No products in the cart.
Description
Pharmacodynamics
Oncotron is a cytostatic drug, a synthetic derivative of anthracenedione. The mechanism of antitumor action is not fully understood, but preliminary data shows that the drug, being inserted between the bases of DNA molecule, blocks the processes of replication and transcription. In addition, mitoxanthror inhibits topoisomerase II and has a nonspecific effect on the cell cycle.
Pharmacokinetics
Mitoxantrone quickly penetrates and distributes into tissues after IV administration, from where it is then gradually released. It is found in high concentrations in the liver, lungs and in descending order: bone marrow, heart, thyroid, spleen, pancreas, adrenal glands and kidneys. It does not penetrate the GEB.
Binding with plasma proteins is 90%. It is metabolized in the liver. Within 5 days 13.6-24.8% of preparation is excreted with bile and 5.2% to 7.9% with urine. The terminal T1/2 reaches 9 days.
In patients with hepatic dysfunction, a decrease in the elimination rate of the drug has been noted.
Indications
Indications
Acute non-lymphoblastic leukemia in adults;
breast cancer;
malignant non-Hodgkin’s lymphomas;
primary hepatocellular carcinoma;
ovarian cancer;
hormone-resistant prostate cancer with pain syndrome.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
Oncotron is a cytostatic drug, a synthetic derivative of anthracenedione. The mechanism of the antitumor effect has not been fully elucidated, but preliminary data indicate that the drug, being embedded between the bases of the DNA molecule, blocks the processes of replication and transcription. In addition, mitoxantror inhibits topoisomerase II and has a nonspecific effect on the cell cycle.
Pharmacokinetics
After intravenous administration, mitoxantrone quickly penetrates and distributes in tissues, from where it is then gradually released. It is found in high concentrations in the liver, lungs and, in descending order: bone marrow, heart, thyroid gland, spleen, pancreas, adrenal glands and kidneys. Does not penetrate the BBB.
Plasma protein binding – 90%. Metabolized in the liver. Within 5 days, 13.6-24.8% of the drug is excreted from the body with bile and from 5.2% to 7.9% of the drug with urine. Terminal T1/2 reaches 9 days.
In patients with impaired liver function, a decrease in the rate of drug elimination was observed.
Special instructions
Special instructions
Treatment with mitoxantrone should be carried out under the supervision of a physician experienced in working with anticancer drugs.
During the treatment process, systematic monitoring of the peripheral blood picture is necessary (before each administration, a complete blood count is required, including platelet count), laboratory indicators of liver function, as well as cardiac activity (ECG, EchoCG with determination of left ventricular ejection fraction (LVEF)). After reaching a total dose of mitoxantrone of 100 mg/m2, determination of LVEF values should be carried out before each subsequent administration of the drug.
Active or inactive cardiovascular disease, radiotherapy to the mediastinal/pericardial region previously or concomitantly with mitoxantrone, previous treatment with other anthracyclines or anthracenediones, and concomitant treatment with other cardiotoxic drugs may increase the risk of cardiac toxicity. The risk of cardiotoxicity increases when the total dose of mitoxantrone exceeds 140 mg/m2, however, toxic cardiac damage can develop at lower total doses of the drug.
Because Some patients with acute leukemia may develop severe stomatitis; it is recommended to take preventive measures.
When treating leukemia, hyperuricemia may occur as a result of the rapid breakdown of tumor cells. If necessary, hypouricemic drugs should be prescribed.
In case of extravasation, it is necessary to stop the drug administration and, if necessary, continue the infusion into another vein.
The use of topoisomerase II inhibitors, including mitoxantrone, in combination with other anticancer drugs and/or radiotherapy, can lead to the development of acute myeloid leukemia or myelodysplastic syndrome.
Due to the immunosuppressive effect of the drug and the possibility of developing severe infections, it is not recommended to use live vaccines during chemotherapy. Vaccination should be carried out 3 months after completion of therapy.
Women and men should use reliable methods of contraception during treatment with mitoxantrone, as well as for 6 months after its discontinuation.
Contact of the drug with the skin or mucous membranes should be avoided, because tissue necrosis may occur. In case of contact with the drug, the skin must be thoroughly rinsed with warm water.
If necessary, an undiluted solution of Oncotron (with aseptic sampling of the drug from the vial) can be used in parts for 7 days, provided it is stored at a temperature not exceeding 25°C.
After dilution, the Oncotron solution should be used within 4 days (aseptic collection conditions, storage at a temperature of 4-25°C); after 96 hours, the unused drug should not be used.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Mitoxantrone
Composition
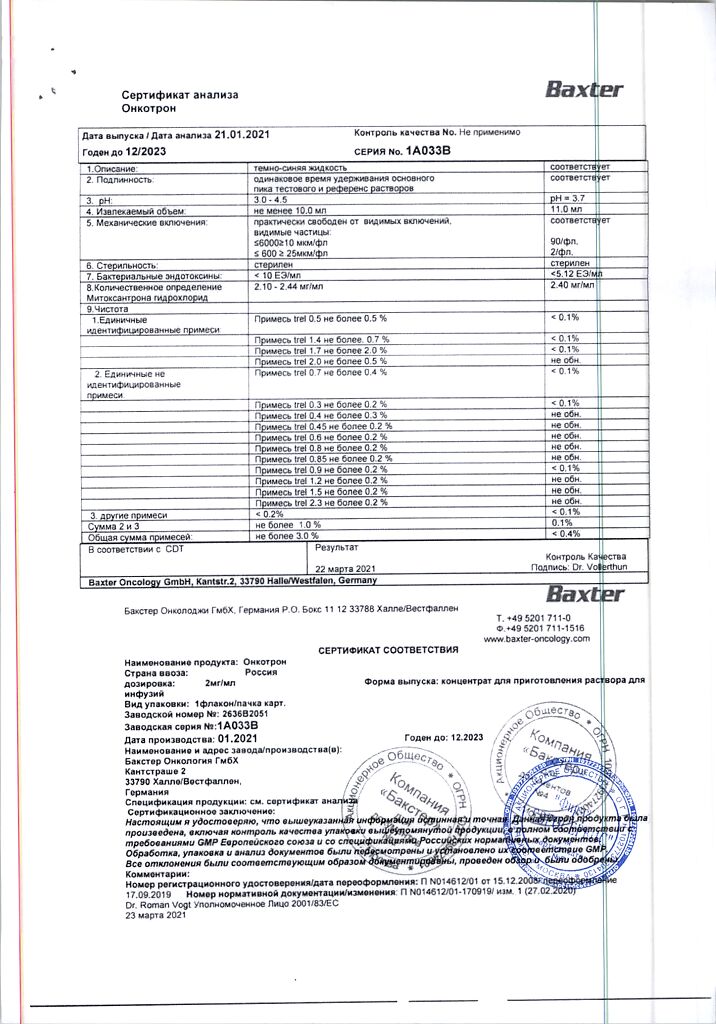
Composition
1 ml of concentrate contains:
Active ingredients:
mitoxantrone hydrochloride 2.328 mg, which corresponds to the content of mitoxantrone 2 mg.
Excipients:
sodium chloride,
sodium acetate,
glacial acetic acid,
water d/i.
Pregnancy
Pregnancy
Contraindicated during pregnancy and lactation.
Contraindications
Contraindications
Neutrophil count less than 1500/μl (except for treatment of non-lymphoblastic leukemia);
lactation period;
pregnancy;
hypersensitivity to mitoxantrone or any other component of the drug.
With caution: use Oncotron in patients with heart disease, with previous irradiation of the mediastinum, with suppression of hematopoiesis, with severe impairment of liver or kidney function, with bronchial asthma, with acute infectious diseases of a viral (including chicken pox, herpes zoster), fungal or bacterial nature (the risk of severe complications and generalization of the process), with diseases in which there is an increased risk of developing hyperuricemia (gout or urate nephrolithiasis) and in patients previously treated with anthracyclines.
Side Effects
Side Effects
From the hematopoietic system: leukopenia (usually on days 6-15, recovery on day 21), neutropenia. thrombocytopenia, erythrocytopenia; rarely – anemia.
From the digestive system: nausea, vomiting, anorexia, loss of appetite, diarrhea, abdominal pain, constipation, gastrointestinal bleeding, stomatitis; rarely – increased activity of liver transaminases, impaired liver function.
From the cardiovascular system: ECG changes, tachycardia, arrhythmias, myocardial ischemia, decreased left ventricular ejection fraction, congestive heart failure. Toxic myocardial damage, in particular congestive heart failure, can develop both during treatment with mitoxantrone and months and years after the end of therapy. The risk of cardiotoxic effect increases when the total dose reaches 140 mg/m2.
From the respiratory system: cases of interstitial pneumonitis have been described.
Allergic reactions: skin itching. rash, urticaria, shortness of breath, decreased blood pressure, anaphylactic reactions (including anaphylactic shock).
Local reactions: phlebitis, with extravasation – erythema, swelling, pain, burning, necrosis of surrounding tissues. Cases of intense blue staining of the veins into which the drug was injected and the surrounding tissues have been described.
Other: alopecia, increased fatigue, general weakness, increased body temperature, nonspecific neurological symptoms, back pain, headache, menstrual irregularities, amenorrhea; rarely – blue coloring of the skin and nails; very rarely – nail dystrophy and reversible blue staining of the sclera, secondary infections, hyperuricemia, hypercreatininemia.
Interaction
Interaction
Pharmaceutical interactions
Do not mix the drug with other drugs when administered intravenously (precipitation may occur).
Pharmacodynamic interaction
Oncotron potentiates the effect of many cytotoxic drugs, such as cytarabine, cisplantin, cyclophosphamide, 5-fluorouracil, methotrexate, vincristine, dacarbazine.
When Oncotron is used simultaneously with other antitumor drugs or irradiation of the mediastinal area, its cardio- and myelotoxicity may increase.
The simultaneous administration of drugs that block tubular secretion (including uricosuric anti-gout drugs – sulfinpyrazone) may increase the risk of developing nephropathy.
Pharmacokinetic interaction
No dangerous interactions with other drugs have been detected.
Overdose
Overdose
Symptoms: increased, primarily, myelotoxicity and the above-mentioned side effects.
Treatment: dialysis is not effective. In case of overdose, the patient should be closely monitored and, if necessary, symptomatic therapy should be provided. A specific antidote for mitoxantrone is unknown.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C (do not freeze)
Shelf life
Shelf life
3 years
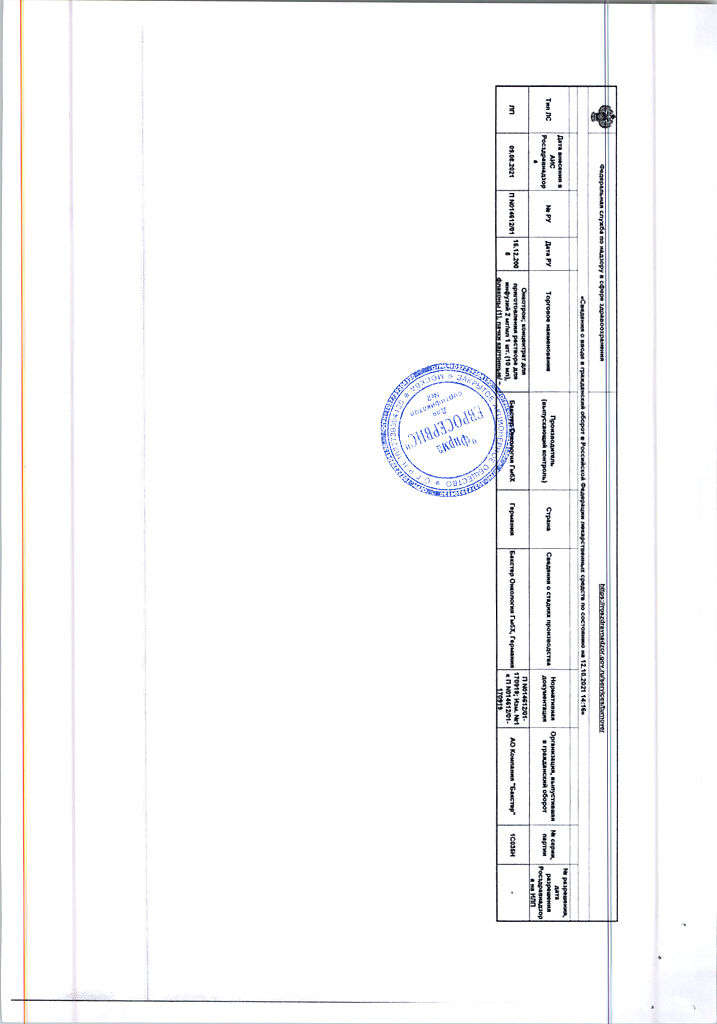
Manufacturer
Manufacturer
Baxter Oncology GmbH, Germany
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C (do not freeze) |
| Manufacturer | Baxter Oncology GmbH, Germany |
| Medication form | concentrate for preparation of infusion solution |
| Brand | Baxter Oncology GmbH |
Related products
Buy Oncotron, 2 mg/ml 10 ml with delivery to USA, UK, Europe and over 120 other countries.