No products in the cart.
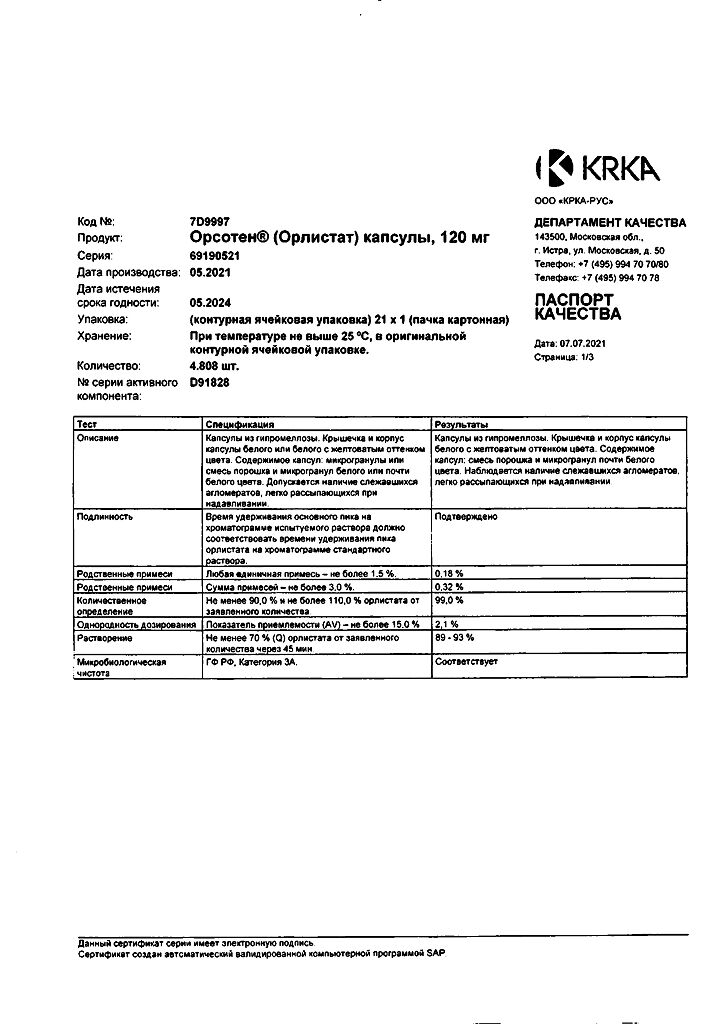
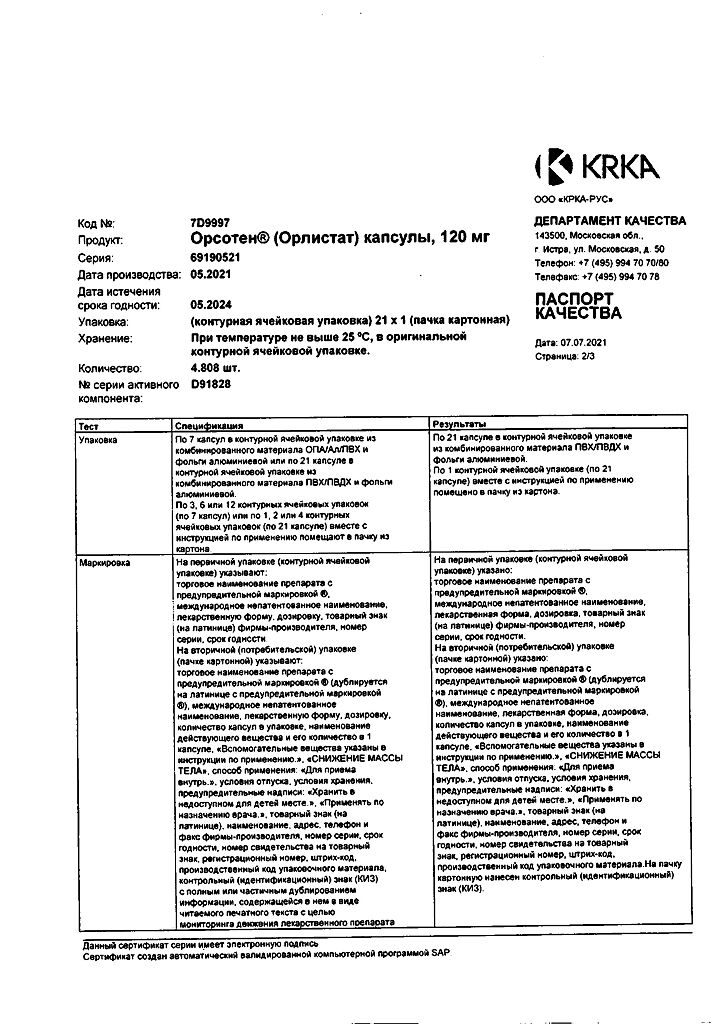
Orsoten, 120 mg capsules 21 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Orsotene is an inhibitor of gastrointestinal lipases.
Pharmacodynamics
Orlistat is a specific inhibitor of gastrointestinal lipases with prolonged action. It has a therapeutic effect in the lumen of the stomach and small intestine by forming a covalent bond with the active serine site of gastric and intestinal lipases. The enzyme, thus inactivated, loses its ability to break down dietary fats that come in the form of triglycerides into absorbable free fatty acids and monoglycerides. Because these uncracked triglycerides are not absorbed, the caloric intake is reduced, resulting in weight loss.
The therapeutic effect of the drug is carried out without absorption into the systemic blood flow. The action of orlistat leads to increase of fat content in feces 24-48 hours after taking the drug. After discontinuation of the drug the content of fat in stool usually returns to the initial level in 48-72 hours.
Pharmacokinetics
Intake. Absorption of orlistat is low. In 8 hours after oral administration of therapeutic dose unchanged orlistat is practically not detected in blood plasma (concentration – < 5 ng/ml). There are no signs of cumulation, which confirms the minimal absorption of the drug.
Distribution. In vitro orlistat is more than 99% bound to plasma proteins (mainly to lipoproteins and albumin). In minimal amounts orlistat can penetrate into erythrocytes.
Metabolism. Orlistat is metabolized primarily in the intestinal wall to form pharmacologically inactive metabolites: M1 (hydrolyzed four-membered lactone ring) and M3 (M1 with a detached N-formylleucine residue).
Elimination. The main route of elimination is excretion through the intestine – about 97% of the administered dose of the drug, of which 83% is orlistat in unchanged form.
Cumulative excretion through the kidneys of all the substances structurally related to orlistat is less than 2% of the administered dose of the drug. Total elimination time is 3-5 days. Orlistat and metabolites may be excreted with the bile.
Indications
Indications
Long-term treatment of patients with conditions such as:
obesity (body mass index (BMI) ≥30 kg/m2);
overweight (BMI ≥28 kg/m2), incl. having risk factors associated with obesity, in combination with a moderately low-calorie diet.
Orsoten can be prescribed in combination with hypoglycemic drugs and/or a moderately low-calorie diet in patients with type 2 diabetes mellitus who are overweight or obese.
Pharmacological effect
Pharmacological effect
Orsoten is a gastrointestinal lipase inhibitor.
Pharmacodynamics
Orlistat is a specific inhibitor of gastrointestinal lipases with a long-lasting effect. It has a therapeutic effect in the lumen of the stomach and small intestine, forming a covalent bond with the active serine site of gastric and intestinal lipases. Thus inactivated, the enzyme loses its ability to break down dietary fats, supplied in the form of triglycerides, into absorbable free fatty acids and monoglycerides. Since undigested triglycerides are not absorbed, the body’s calorie intake is reduced, leading to weight loss.
The therapeutic effect of the drug is carried out without absorption into the systemic circulation. The effect of orlistat leads to an increase in fat content in stool within 24–48 hours after taking the drug. After discontinuation of the drug, the fat content in stool usually returns to its original level within 48–72 hours.
Pharmacokinetics
Suction. Orlistat absorption is low. 8 hours after oral administration of a therapeutic dose, unchanged orlistat in the blood plasma is practically undetectable (concentration – <5 ng/ml). There are no signs of cumulation, which confirms minimal absorption of the drug.
Distribution. In vitro, orlistat is more than 99% bound to plasma proteins (mainly lipoproteins and albumin). In minimal quantities, orlistat can penetrate red blood cells.
Metabolism. Orlistat is metabolized mainly in the intestinal wall to form pharmacologically inactive metabolites: M1 (hydrolyzed four-membered lactone ring) and M3 (M1 with a cleaved N-formylleucine residue).
Excretion. The main route of elimination is excretion through the intestines – about 97% of the dose taken, of which 83% is orlistat in unchanged form.
The cumulative excretion through the kidneys of all substances structurally related to orlistat is less than 2% of the dose taken. The time for complete elimination is 3–5 days. Orlistat and metabolites can be excreted in bile.
Special instructions
Special instructions
Orlistat is effective for long-term weight control (reducing body weight, maintaining it at an appropriate level and preventing weight gain). Treatment with orlistat leads to an improvement in the profile of risk factors and diseases associated with obesity (including hypercholesterolemia, impaired glucose tolerance, hyperinsulinemia, arterial hypertension, type 2 diabetes mellitus) and a decrease in the amount of visceral fat.
Weight loss during treatment with orlistat may be accompanied by improved compensation of carbohydrate metabolism in patients with type 2 diabetes, which may allow a reduction in the dose of hypoglycemic drugs.
To ensure adequate nutrition, patients are advised to take multivitamins.
Patients should follow dietary recommendations. They should receive a balanced, moderately low-calorie diet containing no more than 30% of calories from fat. Daily fat intake should be divided into three main meals.
The likelihood of developing gastrointestinal adverse reactions may increase if orlistat is taken with a diet rich in fat (e.g. 2000 kcal/day, more than 30% of daily caloric intake comes from fat, which equates to approximately 67 g of fat). Patients should be aware that the more accurately they follow their diet (especially in relation to the amount of fat allowed), the less likely they are to develop adverse reactions. A low-fat diet reduces the likelihood of developing gastrointestinal adverse reactions and helps patients monitor and regulate their fat intake.
If after 12 weeks of therapy there is no reduction in body weight by at least 5%, orlistat should be discontinued.
Active ingredient
Active ingredient
Orlistat
Composition
Composition
Active ingredient:
orsoten semi-finished granules 225.6 mg (in terms of the active substance orlistat – 120 mg);
Excipients:
MCC
Contraindications
Contraindications
hypersensitivity to orlistat or any other components of the drug;
chronic malabsorption syndrome;
cholestasis;
pregnancy;
breastfeeding;
children under 18 years of age (efficacy and safety have not been studied).
Side Effects
Side Effects
Adverse reactions to orlistat were mainly observed in the gastrointestinal tract and were caused by an increased amount of fat in the feces. Typically observed adverse reactions are mild and transient. The appearance of these phenomena was observed at the initial stage of treatment during the first 3 months (but not more than one case). With long-term use of orlistat, the incidence of side effects decreases.
There are: flatulence accompanied by rectal discharge, urge to defecate, greasy/oily stools, oily rectal discharge, loose stools, soft stools, inclusions of fat in the stool (steatorrhea), pain/discomfort in the abdomen, increased frequency of bowel movements, pain/discomfort in the rectum, urge to defecate, fecal incontinence, dental damage and gums; hypoglycemia in patients with type 2 diabetes, headache, anxiety, flu, fatigue, upper respiratory tract infections, urinary tract infections, dysmenorrhea, rarely: allergic reactions (eg itching, rash, urticaria, angioedema, bronchospasm, anaphylaxis); very rarely – diverticulitis, cholelithiasis, hepatitis (possibly severe), bullous rash, increased levels of liver transaminases and alkaline phosphatase.
Interaction
Interaction
Patients receiving warfarin or other anticoagulants and orlistat may experience a decrease in prothrombin levels and an increase in the international normalization ratio (INR), which leads to changes in hemostatic parameters.
No interactions were observed with amitriptyline, biguanides, digoxin, fibrates, fluoxetine, losartan, phenytoin, oral contraceptives, phentermine, nifedipine GITS, sustained-release nifedipine, sibutramine, furosemide, captopril, atenolol, glibenclamide, or ethanol. Increases the bioavailability and lipid-lowering effect of pravastatin, increasing its plasma concentration by 30%. Weight loss can improve metabolism in patients with diabetes, as a result of which it is necessary to reduce the dose of oral hypoglycemic agents. Treatment with orlistat may potentially interfere with the absorption of fat-soluble vitamins (A, D, E. K). If multivitamins are recommended, they should be taken no earlier than 2 hours after taking orlistat or before bedtime.
When taking orlistat and cyclosporine simultaneously, a decrease in the level of cyclosporine concentration in the blood plasma was observed, therefore it is recommended to determine the level of cyclosporine concentration in the blood plasma more often.
Patients receiving amiodarone should undergo more careful clinical observation and ECG monitoring, because Cases of decreased plasma amiodarone concentrations have been described.
Overdose
Overdose
Cases of overdose have not been described.
A single dose of orlistat 800 mg or multiple doses of up to 400 mg three times daily for 15 days was not associated with significant adverse reactions.
In addition, a dose of 240 mg three times daily given to obese patients for 6 months did not cause a significant increase in side effects. In case of orlistat overdose, it is recommended to monitor the patient for 24 hours.
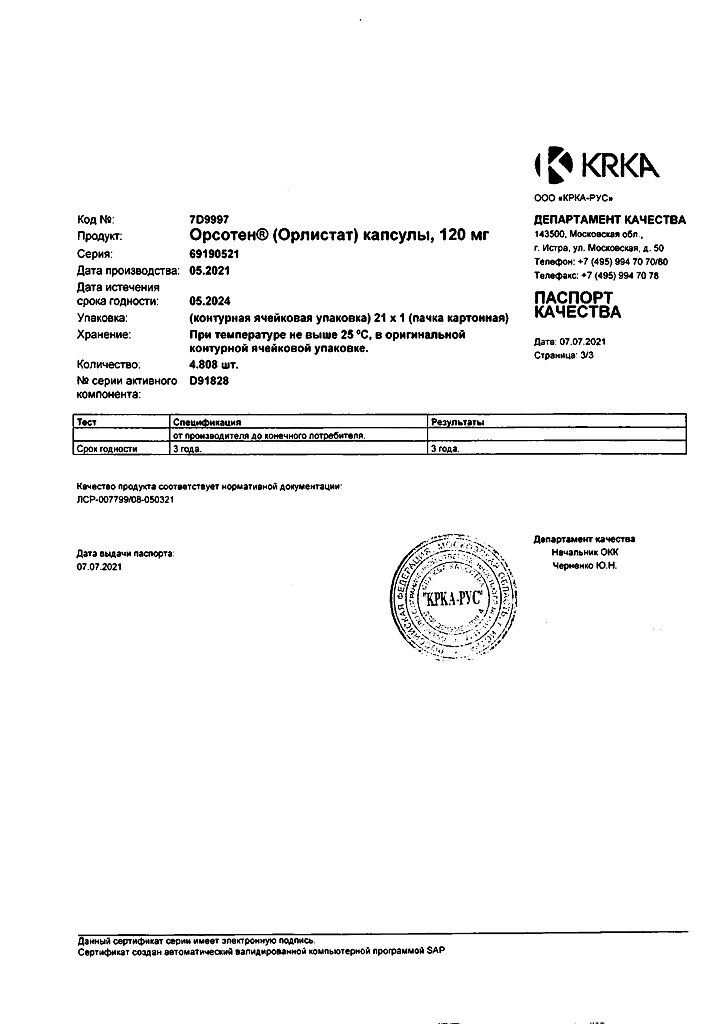
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
KRKA-RUS, Russia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | capsules |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Orsoten, 120 mg capsules 21 pcs with delivery to USA, UK, Europe and over 120 other countries.