No products in the cart.
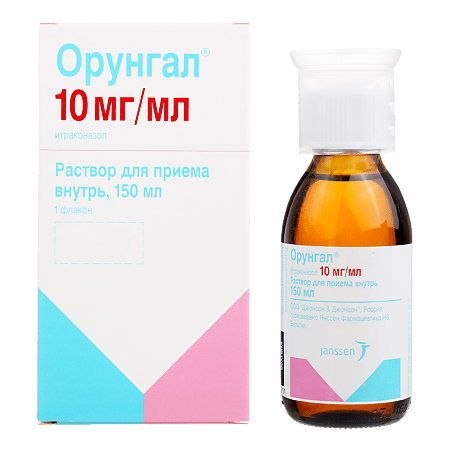
Orungal, 10 mg/ml 150 ml
€1.00
Out of stock
(E-mail when Stock is available)
Description
ORUNGAL is an antifungal.
Pharmacodynamics
Itraconazole inhibits the synthesis of ergosterol of the cell membrane of fungi, which determines the antifungal effect of the drug.
It is active against infections caused by fungi:
- dermatophytes (Trichophyton spp., Microsporum spp., Epidermophyton floccosum);
- dermato-like fungi and yeasts (Candida spp, including C. albicans, C. glabrata and C. krusei, Cryptococcus neoformans, Pityrosporum spp, Geotrichum spp.);
- Aspergillus spp.; Histoplasma spp.; Paracoccidioides brasiliensis; Sporothrix schenckii; Fonsecaea spp.; Cladosporium spp.; Blastomyces dermatitidis; Pseudallescheria boydii; Penicillium marneffei etc.
Candida glabrata and Candida tropicalis are the least sensitive Candida species to the action of itraconazole.
The main types of fungi whose development is not inhibited by itraconazole are Zygomycetes (Rhizopus spp., Rhizomucor spp., Mucor sp p. and Absidia spp.), Fusarium spp., Scedosporium spp. and Sclerosporium spp.
Pharmacokinetics
In general, itraconazole is well absorbed. C max in plasma is reached 2.5 h after taking the drug. Itraconazole is metabolized in the liver with the formation of a large number of metabolites. The main metabolite is hydroxyitraconazole, whose plasma concentrations are almost 2 times higher than the corresponding concentrations of itraconazole. Final T1/2 of itraconazole is 40 hours after repeated administration. In patients with renal and hepatic impairment T1/2 of itraconazole is slightly increased.
The pharmacokinetics of itraconazole is characterized by non-linearity, due to which accumulation in plasma is achieved with prolonged use. Equilibrium concentrations of itraconazole in plasma are reached after 15 days with Cmax value about 2 mcg/ml (at the use of 200 mg itraconazole once a day). Itraconazole clearance decreases at higher doses due to saturation of hepatic metabolism.
Itraconazole is rapidly absorbed after solution administration. Absolute bioavailability of itraconazole when taking the drug with food is about 55%, when taking the solution on an empty stomach the bioavailability of itraconazole increases by 30%.
Itraconazole penetrates well into tissues: concentrations in lungs, kidneys, liver, bones, stomach, spleen and muscles are 2-3 times higher than the corresponding concentrations in plasma. Ratio of itraconazole concentrations in brain tissue and plasma is approximately the same.
The drug concentration in keratinous tissues, especially in the skin, is about 4 times higher than the concentration in plasma.
The main metabolite is hydroxyitraconazole, which in vitro has antifungal activity comparable to that of itraconazole.
Concentrations of hydroxylated metabolite in plasma are almost 2 times higher than the corresponding concentrations of itraconazole.
As shown in in vitro studies, itraconazole is metabolized mainly with the participation of the enzyme CYP3A4.
About 35% of itraconazole in the form of inactive metabolites is excreted in the urine within a week and about 54% – in the feces. From 3 to 18% of the dose of the parent substance is excreted in the feces. Renal excretion of the parent substance is less than 0.03% of the dose.
Indications
Indications
Treatment of oral and/or esophageal candidiasis in HIV-positive and immunodeficient patients; prevention of systemic fungal infections in patients with malignant blood diseases or bone marrow transplant patients with a high probability of neutropenia (
Active ingredient
Active ingredient
Composition
Composition
1 ml. The solution contains:
Active substance:
itraconazole 10 mg;
Associates:
Hydroxypropyl-β-cyclodextrin;
Sorbitol 70% noncrystallizing solution;
sodium saccharinate;
propylene glycol;
Hydrochloric acid concentrated;
Sodium hydroxide;
Flavors (cherry, caramel);
Purified water.
How to take, the dosage
How to take, the dosage
In the mouth, on an empty stomach. Rinse your mouth with the solution and then swallow it. After that, you should not rinse your mouth with water.
Treatment of oral and/or esophageal candidiasis: 200 mg (2 measuring cups) daily in one or two doses for 1 week. If there is no positive effect after 1 week, treatment should be continued for another week.
Treatment of oral and/or esophageal candidiasis, in case of resistance to fluconazole: 200-400 mg (2-4 measuring cups) daily in 1-2 doses for 2 weeks. If there is no positive effect after 2 weeks, treatment should be continued for another 2 weeks.
Prevention of fungal infections: 5 mg/kg/day in 2 doses. The drug is started one week before treatment with cytostatics or one week after a bone marrow transplant. Orungal® administration is continued until neutrophil count is restored (at least 1000 cells/μL).
Interaction
Interaction
Medications affecting the absorption of itraconazole
Medications that reduce the acidity of the gastric contents reduce the absorption of itraconazole, which is associated with the solubility of the capsule shells.
Drugs affecting the metabolism of itraconazole
In studies it was found that when Orungal interacts with rifampicin, rifabutin and phenytoin the bioavailability of itraconazole and hydroxyitraconazole is significantly reduced, which leads to a significant reduction in the effectiveness of the drug. Concomitant use of itraconazole with these drugs, which are potential inducers of liver enzymes, is not recommended. Studies of interaction with other inducers of liver enzymes, such as carbamazepine, phenobarbital and isoniazid were not conducted, but similar results can be assumed.
As itraconazole is mainly metabolized by CYP3A4 isoenzyme, potential inhibitors of this enzyme (ritonavir, indinavir, clarithromycin and erythromycin) may increase the bioavailability of itraconazole.
The effect of itraconazole on the metabolism of other drugs
Itraconazole may inhibit the metabolism of drugs metabolized by CYP3A4 isoenzyme. This may result in enhancement or prolongation of their effects (including side effects). Before starting to take concomitant drugs, it is necessary to consult the attending physician about the metabolism pathway of this drug, indicated in the instructions for medical use. After discontinuation of treatment, plasma concentrations of itraconazole decrease gradually, depending on the dose and duration of treatment. This should be taken into account when assessing the inhibitory effect of itraconazole on the metabolism of concomitantly administered drugs.
In the course of treatment with Orungal it is not allowed to prescribe:
– terfenadine, astemizole, misolastin, cisapride, dofetilide, quinidine, pimozide, sertindole, levomethadone, the use of which together with Orungal may lead to an increase in plasma concentration of these substances, which in turn may cause QT interval increase and in rare cases – paroxysmal ventricular tachycardia type “pirouette” (torsade de pointes);
– oral midazolam and triazolam;
– CYP3A4 metabolizable HMG-CoA reductase inhibitors such as simvastatin and lovastatin;
– ergot alkaloid preparations such as dihydroergotamine, ergometrine, ergotamine and methylergometrine;
– Calcium channel blockers – in addition to a possible pharmacokinetic interaction related to the common metabolic pathway involving the CYP3A4 enzyme, calcium channel blockers have a negative inotropic effect, which may enhance the similar effect of itraconazole.
When concomitant administration with Orongal, plasma levels, effects, side effects of oral anticoagulants; HIV protease inhibitors (such as ritonavir, indinavir, saquinavir) should be monitored; some anticancer drugs (such as periwinkle pink alkaloids, busulfan, docetaxel, trimetrexate); calcium channel blockers metabolized by CYP3A4 isoenzyme (dihydropyridine and verapamil); some immunosuppressive drugs (such as cyclosporine, tacrolimus, sirolimus); some HMG-CoA reductase inhibitors metabolized by CYP3A4 enzyme, such as atorvastatin; some GKS, such as budesonide, dexamethasone and methylprednisolone and digoxin, carbamazepine, buspirone, alfentanil, alprazolam, brotizolam, midazolam (IV), rifabutin, methylprednisolone, ebastine, reboxetine, repaglinide, disopyramide, cilostazol, eletriptan, halofantrine. When concomitant use with Orungal, the dose of the above drugs should be reduced if necessary.
The interaction between itraconazole and zidovudine and fluvastatin has not been found.
Itraconazole has not been observed to affect the metabolism of ethinylestradiol and norethisetron.
In vitro studies have demonstrated no interaction due to competition for binding to plasma proteins between itraconazole and such drugs as imipramine, propranolol, diazepam, cimetidine, indomethacin, tolbutamide and sulfamethazine.
Special Instructions
Special Instructions
Women of childbearing age taking Orungal® should use adequate contraception for the duration of treatment until their first menstrual period after completion of treatment.
In an IV study of Orungal® in healthy volunteers, a transient asymptomatic decrease in left ventricular ejection fraction was observed that normalized before the next infusion of the drug.
The clinical significance of the findings for oral dosage forms is unknown.
Itraconazole has been found to have a negative inotropic effect. Caution should be exercised when concomitant administration of itraconazole and BCAAs, which may have the same effect. Cases of congestive heart failure associated with taking Orungal® have been reported. Orungal® should not be taken in patients with chronic heart failure or with a history of this disease, except in cases when the possible benefit significantly exceeds the potential risk. In individual assessment of the benefit-risk ratio such factors as severity of indications, dosage regimen and individual risk factors of congestive heart failure should be taken into account. Risk factors include the presence of diseases, such as CHD or heart valve lesions; obstructive pulmonary lesions; renal failure or other diseases accompanied by edema. Such patients should be informed about the signs and symptoms of congestive heart failure. Treatment should be performed with caution, and the patient should be monitored for the occurrence of symptoms of congestive heart failure. If symptoms occur, Orungal® should be discontinued.
In low gastric acidity: In this condition, the absorption of itraconazole from Orunhal® capsules is impaired. Patients taking antacids (e.g., aluminum hydroxide) should not use them until 2 hours after taking Orunhal® capsules.
Patients with achlorhydria or who use H2-histamine receptor blockers or proton pump inhibitors are recommended to take Orungal® capsules with cola.
In very rare cases, severe toxic liver damage, including cases of acute hepatic failure with fatal outcome, has developed with the use of Orungal®. In most cases this was observed in patients who already had liver disease, in patients with other severe diseases who received itraconazole therapy for systemic indications, as well as in patients who received other drugs with hepatotoxic effect. Some patients had no obvious risk factors for liver damage. Several such cases occurred in the first month of therapy, and some occurred in the first week of treatment.
In this regard, it is recommended to regularly monitor liver function in patients receiving itraconazole therapy. Patients should be warned to contact their physician immediately if symptoms suggestive of hepatitis occur, such as: anorexia, nausea, vomiting, weakness, abdominal pain, and darkened urine. In case of appearance of such symptoms it is necessary to stop therapy immediately and conduct liver function tests.
Patients with elevated liver enzymes or active liver disease or who have experienced toxic liver injury while taking other drugs should not be treated with Orungal® unless the expected benefit justifies the risk of liver damage. In these cases, liver enzyme levels should be monitored during treatment.
Hepatic disorders: Itraconazole is metabolized mainly in the liver. As the total T1/2 of itraconazole is slightly prolonged in patients with hepatic impairment, it is recommended to monitor the concentrations of itraconazole in plasma and to correct the dose of the drug, if necessary.
With impaired renal function: because in patients with renal impairment the total T1/2 of itraconazole is slightly increased, it is recommended to monitor the concentrations of itraconazole in plasma and adjust the dose of the drug, if necessary.
Patients with immunodeficiencies: bioavailability of itraconazole in per oral administration may be reduced in some patients with impaired immunity, such as patients with neutropenia, patients with AIDS or patients who underwent surgery for organ transplantation.
Patients with systemic fungal infections that are life-threatening: Due to the pharmacokinetic characteristics of Orungal® capsules, it is not recommended for initiating treatment of systemic mycoses that are life-threatening to patients.
AIDS patients: The treating physician should evaluate the need for maintenance therapy in AIDS patients previously treated for systemic fungal infections such as sporotrichosis, blastomycosis, histoplasmosis, or cryptococcosis (both meningeal and nonmeningeal) who are at risk for relapse.
The clinical data on the use of Orungal® capsules in pediatric practice are limited. Orungal® capsules should not be administered to children unless the expected benefit exceeds the possible risk.
The treatment should be discontinued if peripheral neuropathy occurs, which may be associated with the administration of Orungal® capsules.
There are no data on cross-sensitivity to itraconazole and other azole antifungal drugs.
Contraindications
Contraindications
With caution: the drug should be prescribed in patients with liver cirrhosis, chronic renal insufficiency, chronic heart failure, hypersensitivity to other drugs of azole group, as well as in children and elderly patients.
Side effects
Side effects
Immune system disorders: very rare – anaphylactic, anaphylactoid and allergic reactions.
Metabolic disorders: very rare – hypokalemia.
Nervous system disorders: very rare – peripheral neuropathy, headache, dizziness.
Cardiovascular system disorders: very rarely – congestive heart failure.
Respiratory system: very rare – pulmonary edema;
Gastrointestinal system: very rare – abdominal pain, vomiting, dyspepsia, nausea, decreased appetite, diarrhea, constipation.
Hepatobiliary system disorders: very rarely – severe toxic liver damage (including several cases of acute liver failure with lethal outcome), hepatitis, reversible increase in liver enzymes.
Skin and subcutaneous fatty tissue disorders: very rarely – Stevens-Johnson syndrome, angioedema, urticaria, alopecia, photosensitivity, rash, itching.
Reproductive system disorders: very rarely – disruption of the menstrual cycle.
General disorders: very rare – edema syndrome.
Overdose
Overdose
No cases of overdose of Orungal have been reported.
Treatment: In case of accidental overdose, gastric lavage should be performed within the first hour after taking the drug and, if necessary, activated charcoal should be prescribed. Itraconazole is not excreted by hemodialysis. There is no specific antidote.
Pregnancy use
Pregnancy use
Pregnancy. Orungal® should not be used in pregnancy except in life-threatening cases and if the expected beneficial effect exceeds the possible harm to the fetus.
There are insufficient data on the use of Orungal® solution during pregnancy. Cases of congenital abnormalities have been reported during the clinical use of the drug after registration. These cases included visual, skeletal, genitourinary and cardiovascular abnormalities as well as chromosomal abnormalities and multiple malformations. However, whether the use of Orungal® solution causes these abnormalities has not been reliably established.
The epidemiologic data regarding exposure to Orungal® in the first trimester of pregnancy, primarily in patients receiving short-term therapy for vulvovaginal candidiasis, did not show an increased risk of congenital abnormalities compared to a control group not exposed to any of the known teratogenic factors.
Women of childbearing age taking Orungal® solution should use adequate contraception for the duration of treatment until their first menstrual period after completion.
Lactation. Since itraconazole may penetrate into the breast milk, women using Orungal® should stop breastfeeding if use during lactation is necessary.
Similarities
Similarities
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C. |
| Manufacturer | Janssen Pharmaceuticals N.V., Belgium |
| Medication form | oral solution |
| Brand | Janssen Pharmaceuticals N.V. |
Related products
Buy Orungal, 10 mg/ml 150 ml with delivery to USA, UK, Europe and over 120 other countries.