No products in the cart.
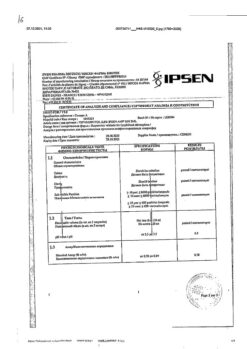
Ovestin, tablets 2 mg 30 pcs
€48.19 €40.16
Description
Pharmacotherapeutic group: Estrogens.
ATC code: G03CA04
Pharmacological properties
Pharmacodynamics
Ovestin® contains the natural female sex hormone estriol. Pre-menopausal and post-menopausal (natural or surgical) estriol is used to treat symptoms caused by estrogen deficiency.
Estriol has a selective effect primarily on the cervix, vagina, and vulva and is particularly effective for the treatment of urogenital symptoms caused by estrogen deficiency.
In cases of vaginal mucosal atrophy estriol causes increase of proliferation of vaginal and cervical epithelium, stimulates its blood supply, promotes restoration of epithelium, normal microflora and physiological pH of the vaginal environment, influences the quality and quantity of cervical mucus.
As a result the resistance of epithelial cells to infection and inflammation increases. Unlike other estrogens, estriol has a short-term effect, since it is retained in the nuclei of endometrial cells for a short time and endometrial proliferation should not be expected if the recommended dosing regimen is followed. Because of this, cyclic use of progestagens is not necessary, postmenopausal bleeding cancellation does not occur.
Pharmacokinetics
After oral administration, estriol is quickly and almost completely absorbed in the gastrointestinal tract. The maximum concentration of unconjugated estriol in plasma is reached within 1 hour after ingestion.
About 90% of estriol is bound to plasma albumin, and, unlike other estrogens, estriol almost does not bind to sex hormone-binding globulin (HSPG). The metabolism of estriol consists mainly of conjugation and deconjugation during the intestinal-hepatic circulation. Estriol, the end product of metabolism, is excreted mainly with the urine in conjugated form. Only a small portion (±2%) is excreted with the feces, mainly as unconjugated estriol.
Indications
Indications
Atrophy of the mucous membranes of the lower genitourinary tract due to estrogen deficiency, in particular to treat symptoms such as dyspareunia, vaginal dryness and itching, to prevent recurrent infections of the vagina and lower genitourinary tract; for the treatment of urinary disorders (for example, frequency, dysuria) and moderate urinary incontinence;
Pre- and postoperative treatment during vaginal surgery in the postmenopausal period;
Menopausal disorders such as hot flashes and night sweats;
As an auxiliary diagnostic tool when obtaining an atrophic picture of a cervical smear;
Infertility caused by cervical factor.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: Estrogens.
ATX code: G03CA04
Pharmacological properties
Pharmacodynamics
Ovestin® contains the natural female sex hormone estriol. During premenopause and postmenopause (natural or surgical), estriol is used to treat symptoms caused by estrogen deficiency.
Estriol has a selective effect primarily on the cervix, vagina, vulva and is especially effective for the treatment of urogenital symptoms caused by estrogen deficiency.
In cases of atrophy of the vaginal mucosa, estriol causes increased proliferation of the epithelium of the vagina and cervix, stimulates its blood supply, helps restore the epithelium, normal microflora and physiological pH of the vaginal environment, and affects the quality and quantity of cervical mucus.
As a result, the resistance of epithelial cells to infection and inflammation increases. Unlike other estrogens, estriol has a short-term effect, since it is retained for a short time in the nuclei of endometrial cells and, if the recommended dosage regimen is followed, endometrial proliferation should not be expected. In this regard, cyclic use of progestogens is not necessary; postmenopausal withdrawal bleeding does not occur.
Pharmacokinetics
After oral administration, estriol is quickly and almost completely absorbed from the gastrointestinal tract. The maximum concentration of unconjugated estriol in plasma is achieved within 1 hour after administration.
About 90% of estriol is bound to plasma albumin, and, unlike other estrogens, estriol has almost no binding to sex hormone binding globulin (SHBG). The metabolism of estriol consists mainly of conjugation and deconjugation during the enterohepatic circulation. Estriol, the end product of metabolism, is excreted mainly in the urine in conjugated form. Only a small part (2%) is excreted in the feces, mainly in the form of unconjugated estriol.
Special instructions
Special instructions
To treat menopausal symptoms, HRT should only be started for symptoms that adversely affect quality of life. In all cases, a thorough assessment of the risks and benefits of treatment should be carried out at least once a year and HRT should be continued only as long as the benefits outweigh the risks.
There is limited evidence of the risk development of HRT when treating premature menopause. Because younger women have a lower absolute risk, their benefit-risk ratio is more favorable than that of older women.
Medical examination/observation
Before starting or resuming HRT, a detailed individual and family history should be obtained. Based on the obtained medical history, contraindications and warnings for use, it is necessary to conduct a clinical examination (including examination of the pelvic organs and mammary glands).
During treatment, it is recommended to conduct periodic medical examinations, the frequency and nature of which vary from person to person. Women should be informed about the need to tell their doctor about changes in the mammary glands (see section “Breast cancer” below). Investigations, including appropriate imaging modalities such as mammography, should be performed in accordance with currently accepted screening standards and on a case-by-case basis.
Reasons for immediate discontinuation of therapy
Therapy should be discontinued if a contraindication is identified and if the following conditions occur:
Jaundice or deterioration of liver function.
Significant increase in blood pressure.
The occurrence of a migraine-type headache.
Pregnancy.
Endometrial hyperplasia and carcinoma
To prevent endometrial stimulation, the daily dose of the drug should not exceed 1 suppository (0.5 mg estriol). This maximum dose should not be used for more than 4 weeks. In addition, one epidemiological study found that long-term use of low-dose estriol, administered orally but not intravaginally, may increase the risk of endometrial cancer. The risk increases with the duration of treatment and returns to baseline values one year after discontinuation of the drug. Basically, the risk of minimally invasive and well-differentiated tumors increases. Vaginal bleeding in all cases requires examination. The patient should be informed of the need to contact the attending physician if vaginal bleeding begins.
Breast cancer
Hormone replacement therapy (HRT) may increase mammographic density. This can make radiological detection of breast cancer more difficult. Clinical studies have shown that the likelihood of an increase in mammographic density is lower in women treated with estriol than in women treated with other estrogens.
Composite evidence suggests an increased risk of breast cancer in women receiving combination therapy with estrogens and progestogens and possibly estrogen monotherapy.
In women receiving combination therapy with estrogens and progestogens for more than 5 years, a 2-fold increase in the risk of breast cancer was noted.
With estrogen monotherapy, the increase in risk is significantly lower than when combined with progestogens.
The level of risk depends on the duration of HRT.
It is not known whether Ovestin® poses the same risk. A recent population-based case-control study of 3345 women with invasive breast cancer and 3454 controls showed that estriol use, unlike other estrogens, was not associated with an increased risk of breast cancer. It is therefore important that the risk of developing breast cancer is discussed with the patient and weighed against the known benefits of HRT.
Ovarian cancer
Ovarian cancer develops much less frequently than breast cancer. Long-term estrogen monotherapy (at least 5–10 years) was associated with a small increase in the risk of ovarian cancer. Some studies suggest that combined HRT may increase the risk of ovarian cancer in a similar or small way. It is not known whether the risk of long-term use of low-potency estrogens (such as Ovestin®) differs from that of monotherapy with other estrogens.
Venous thromboembolism
HRT is associated with an increased risk of venous thromboembolism (VTE), i.e. deep vein thrombosis or pulmonary embolism, 1.3 – 3 times. The likelihood of developing VTE is higher during the first year of HRT use than at a later date. It is not known whether Ovestin® has the same risk.
In patients with confirmed thrombophilia, the risk of VTE is high, and HRT may further increase this risk. In this regard, HRT is contraindicated for such women (see section “Contraindications”).
Commonly recognized risk factors for VTE include estrogen use, older age, major surgery, prolonged immobilization, obesity (BMI > 30 kg/m2), pregnancy/puerperium, systemic lupus erythematosus, and cancer. There is no consensus regarding the possible role of varicose veins in the development of VTE. After any surgical intervention, VTE prophylaxis is necessary. If prolonged immobilization is associated with elective surgery, it is necessary to temporarily discontinue HRT 4-6 weeks before surgery. Treatment should be resumed after the woman begins to walk.
For women already receiving anticoagulant treatment, careful consideration of the benefit-risk balance of HRT is required.
If Ovestin® is prescribed as “pre- and postoperative treatment…”, the issue of thrombosis prophylaxis should be considered.
In the absence of a history of VTE, but in the presence of thrombosis at a young age in the patient’s closest relatives, she can be offered a screening examination, having previously discussed all its limitations (screening can detect only a number of thrombophilic disorders). If a thrombophilic defect is detected that does not correspond to the disease in relatives, or if a “severe” defect is detected (for example, deficiency of antithrombin, protein S or protein C, or a combination of these defects), HRT is contraindicated.
If VTE develops after starting treatment with Ovestin®, then treatment with the drug must be discontinued. Patients should be informed to seek immediate medical attention if they experience possible signs of thromboembolism (eg, painful leg swelling, sudden chest pain, shortness of breath).
Coronary heart disease (CHD)
Randomized controlled trials did not provide results that would indicate that combination therapy with estrogens and progestogens and estrogen monotherapy can prevent the development of myocardial infarction in women with and without coronary artery disease.
Estrogen monotherapy:
According to randomized controlled trials, the risk of coronary heart disease in women with a removed uterus does not increase with estrogen monotherapy.
The risk of coronary heart disease increases slightly with combined HRT with estrogens and progestogens in patients over 60 years of age.
Ischemic stroke
Combination therapy with estrogens and progestogens and monotherapy with estrogens are associated with a 1.5-fold increase in the risk of ischemic stroke. The relative risk does not change with age or time after menopause. However, the baseline risk of stroke is highly dependent on age, and the overall risk of stroke with HRT increases with age. The risk of hemorrhagic stroke does not increase with HRT.
Other states
Estrogens can cause fluid retention and therefore patients with impaired renal function and cardiovascular insufficiency should be closely monitored.
Estriol is a weak gonadotropin antagonist and has no other significant effects on the endocrine system.
Cognitive function does not improve with HRT. Evidence has been obtained of an increased risk of developing dementia in women who began using combination therapy or monotherapy in a continuous regimen after 65 years.
Impact on the ability to drive a car and other mechanisms
There was no effect of the drug Ovestin® on concentration and attention.
Active ingredient
Active ingredient
Estriol
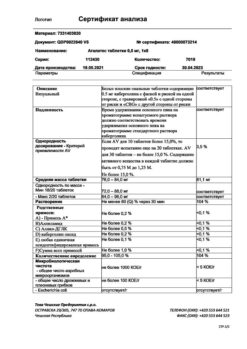
Composition
Composition
Active substance:
estriol 2.0 mg;
Excipients:
colloidal silicon dioxide 0.75 mg,
potato starch 10.0 mg,
magnesium stearate 0.50 mg,
povidone 1.0 mg,
lactose monohydrate up to 100.0 mg (about 87.75 mg), distilled water q.s.*
* – removed during production.
Contraindications
Contraindications
identified or suspected estrogen-dependent tumors (breast cancer, endometrial cancer);
vaginal bleeding of unknown etiology;
confirmed venous thromboembolism (deep vein thrombosis, pulmonary thromboembolism) within the last 2 years;
a history of venous thromboembolism or thrombosis, if anticoagulant therapy is not carried out;
diabetes mellitus with angiopathy;
sickle cell anemia;
Dubin-Johnson syndrome;
Rotor syndrome;
cerebrovascular accident;
pregnancy;
lactation period (breastfeeding);
hypersensitivity to the active and/or excipients of the drug.
The drug should be prescribed with caution in the following conditions:
familial hyperlipoproteinemia;
increased risk of thromboembolic complications;
systemic lupus erythematosus;
prolonged immobilization, serious surgical interventions;
severe liver disease;
history of gallbladder disease (especially cholelithiasis);
hepatic porphyria;
severe itching or cholestatic jaundice (including a history of previous pregnancy);
pancreatitis;
endometriosis;
leiomyoma;
bronchial asthma;
arterial hypertension;
hypercalcemia caused by bone metastases of breast cancer;
herpes during pregnancy;
epilepsy;
otosclerosis.
Side Effects
Side Effects
According to monitoring safety studies, the following adverse reactions exist:
From the digestive system: nausea.
From the side of water-electrolyte metabolism: fluid retention.
From the reproductive system:
– soreness and tension of the mammary glands;
– intermenstrual bloody spotting from the vagina;
– cervical hypersecretion.
Adverse reactions are usually transient and may also indicate an overdose of the drug. Other adverse reactions have been reported during estrogen monotherapy or combination therapy with estrogens and progestogens:
From the reproductive system: estrogen-dependent benign and malignant tumors, incl. endometrial cancer.
From the digestive system: gallbladder diseases.
From the skin: chloasma, erythema multiforme, erythema nodosum, vascular purpura.
From the central nervous system:
– headache;
– dementia when starting continuous HRT after 65 years.
There is data on the development of the risk of breast cancer, ovarian cancer, the risk of venous thromboembolism, the risk of coronary heart disease, and the risk of ischemic stroke.
Interaction
Interaction
There have been no cases of interaction between the drug Ovestin® and other drugs. At the same time, there is evidence of an increase in the pharmacological effect of glucocorticosteroids and lipid-lowering drugs when used together with estrogens. If necessary, the dose of glucocorticosteroids can be reduced.
The effects of male sex hormones, anticoagulants, antidepressants, diuretics, antihypertensive and hypoglycemic drugs may be weakened. Barbiturates, antiepileptic drugs (carbamazepine, phenytoin), antiretroviral drugs nevirapine and efavirenz, herbal preparations containing St. John’s wort (Hypericum perforatum), increase the metabolism of steroid hormones. Ritonavir and nelfinavir exhibit inducing properties when used simultaneously with steroid hormones.
From a clinical point of view
increased estrogen metabolism may lead to decreased effectiveness
7
the drug Ovestin® and changes in the nature of uterine bleeding.
Antibiotics (griseofulvin, ampicillin, rifampicin), medicines for
general anesthesia, narcotic analgesics, anxiolytics, antiepileptics
medicines, some antihypertensive drugs, ethanol
reduce the effectiveness of estrogens.
Folic acid and thyroid hormone preparations enhance the effect
estriol.
Estriol may alter the effectiveness of oral anticoagulants, increase
pharmacological effect of succinylcholine, theophylline, foleandomycin.
Overdose
Overdose
In case of overdose, nausea, vomiting and vaginal bleeding occur.
Treatment is symptomatic.
Storage conditions
Storage conditions
At temperatures from 2 °C to 30 °C in a dry place, protected from light. Keep out of the reach of children.
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Sindea Pharma S.L., Spain
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | From 2°C to 30°C in a dry, light-protected place. Keep out of reach of children. |
| Manufacturer | Sindea Pharma S.L., Spain |
| Medication form | pills |
| Brand | Sindea Pharma S.L. |
Other forms…
Related products
Buy Ovestin, tablets 2 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.