No products in the cart.
Ofloxacin, 400 mg 10 pcs
€2.12 €1.93
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group
Antimicrobial agent, fluoroquinolone
ATX Code
S01AE01
Pharmacodynamics:
A broad-spectrum antimicrobial from the group of fluoroquinolones acts on the bacterial enzyme DNA-hydrase, which provides superspiration and thus the stability of bacterial DNA (destabilization of DNA chains leads to their death). It has a bactericidal effect.
Highly active against most gram-negative and some gram-positive microorganisms: Aeromonas hydrophila Branhamella catarrhalis Brucella spp. Clostridium perfringens Escherichia coli Salmonella spp. Enterobacter spp. Serratia spp. Citrobacter spp. Yersinia spp. Providencia spp. Haemophilus influenzae and parainfluenzae Haemophilus ducreyi Plesiomonas Legionella Shigella spp. Proteus spp. including Proteus mirabilis Proteus vulgaris (indol + indol -) Moraxella morganii Klebsiella spp. (including Klebsiella pneumonia) Helicobacter pylori Mycoplasma spp. Vibrio spp. Gardnerella vaginalis Neisseria gonorrhoeae Neisseria meningitidis Chlamydia trachomatis Staphylococcus aureus methi-S Staphylococcus coagulase negative.
Moderately sensitive to ofloxacin Acinetobacter spp. Ureaplasma urealyticum Bacteroides fragilis Mycobacterium tuberculosis Mycobacterium fortuitum Chlamidia psittaci anaerobic gram-positive cocci Enterococcus faecalis Streptococcus pneumoniae Pseudomonas spp. Streptococcus spp. (especially beta-hemolytic).
Acinetobacter braumanmii Clostridium difficile Enterococci Listeria monocytogenes Staphylococci methi-R Nocardia spp. are insensitive to Ofloxocin.
Ofloxacin is inactive against Treponema pallidum.
Pharmacokinetics:
Absorption after oral administration is fast and complete (95%). Bioavailability – over 96% plasma protein binding – 25%. Time to reach maximum concentration (TCmax) when taken orally – 1 -2 hours. Maximal concentration (Cmax) after a single dose of 100, 200, 300 and 600 mg is 1.3 4 and 6.9 mg/l, respectively, and it depends on the dose: after a single dose of 200 and 400 mg it is 2.5 and 5 mcg/ml, respectively.
Food may delay absorption but has no significant effect on bioavailability. Volume of distribution is 100 l. Distribution: cells (leukocytes alveolar macrophages) skin soft tissues bones abdominal organs and small pelvis respiratory system urine saliva bile prostate secretion; well penetrates through the blood-brain barrier placental barrier is secreted with the mother’s milk. Penetrates into cerebrospinal fluid (14-60%). Metabolized in the liver (about 5%) to form N-oxide ofloxacin and dimethylofloxacin. Half-life (T1/2) – 4.5-7 hours (regardless of the dose). Excreted by the kidneys – 75-90% (unchanged) about 4% – in the bile. Extra-renal clearance is less than 20%.
After a single use in a dose of 200 mg in the urine is detectable within 20-24 hours. With renal/hepatic insufficiency, excretion may be delayed. It does not cumulate. Hemodialysis removes 10-30% of the drug.
Indications
Indications
Treatment of infectious and inflammatory diseases caused by microorganisms sensitive to ofloxacin:
– respiratory tract infections (except for cases of pneumococcal infection);
– infections of the ear, throat, nose (except for cases of acute tonsillitis);
– infections of the abdominal cavity and biliary tract;
– infections of the kidneys, urinary tract, prostate gland, urethra (including gonococcal ones);
– infections of the pelvic organs;
– infections of bones and joints;
– infections of the skin and soft tissues;
– prevention of infections in patients with impaired immune status (including neutropenia).
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group
Antimicrobial agent, fluoroquinolone
ATX code
S01AE01
Pharmacodynamics:
A broad-spectrum antimicrobial agent from the group of fluoroquinolones acts on the bacterial enzyme DNA hydrase, which ensures supercoiling and thus stability of bacterial DNA (destabilization of DNA chains leads to their death). Has a bactericidal effect.
Highly active against most gram-negative and some gram-positive microorganisms: Aeromonas hydrophila Branhamella catarrhalis Brucella spp. Clostridium perfringens Escherichia coli Salmonella spp. Enterobacter spp. Serratia spp. Citrobacter spp. Yersinia spp. Providencia spp. Haemophilus influenzae and parainfluenzae Haemophilus ducreyi Plesiomonas Legionella Shigella spp. Proteus spp. including Proteus mirabilis Proteus vulgaris (indol + indol -) Moraxella morganii Klebsiella spp. (including Klebsiella pneumonia) Helicobacter pylori Mycoplasma spp. Vibrio spp. Gardnerella vaginalis Neisseria gonorrhoeae Neisseria meningitidis Chlamydia trachomatis Staphylococcus aureus methi-S Staphylococcus coagulase negative.
Acinetobacter spp. are moderately sensitive to ofloxacin. Ureaplasma urealyticum Bacteroides fragilis Mycobacterium tuberculosis Mycobacterium fortuitum Chlamydia psittaci anaerobic gram-positive cocci Enterococcus faecalis Streptococcus pneumoniae Pseudomonas spp. Streptococcus spp. (especially beta-hemolytic).
Acinetobacter braumanmii Clostridium difficile Enterococci Listeria monocytogenes Staphylococci methi-R Nocardia spp. is insensitive to ofloxocin.
Ofloxacin is inactive against Treponema pallidum.
Pharmacokinetics:
Absorption after oral administration is rapid and complete (95%). Bioavailability – over 96%; connection with plasma proteins – 25%. The time to reach the maximum concentration (TCmax) after oral administration is 1-2 hours. The maximum concentration (Cmax) after taking a dose of 100 200 300 and 600 mg is 1 3 4 and 6.9 mg/l, respectively, and depends on the dose: after a single dose of 200 and 400 mg it is 2.5 and 5 μg/ml, respectively.
Food may slow absorption but does not significantly affect bioavailability. Distribution volume – 100 l. Distribution: cells (leukocytes, alveolar macrophages) skin soft tissues bones abdominal and pelvic organs respiratory system urine saliva bile secretion of the prostate gland; penetrates well through the blood-brain barrier; the placental barrier is secreted into breast milk. Penetrates into the cerebrospinal fluid (14-60%). Metabolized in the liver (about 5%) to form N-oxide ofloxacin and dimethylofloxacin. The half-life (T1/2) is 4.5-7 hours (regardless of the dose). Excreted by the kidneys – 75-90% (unchanged) and about 4% – with bile. Extrarenal clearance is less than 20%.
After a single dose of 200 mg, it is detected in the urine within 20-24 hours. In case of renal/liver failure, excretion may slow down. Does not cumulate. Hemodialysis removes 10-30% of the drug.
Special instructions
Special instructions
Due to the fact that ofloxacin is excreted mainly through the kidneys, dosage adjustment of ofloxacin is necessary in patients with renal failure. Due to the risk of photosensitivity, exposure to sunlight and ultraviolet rays should be avoided. The appearance of diarrhea, especially severe persistent diarrhea and/or bloody diarrhea during or after treatment with ofloxacin, may be a manifestation of pseudomembranous colitis. If the development of pseudomembranous colitis is suspected, treatment with ofloxacin should be stopped immediately and appropriate specific antibacterial therapy should be prescribed without delay. In this clinical situation, drugs that suppress intestinal motility are contraindicated.
Like other quinolones, ofloxacin should be prescribed with extreme caution to patients predisposed to the development of epileptic seizures (patients with a history of damage to the central nervous system taking fenbufen and similar non-steroidal anti-inflammatory drugs or drugs that lower the seizure threshold, such as theophylline).
Tendonitis, which occurs very rarely, can sometimes lead to tendon rupture, especially the Achilles tendon, especially in older patients. If signs of tendonitis (inflammation of the tendon) appear, it is recommended to immediately stop treatment, immobilize the Achilles tendon and consult an orthopedic surgeon.
Some caution is required when taking fluoroquinolones including ofloxacin in patients with known risk factors for QT prolongation such as:
– old age;
– uncorrectable electrolyte imbalance (for example, hypokalemia, hypomagnesemia); -congenital prolongation of the QT interval;
– diseases of the cardiovascular system (heart failure, myocardial infarction, bradycardia);
– simultaneous use of drugs that prolong the QT interval (classes IA and III antiarthmic drugs, tricyclic antidepressants, macrolides).
Ofloxacin may worsen myasthenia gravis. Possible increased frequency of porphyria attacks. During treatment with ofloxacin, false-positive results may occur when determining opiates and porphyrins in urine.
Ofloxacin prevents the isolation of Mycobacterium tuberculosis, leading to false negative results in the bacteriological diagnosis of tuberculosis. It is also not recommended to consume ethanol during the treatment period. Ofloxacin is not the drug of choice for pneumonia caused by pneumococci. Not indicated for the treatment of acute tonsillitis.
Impact on the ability to drive vehicles. Wed and fur.:
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Ofloxacin
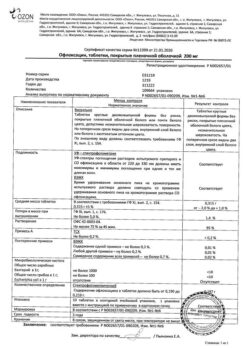
Composition
Composition
Each tablet contains:
Active ingredient:
ofloxacin 400 mg;
Excipients:
corn or potato starch;
MCC;
talc;
low molecular weight polyvinylpyrrolidone;
magnesium or calcium stearate;
Aerosil
Shell composition: hydroxypropyl methylcellulose; talc; titanium dioxide; propylene glycol; polyethylene oxide 4000 or opadry IIOfloxacin – 400 mg.
Pregnancy
Pregnancy
Contraindicated.
Contraindications
Contraindications
– Hypersensitivity to ofloxacin, other quinolones or components of the drug;
– epilepsy;
– damage to the central nervous system with a reduced seizure threshold (after traumatic brain injury, stroke, inflammatory processes in the central nervous system (CNS);
– tendon damage due to previous treatment with quinolones;
– deficiency of glucose-6-phosphate dehydrogenase;
– age up to 18 years;
– pregnancy and lactation period.
With caution:
In patients with cerebral atherosclerosis, cerebrovascular accident (history), chronic renal failure, organic lesions of the central nervous system with prolongation of the QT interval.
Side Effects
Side Effects
From the digestive system: gastralgia, loss of appetite, nausea, vomiting, diarrhea, flatulence, abdominal pain, increased activity of liver transaminases, hyperbilirubinemia, cholestatic jaundice, pseudomembranous enterocolitis.
From the nervous system: headache, dizziness, uncertainty of movements, tremor, convulsions, numbness and paresthesia of the limbs, intense dreams, “nightmare” dreams, psychotic reactions, anxiety, state of excitation, phobias, depression, confusion, hallucinations, increased intracranial pressure.
From the musculoskeletal system: tendonitis myalgia arthralgia tenosynovitis tendon rupture.
From the senses: impaired color vision, diplopia, impaired taste, smell, hearing and balance.
From the cardiovascular system: tachycardia, decreased blood pressure (BP)
Allergic reactions: skin rash itching urticaria allergic pneumonitis allergic nephritis eosinophilia fever angioedema bronchospasm; exudative erythema multiforme (including Stevens-Johnson syndrome) and toxic epidermal necrolysis (Lyell’s syndrome), photosensitivity, vasculitis, anaphylactic shock.
From the skin: pinpoint hemorrhages (petechiae), bullous hemorrhagic dermatitis, papular rash with crust, indicating vascular damage (vasculitis).
From the hematopoietic organs: leukopenia, agranulocytosis, anemia, thrombocytopenia, pancytopenia, hemolytic and aplastic anemia.
From the urinary system: acute interstitial nephritis, impaired renal function, hypercreatininemia, increased urea concentration.
Other: intestinal dysbiosis, superinfection, hypoglycemia (in patients with diabetes) vaginitis.
Interaction
Interaction
Antacids containing aluminum hydroxide (including sucralfate) and magnesium hydroxide, aluminum phosphate, zinc iron, reduce the absorption of ofloxacin. When taking antacids and ofloxacin, an interval of approximately two hours should be maintained between doses.
When using vitamin K antagonists simultaneously, monitoring of the blood coagulation system is necessary.
Ofloxacin may slightly increase serum concentrations of glibenclamide when used concomitantly.
In the case of using high doses of ofloxacin and other drugs eliminated by renal tubular secretion such as probenecid cimetidine furosemide or methotrexate, an increase in the concentration of ofloxacin in the blood serum is possible.
A noticeable decrease in the threshold for seizure activity can be observed when fluoroquinolones are prescribed in combination with theophylline, fenbufen or other non-steroidal anti-inflammatory drugs, as well as other drugs that lower the threshold for seizure activity.
When prescribed together with non-steroidal anti-inflammatory drugs, derivatives of nitroimidazole and methylxanthines, the risk of developing neurotoxic effects increases.
When prescribed simultaneously with glucocorticosteroids, the risk of tendon rupture increases, especially in older people.
When co-administered with drugs that prolong the QT interval (class IA and III antiarrhythmic drugs, tricyclic antidepressants, macrolides), the risk of prolongation of the QT interval increases.
When prescribed with drugs that alkalinize urine (carbonic anhydrase inhibitors, sodium bicarbonate citrates), the risk of crystalluria and nephrotoxic effects increases.
Overdose
Overdose
Symptoms: dizziness, confusion, lethargy, disorientation, drowsiness, vomiting.
In case of overdose, it is recommended to perform gastric lavage and symptomatic therapy. There is no specific antidote.
Storage conditions
Storage conditions
In a place protected from light, at a temperature of 15–25 °C. Freezing is unacceptable.
Shelf life
Shelf life
3 years. Do not use after expiration date.
Manufacturer
Manufacturer
Ozon, Russia
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | In a light-protected place at 15-25 °C. Freezing is not allowed. |
| Manufacturer | Ozon, Russia |
| Medication form | pills |
| Brand | Ozon |
Other forms…
Related products
Buy Ofloxacin, 400 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.