); rarely – anaphylatoid reactions.
From the laboratory parameters: often – an increase in the activity of liver transaminases, an increase in the concentration of alkaline phosphatase, bilirubin, creatinine in the blood serum.
Local reactions: often – pain, localized swelling, erythema, induration and pigmentation of the skin at the injection site; extravasation can cause inflammation and necrosis of the subcutaneous tissue.
Other: rarely – asthenia, fever, dehydration, general weakness.
Interaction
Interaction
Cisplatin reduces the overall clearance of paclitaxel by 20%, therefore, in combination chemotherapy, paclitaxel must be administered before cisplatin. More pronounced myelosuppression is observed when paclitaxel is administered after cisplatin. With combination chemotherapy (paclitaxel and cisplatin), the risk of developing renal failure is higher than with cisplatin monotherapy.
Co-administration with cimetidine, ranitidine, dexamethasone or diphenhydramine does not affect the binding of paclitaxel to plasma proteins.
Since the elimination of doxorubicin and its active metabolites may decrease when the time interval between administrations of paclitaxel and doxorubicin is shortened, paclitaxel should be administered 24 hours after doxorubicin.
Information on the potential interaction of paclitaxel with inhibitors and inducers of cytochrome P450 isoenzymes (in particular the CYP3A4 isoenzyme) is limited, so caution is required when using inhibitors (for example, erythromycin, fluoxetine, gemfibrozil) or inducers (for example, rifampicin, carbamazepine, phenytoin, phenobarbital) of cytochrome isoenzymes P450.
Microsomal oxidation inhibitors (including ketoconazole, cimetidine, verapamil, diazepam, quinidine, cyclosporine) inhibit the metabolism of paclitaxel. However, it is known that when ketoconazole and paclitaxel are taken simultaneously, the elimination of the latter does not slow down, so both drugs can be used without dose adjustment.
With simultaneous use of paclitaxel and nelfinavir or ritonavir (but not indinavir), the systemic clearance of paclitaxel is significantly reduced. There is insufficient information on the interactions between paclitaxel and other protease inhibitors when used concomitantly.
Polyoxyethylated castor oil, which is part of paclitaxel, can cause di-(2-hexyl) phthalate (DEHP) to be extracted from plasticized PVC containers, and the degree of DEHP leaching increases with increasing solution concentration and time. Therefore, when preparing, storing and administering Paclitaxel-Ebeve, you should use equipment that does not contain PVC parts.
Overdose
Overdose
Symptoms: bone marrow suppression, peripheral neuropathy, inflammation and ulceration of the mucous membranes.
Treatment: symptomatic. There is no known antidote to paclitaxel.
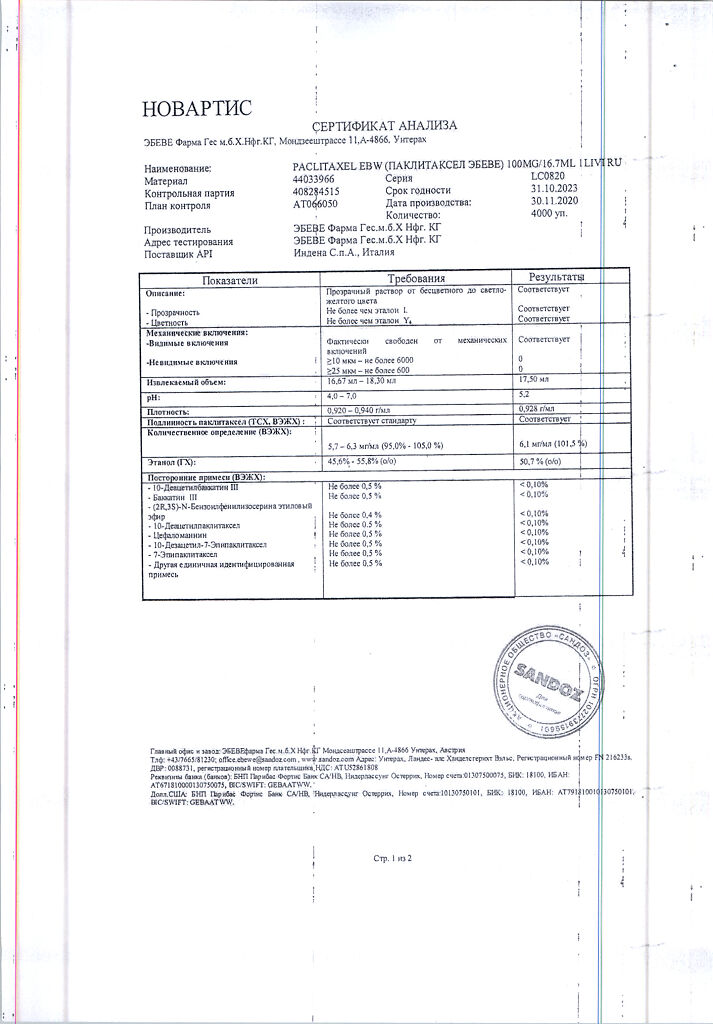
Storage conditions
Storage conditions
Store out of reach of children, protected from light at a temperature not exceeding 25°C.
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Ebewe Pharma, Austria
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store out of the reach of children, protected from light at a temperature not exceeding 25°C. |
| Manufacturer | Abeve Pharma, Austria |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Abeve Pharma |
Other forms…
Related products
Buy Paclitaxel-Ebeve, 6 mg/ml 16.7 ml with delivery to USA, UK, Europe and over 120 other countries.