No products in the cart.
Ofloxacin Sanofi, 200 mg 10 pcs
€4.94 €4.11
Description Pharmacotherapeutic group: Pharmacodynamics:
Antimicrobial agent – fluoroquinolone
ATC: J01MA01 Ofloxacin
Ofloxacin is a synthetic broad-spectrum antibacterial drug from the group of fluoroquinolones with bactericidal action. The main mechanism of action of quinolones is specific inhibition of bacterial DNA-gyrase. DNA-gyrase is necessary for replication, transcription, repair and recombination of bacterial DNA. Its inhibition leads to unwinding and destabilization of bacterial DNA and consequently to the death of the microbial cell. It is highly active against the majority of Gram-negative and Gram-positive microorganisms.
Fluoroquinolones have concentration-dependent bactericidal activity and moderate post-antibacterial action. The ratio of AUC to minimum inhibitory concentration (MIC) or the ratio of maximum plasma concentration (Cmax) to MIC is predictive of successful therapy.
Sensitive microorganisms
Non-sensitive microorganisms (possibly due to acquired resistance): Citrobacter freundii, Escherichia coli, Klebsiella oxytoca, Klebsiella pneumoniae, Neisseria gonorrhoeae, Proteus mirabilis, Pseudomonas aeruginosa, Serratia spp, Staphylococcus spp. (coagulazonegative strains), Staphylococcus aureus (methicillin-sensitive strains), Streptococcus pneumoniae, Staphylococcus epidermidis, Campylobacter jejuni, Enterococcus faecali.
Resistant microorganisms
Acinetobacter baumannii, Bacteroides spp., Clostridium difficile, Enterococci, Listeria monocytogenes, Staphylococcus spp. (methicillin-resistant strains), Nocardia spp.
Resistance
Resistance to ofloxacin develops as a result of a stepwise process of mutations in the genes encoding both type II topoisomerases: DNA-Gyrase and topoisomerase IV. Other mechanisms of resistance, such as effects on the permeability of the outer structures of the microbial cell (a mechanism characteristic of Pseudomonas aeruginosa), the mechanism of efflux (active excretion of the antimicrobial agent from the microbial cell), can also affect the sensitivity of microorganisms to ofloxacin.
Pharmacokinetics:
After oral administration ofloxacin is quickly and almost completely absorbed from the gastrointestinal tract (GIT). Bioavailability is almost 100%, plasma protein binding is 25%.
Max ofloxacin after oral administration of 200 mg averaged 2.5-3 mcg/ml and was reached within one hour.
The apparent volume of distribution is 120 liters. Concentrations of ofloxacin in the urine and infected urinary tract exceed plasma concentrations of ofloxacin by 5 to 100 times.
It is metabolized in the liver (about 5%) to form ofloxacin N-oxide and N-desmethylofloxacin.
The elimination half-life (T1/2) is 6-7 hours.
It is mainly excreted by the kidneys – 80-90% (unchanged), about 4% is excreted in the bile as glucuronide.
The serum concentrations increase slightly after repeated administration (accumulation rate is about 1.5).
Special patient groups
Elderly patients: There is an increase in T1/2 but no change in Cmax.
Patients with renal insufficiency: T1/2 is longer, with renal clearance rates decreasing in relation to creatinine clearance (CK) rates.
.
Indications
Indications
Infectious inflammatory diseases caused by microorganisms sensitive to Ofloxacin:
The official national guidelines for the appropriate use of antibacterials as well as the sensitivity of pathogens in a specific country should be considered when using the drug.
Active ingredient
Active ingredient
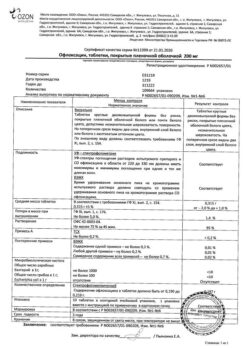
Composition
Composition
Active ingredient: ofloxacin – 200.00 mg;
excipients: core: lactose monohydrate – 95.20 mg, corn starch – 47.60 mg, povidone 25 – 12.00 mg, crosspovidone – 20.00 mg, poloxamer – 0.20 mg, magnesium stearate – 8.00 mg, talc – 4.00 mg; film coating: hypromelose 2910/5 – 9.42 mg, macrogol 6000 – 0.53 mg, talc – 0.70 mg, titanium dioxide – 2.35 mg.
How to take, the dosage
How to take, the dosage
Interaction
Interaction
Theophylline, phenbufen or similar non-steroidal anti-inflammatory drugs
There have been no pharmacokinetic interactions between ofloxacin and theophylline in clinical studies. However, a marked decrease in cerebral seizure threshold may be observed with concomitant use of quinolones with theophylline, NSAIDs or other drugs that reduce cerebral seizure threshold (including with phenbufen).
Drugs causing prolongation of the QT interval
Ofloxacin, like other fluoroquinolones, should be used with caution in patients receiving drugs that cause prolongation of the QT interval on ECG (e.g., antiarrhythmic drugs of class IA and III, tricyclic antidepressants, macrolides, neuroleptics).
Glibenclamide
Special Instructions
Special Instructions
Hypersensitivity reactions and allergic reactions
Disability and potential irreversible serious adverse reactions due to fluoroquinolones
The use of fluoroquinolones, including ofloxacin, has been associated with disability and irreversible serious adverse reactions in various body systems, which can occur simultaneously in the same patient.
The adverse reactions caused by fluoroquinolones include tendonitis, tendon rupture, arthralgia, myalgia, peripheral neuropathy, and nervous system side effects (hallucinations, anxiety, depression, insomnia, headaches and confusion).
These reactions may occur within a few hours to a few weeks after starting therapy with ofloxacin.
The development of these adverse reactions has been reported in patients of any age or without prior risk factors.
The first signs or symptoms of any serious adverse reactions should be discontinued immediately.
The use of fluoroquinolones, including ofloxacin, should be avoided in patients who have already had any of these serious adverse reactions.
Pseudomembranous colitis (disease associated with Clostridium difficile)
Patients prone to developing seizures
Tendinitis and tendon rupture
Tendinitis, which is rarely seen with quinolone treatment, can sometimes lead to tendon rupture, particularly of the Achilles tendon, and may be bilateral. This side effect may develop within 48 hours of treatment initiation or within several months after completion of fluoroquinolone therapy.
Elderly patients are more likely to develop tendinitis.
The risk of tendon rupture may increase with concomitant use of glucocorticosteroids.
In addition, transplant patients are at increased risk for tendinitis, and use of fluoroquinolones with caution is recommended in this group of patients.
In patients with impaired renal function the daily dose should be calculated based on CK (see section “Doses and administration”).
Patients should remain at rest at the first signs of tendinitis or tendon rupture and see their physician. If signs of tendonitis or tendon rupture occur, treatment with ofloxacin should be stopped immediately. Appropriate treatment (e.g., immobilization) of the damaged tendon should be started immediately.
Serious skin adverse reactions
The development of severe bullous reactions such as Stevens-Johnson syndrome and toxic epidermal necrolysis has been reported while taking ofloxacin. Patients should be informed that if skin reactions and/or mucous membrane lesions develop, it is necessary to immediately consult a physician before continuing treatment with ofloxacin.
Patients with impaired renal function
Patients with a history of psychotic disorders
Patients with impaired liver function
Pseudoparalytic myasthenia gravis
Prevention of photosensitization
Due to the risk of photosensitization, exposure to intense sunlight and ultraviolet radiation should be avoided during treatment with the drug ofloxacin.
Superinfection
As with other antimicrobial agents, superinfection associated with the growth of drug-resistant microorganisms is possible with the use of of ofloxacin, especially for a long time; the patient should be reevaluated to exclude and confirm it. If superinfection develops during therapy, necessary measures should be taken to treat it.
Long QT interval
Cases of QT interval prolongation have been observed in patients taking fluoroquinolones, including ofloxacin.
Contraindications
Contraindications
– Hypersensitivity to ofloxacin, other quinolones or excipients of the drug;
– epilepsy;
– pseudoparalytic myasthenia gravis (see sections “Side Effects” and “Precautions”). Side effects, Special Precautions);
– tendon damage with previous treatment with quinolones;
– Age before 18 years of age (the risk of cartilage bone growth zone damage in a child cannot be completely excluded);
– pregnancy and breastfeeding (the risk of cartilage growth zone lesions in the fetus cannot be completely excluded);
– lactase deficiency, lactose intolerance, glucose-galactose malabsorption.
– Predisposition to the development of seizures (pronounced atherosclerosis of cerebral vessels, cerebral circulation disorders in the history, organic lesions of the central nervous system (CNS), brain injuries in the history);
– renal function disorders (mandatory monitoring of renal function parameters, as well as dosing regimen correction is required, see.
– hepatic insufficiency (control of liver function parameters);
– porphyria;
– risk factors for QT interval prolongation: elderly age; uncorrected electrolyte disorders (hypokalemia, hypomagnesemia); congenital QT interval prolongation syndrome; heart disease (heart failure, myocardial infarction, bradycardia); concomitant use of drugs that may prolong the QT interval (e.g., antiarrhythmic drugs of classes IA and III, tricyclic antidepressants, macrolides, neuroleptics);
– severe adverse reactions to other quinolones, such as severe neurological reactions (increased risk of similar adverse reactions with ofloxacin);
– history of psychosis or other psychiatric disorders;
– older age, post-transplant condition, concomitant use of glucocorticosteroids (increased risk of tendinitis and tendon rupture).
Side effects
Side effects
The information below is based on data from clinical studies and extensive post-registration experience with the drug.
The frequency of adverse reactions was determined according to the following grading (World Health Organization classification): Very common (⥠1/10), common (⥠1/100, but < 1/10); infrequent (⥠1/1000, but < 1/100); rare (⥠1/10000, but < 1/1000); very rare (< 1/10000), frequency unknown (the frequency could not be determined from available data).
Infectious and parasitic diseases: infrequent fungal infection, resistance of pathogens.
Blood and lymphatic system disorders: very rarely – anemia, hemolytic anemia, leukopenia, eosinophilia, thrombocytopenia; frequency is unknown – agranulocytosis, pancytopenia, suppression of medullar hemopoiesis.
Immune system disorders: rare – anaphylactic reaction, anaphylactoid reaction, angioedema; very rare – anaphylactic shock, anaphylactoid shock.
Disorders of metabolism and nutrition: rare – anorexia; frequency unknown – hyperglycemia, hypoglycemia, hypoglycemic coma (in patients with diabetes receiving hypoglycemic drugs).
Mental disorders: infrequent – agitation, sleep disturbance, insomnia; rare – psychotic disorders (hallucinations), anxiety, nervousness, confusion, “nightmare” dreams, depression; frequency unknown – psychotic disorders and depression with self-destructive behavior, including suicidal thoughts and suicide attempts.
Nervous system disorders: infrequent – dizziness, headache; rare – somnolence, paresthesia, dysgeusia (taste perception disorder), parosmia (olfactory disorder); very rare – peripheral sensory neuropathy, peripheral sensory-motor neuropathy, seizures, extrapyramidal symptoms, including tremor, and other disorders of muscle coordination; frequency unknown – agueusia (loss of ability to sense taste), increased intracranial pressure (benign intracranial hypertension, pseudotumor of the brain).
Visual disorders: infrequent – irritation of the mucous membrane of the eye, conjunctivitis; rarely – visual impairment (diplopia, color perception disorders); frequency is unknown – uveitis.
Hearing and labyrinth disorders: infrequent – vertigo; very rare – ringing or noise in the ears, hearing loss.
Chronic disorders: infrequent – tachycardia; infrequent – palpitations; frequency unknown – ventricular pirouette (mainly seen in patients with risk factors for prolonged QT interval), prolongation of the QT interval on ECG.
Vascular disorders: rarely – increase of blood pressure, decrease of blood pressure.
Respiratory system, thoracic and mediastinal disorders: infrequent – cough, nasopharyngitis; rare – shortness of breath, bronchospasm; frequency unknown – allergic pneumonitis, severe shortness of breath.
Gastrointestinal tract disorders: infrequent – abdominal pain, diarrhea, nausea, vomiting, decreased appetite; rare – enterocolitis (sometimes hemorrhagic); very rare – pseudomembranous colitis; frequency unknown – dyspepsia, flatulence, constipation, pancreatitis, stomatitis.
Liver and biliary tract disorders: rare – increased-activity of “liver” transaminases (aspartate aminotransferase (ACT), alanine aminotransferase (ALT), lactate dehydrogenase (LDH), gamma-glutamyltransferase (GGT) and/or alkaline phosphatase (ALP) and/or bilirubin concentration; very rare – cholestatic jaundice, frequency is unknown – hepatitis (may be severe), when using ofloxacin (mainly in patients with liver dysfunction). Cases of severe liver failure, including acute liver failure, sometimes fatal, have been reported.
Skin and subcutaneous tissue disorders: infrequent – skin rash, skin itching; rarely – urticaria, “rushes” of blood to the skin, increased sweating, pustular rash; very rarely – erythema multiforme, toxic epidermal necrolysis, photosensitization reaction, drug rash, vascular purpura, vasculitis (which can lead in some cases to skin necrosis), frequency unknown – Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, exfoliative dermatitis.
Muscular and connective tissue disorders: rare – tendinitis; very rare – arthralgia, myalgia, tendon rupture (Achilles tendon, as with other fluoroquinolones this side effect may occur within 48 h after initiation of treatment and may be bilateral); frequency unknown – rhabdomyolysis and/or myopathy, muscle weakness (which may be particularly important in patients with pseudoparalytic myasthenia gravis [myasthenia gravis]), muscle tearing, muscle rupture, ligament tear, arthritis.
Renal and urinary tract disorders: rare – increased serum creatinine concentration; very rare – acute renal failure; frequency unknown – acute interstitial nephritis, increased plasma urea concentration.
General disorders and disorders at the site of administration: frequency unknown – asthenia, increased body temperature, pain in the back, chest, extremities.
Congenital, inherited and genetic disorders: frequency unknown – exacerbation of porphyria in patients with porphyria.
Overdose
Overdose
Symptoms: the most important symptoms of overdose are CNS symptoms (such as dizziness, confusion, disorientation, seizures), prolonged QT interval, as well as gastrointestinal symptoms such as nausea and mucous membrane erosions.
Treatment: gastric lavage, use of activated charcoal and other adsorbents, symptomatic therapy. Antacids may be used to protect the gastric mucosa. ECG monitoring should always be performed due to possible prolongation of the QT interval. Ofloxacin fractions can be removed from the body by hemodialysis. There is no specific antidote.
Pregnancy use
Pregnancy use
Pregnancy use
The use ofloxacin in pregnancy is contraindicated (see section “Contraindications”).
The use of the drug during breastfeeding
Because ofloxacin is excreted into the breast milk, the use of the drug is contraindicated due to the possible risk to the child. If it is necessary to use the drug during lactation, discontinuation of breastfeeding should be considered.
Similarities
Similarities
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 ° C. Store out of the reach of children. |
| Manufacturer | Zentiva k.s., Czech Republic |
| Medication form | pills |
| Brand | Zentiva k.s. |
Other forms…
Related products
Buy Ofloxacin Sanofi, 200 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.