No products in the cart.
Description
Pharmacodynamics
Oxaliplatin is an anticancer drug belonging to a new class of platinum derivatives in which the platinum atom forms a complex with oxalate and 1,2-diaminocyclohexane. Oxaliplatin exhibits a wide spectrum of cytotoxic action. It also shows activity in vitro and in vivo on various cisplatin-resistant tumor models. In combination with 5-fluorouracil a synergistic cytotoxic effect is observed.
The study of the mechanism of action of oxaliplatin supports the hypothesis that biotransformed, aqueous derivatives of oxaliplatin interact with DNA by formation of inter- and intrathecal bridges suppresses DNA synthesis, which leads to cytotoxicity and antitumor effect.
Pharmacokinetics
In vivo oxaliplatin undergoes active biotransformation and is not detected in plasma by the end of 2 hours after administration at a dose of 130 mg/sq.m, with 15% of the administered platinum being in the blood and the remaining 85% rapidly distributed to the tissues or excreted by the kidneys. Platinum is bound to plasma albumin and excreted in the urine within the first 48 hours.
By day 5, about 54% of the total dose is found in the urine and less than 3% in the feces. In renal insufficiency there is a significant decrease in clearance of oxaliplatin from 17.6 l/hour to 9.95 l/hour. The effect of severe renal failure on platinum clearance has not been studied.
Indications
Indications
Adjuvant therapy for colorectal cancer stage III (Duke C) after radical resection of the primary tumor in combination with 5-fluorouracil and folinic acid;
disseminated colorectal cancer (as monotherapy or combination therapy in combination with 5-fluorouracil and folinic acid).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Oxaliplatin is an antitumor drug belonging to a new class of platinum derivatives in which the platinum atom forms a complex with oxalate and 1,2-diaminocyclohexane. Oxaliplatin exhibits a wide range of cytotoxic effects. It also exhibits activity in vitro and in vivo in various cisplatin-resistant tumor models. In combination with 5-fluorouracil, a synergistic cytotoxic effect is observed.
Studying the mechanism of action of oxaliplatin confirms the hypothesis that biotransformed, aqueous derivatives of oxaliplatin, interacting with DNA by forming inter- and intrastrand bridges, suppress DNA synthesis, which leads to cytotoxicity and an antitumor effect.
Pharmacokinetics
In vivo, oxaliplatin undergoes active biotransformation and is not detected in plasma by the end of 2 hours after administration at a dose of 130 mg/m2, while 15% of the administered platinum is in the blood, and the remaining 85% is quickly distributed to tissues or excreted by the kidneys. Platinum binds to plasma albumin and is excreted in the urine within the first 48 hours.
By day 5, about 54% of the total dose is found in the urine and less than 3% in the feces. In renal failure, there is a significant decrease in oxaliplatin clearance from 17.6 l/hour to 9.95 l/hour. The effect of severe renal impairment on platinum clearance has not been studied.
Special instructions
Special instructions
Treatment with Oxaliplatin medac should be carried out under the supervision of a physician experienced in the use of cytotoxic drugs. Constant monitoring of possible toxic effects during oxaliplatin therapy is mandatory.
Regularly (once a week), as well as before each administration of the drug Oxaliplatin medac, the formed elements of peripheral blood and indicators of kidney and liver function should be monitored.
Before starting each cycle of therapy with Oxaliplatin medac, a neurological examination should be performed to identify signs of neurotoxicity.
Patients should be informed of the possibility of persistent symptoms of peripheral sensory neuropathy after completion of treatment. Localized moderate paresthesia with functional impairment can last up to 3 years after the end of treatment according to the adjuvant use of the drug.
If symptoms such as dry cough, dyspnea, wheezing or pulmonary infiltrates are detected on X-ray examination, treatment with Oxliplatin medac should be suspended until the presence of interstitial pneumonitis is ruled out.
Symptoms such as dehydration, paralytic ileus, intestinal obstruction, hypokalemia, metabolic acidosis and renal failure may be due to severe diarrhea or vomiting, especially when Oxaliplatin medac is used in combination with 5-fluorouracil.
Patients with a history of allergic reactions to other platinum compounds should be monitored for allergic symptoms. In the event of an anaphylactic-like reaction to oxaliplatin, the infusion should be interrupted immediately and appropriate symptomatic treatment should be instituted. Further use of the drug Oxaliplatin medac in case of allergic reactions is contraindicated. If liver dysfunction or portal hypertension occurs that is not due to liver metastases, the possible presence of drug-induced hepatovascular disorders, which are observed very rarely, should be considered.
In case of extravasation, the infusion should be stopped immediately and local symptomatic treatment should be started. The remaining dose of the drug should be injected into another vein. Women and men should use reliable methods of contraception during treatment and for 6 months after the end of oxaliplatin therapy. When using Oxaliplatin medac, all usual instructions for the use of cytotoxic drugs must be followed. If the lyophilisate or solution of the drug Oxaliplatin medac gets on the skin or mucous membranes, they should be immediately and thoroughly rinsed with water.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Not studied. However, the use of oxaliplatin increases the risk of dizziness, nausea, vomiting, and other neurological symptoms that affect the speed of reaction and, thus, reduce the ability to drive a car and use machinery.
Active ingredient
Active ingredient
Oxaliplatin
Composition
Composition
1 bottle contains:
Active ingredients:
oxaliplatin 150 mg.
Excipients:
lactose monohydrate.
The bottle contains 150 mg of lyophilisate.
There is 1 bottle in a cardboard package.
Pregnancy
Pregnancy
Contraindicated during pregnancy and breastfeeding.
Contraindications
Contraindications
Hypersensitivity to oxaliplatin or other components of the drug;
myelosuppression (neutrophil count less than 2000/μl and/or platelet count less than 100,000/μl) before the start of the first course of treatment;
peripheral sensory neuropathy with functional impairment before the start of the first course of treatment;
severe renal dysfunction (creatinine clearance less than 30 ml/min);
pregnancy;
breastfeeding period.
Side Effects
Side Effects
The most common side effects observed with oxaliplatin, including in combination with 5-fluorouracil/folinic acid, were gastrointestinal reactions (diarrhea, nausea, vomiting, mucositis), hematological reactions (neutropenia, thrombocytopenia) and neurological reactions (acute and cumulative dose-dependent peripheral sensory neuropathy). Overall, these side effects were more frequent and severe with the combination of oxaliplatin with 5-fluorouracil/folinic acid compared with 5-fluorouracil and folinic acid alone.
The frequency of adverse reactions listed below is presented in accordance with the following gradation:
very often (> 1/10);
often (> 1/100, < 1/10);
uncommon (> 1/1000, < 1/100);
rare (> 1/10000, < 1/1000);
very rare (<1/10000), including isolated reports.
From the hematopoietic system: very often – anemia, leukopenia, neutropenia, thrombocytopenia, lymphopenia; often – febrile neutropenia (including grade 3-4), sepsis due to neutropenia; rarely – hemolytic anemia, immune thrombocytopenia.
From the digestive system: very often – nausea, vomiting, diarrhea, stomatitis, mucositis, pain in the stomach, constipation, loss of appetite; often – dyspepsia, gastroesophageal reflux, hiccups; infrequently – intestinal obstruction; rarely – colitis, including cases of pseudomembranous colitis.
From the central and peripheral nervous system: very often – peripheral neurosensory neuropathy, sensitivity disorders, headache, asthenia; often – dizziness, meningism, depression, insomnia; infrequently – increased nervousness; rarely – dysarthria.
Neurotoxicity is a dose-limiting adverse effect. Symptoms of sensory neuropathy are often triggered by cold. The duration of these symptoms, which usually resolve between courses, increases depending on the total dose of oxaliplatin. Functional impairment, which is characterized by difficulty performing precise movements, is a possible consequence of sensory damage.
The risk of functional impairment for a total dose of about 850 mg/m2 (10 cycles) is about 10%, reaching 20% in the case of a total dose of 1020 mg/m2 (12 cycles). In most cases, neurological symptoms improve or disappear completely after stopping treatment. However, in 3% of patients 3 years after the end of treatment, either persistent localized paresthesia of moderate intensity (2.3%) or paresthesia affecting functional activity (0.5%) was observed.
During treatment with oxaliplatin, acute neurosensory manifestations were noted, which usually occurred within several hours after drug administration and were most often provoked by cold. They were characterized by transient paresthesia, dysesthesia or hypoesthesia, and rarely (1-2%) acute laryngopharyngeal dysesthesia syndrome.
The latter was manifested by a subjective feeling of dysphagia and shortness of breath without objective signs of respiratory distress syndrome (cyanosis or hypoxia), or laryngeal spasm or bronchospasm (without stridor or wheezing). Such phenomena as jaw spasm, tongue dysesthesia, dysarthria and a feeling of pressure in the chest were also observed. Typically, these symptoms were quickly relieved both without the use of drug therapy and with the administration of antihistamines and bronchodilators. Increasing the infusion time during subsequent cycles of oxaliplatin therapy can reduce the incidence of this syndrome.
From the musculoskeletal system: very often – back pain; often – arthralgia, bone pain.
From the respiratory system: very often – cough, shortness of breath; often – rhinitis, upper respiratory tract infections; rarely – pulmonary fibrosis.
From the cardiovascular system: often – chest pain, deep vein thrombophlebitis, pulmonary embolism.
From the urinary system: often – hematuria, dysuria.
From the skin and skin appendages: very often – alopecia, skin rashes; often – peeling of the skin of the palms and feet, erythematous rashes, increased sweating, nail disorders.
From the organs of vision and hearing: often – conjunctivitis, visual impairment; rarely – transient decrease in visual acuity, loss of visual fields, hearing loss, auditory neuritis.
Allergic reactions: rarely (when used as monotherapy) or often (in combination with 5-fluorouracil +/- calcium folinate), bronchospasm, angioedema, hypotension and anaphylactic shock may occur. Cases of allergic manifestations such as rash (especially urticaria), conjunctivitis or rhinitis have often been reported.
Local reactions: with extravasation of the drug – pain and inflammatory reactions at the injection site.
From the laboratory parameters: very often – increased levels of alkaline phosphatase, activity of liver enzymes, bilirubin content, lactate dehydrogenase, hypokalemia, disturbances in sodium and glucose levels in the blood serum; often – increased creatinine levels.
Other: very often – increased body temperature, increased fatigue, increased body weight, taste disturbances.
Interaction
Interaction
Pharmaceutically incompatible with alkaline solutions and solutions containing chlorine.
In cases where patients were given a single dose of 85 mg/m2 of oxaliplatin immediately before the administration of 5-fluorouracil, no change in the level of 5-fluorouracil was observed.
There was no noticeable change in the binding of oxaliplatin to plasma proteins in combined in vitro experiments with erythromycin, salicylates, granisetron, paclitaxel and sodium valproate.
Incompatibilities
do not use together with alkaline preparations or solutions (in particular, 5-fluorouracil, alkaline solutions, trometamol and folinic acid preparations containing trometamol as an excipient);
do not use saline solutions to dissolve the drug or dilute the drug solution (to prepare an infusion solution), do not mix with other drugs in the same container or in the infusion system;
do not use administration equipment containing aluminum (precipitate formation may occur and the activity of oxaliplatin may decrease).
Overdose
Overdose
Symptoms: increased described side effects. No antidote is known.
Treatment: hematological control and symptomatic therapy.
Storage conditions
Storage conditions
Store out of the reach of children and away from light at a temperature not exceeding 25 °C.
Shelf life
Shelf life
2.5 years.
Manufacturer
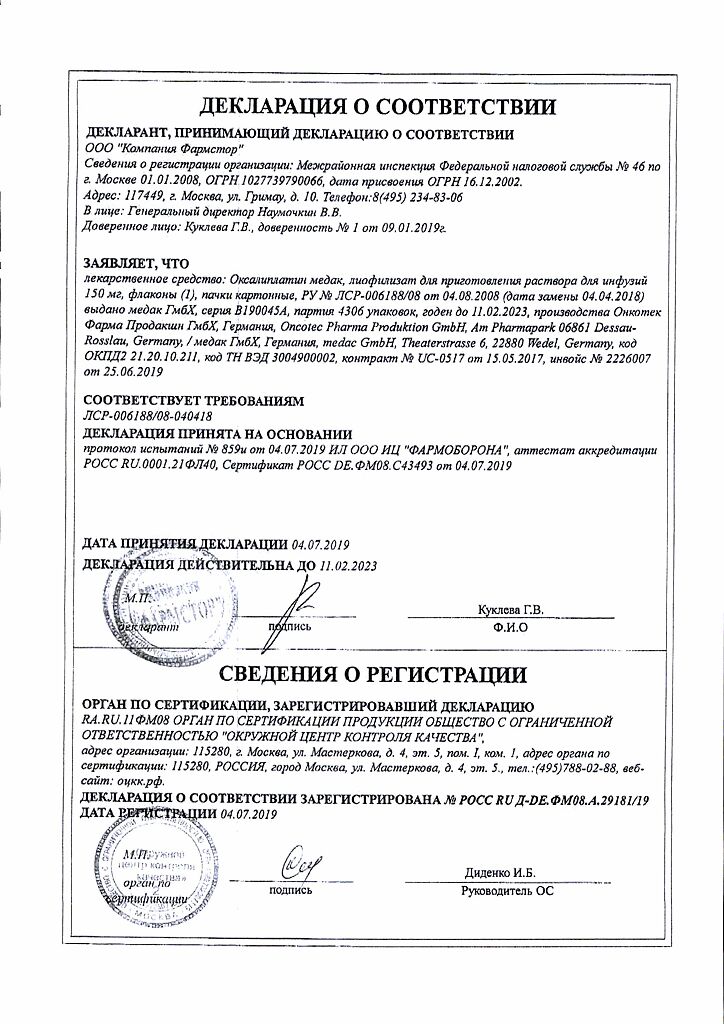
Manufacturer
Oncotech Pharma Production GmbH, Germany
Additional information
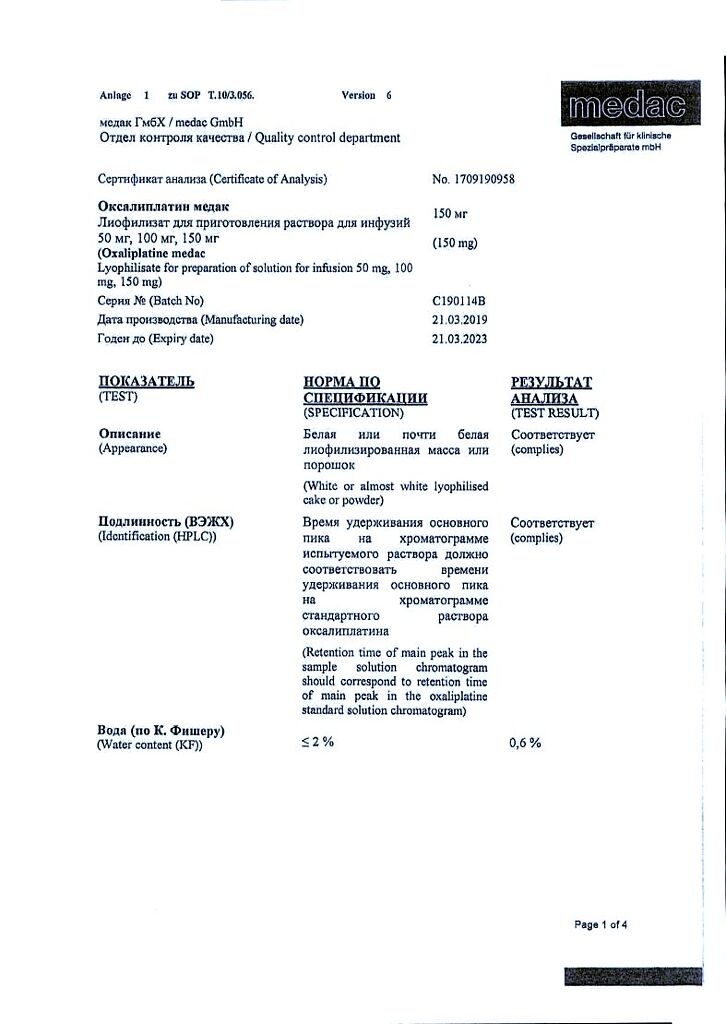
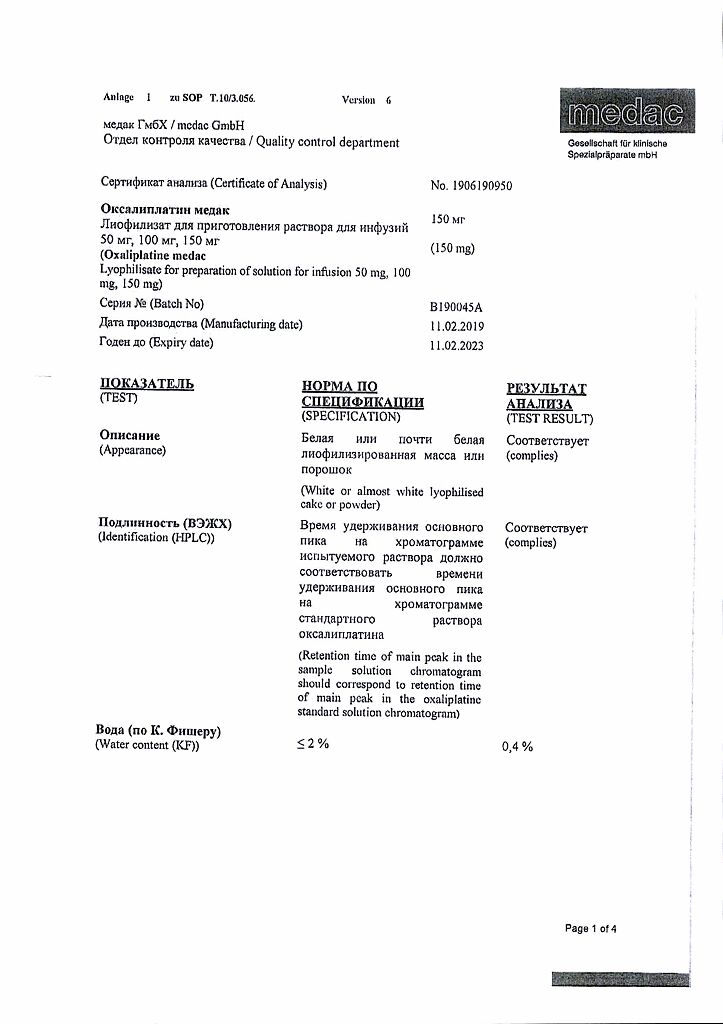
| Shelf life | 2.5 years. |
|---|---|
| Conditions of storage | Keep out of reach of children and out of the light at a temperature not exceeding 25 ° C. |
| Manufacturer | Onkotek Pharma Production GmbH, Germany |
| Medication form | lyophilizate |
| Brand | Onkotek Pharma Production GmbH |
Related products
Buy Oxaliplatin medac, lyophilizate 150 mg with delivery to USA, UK, Europe and over 120 other countries.