No products in the cart.
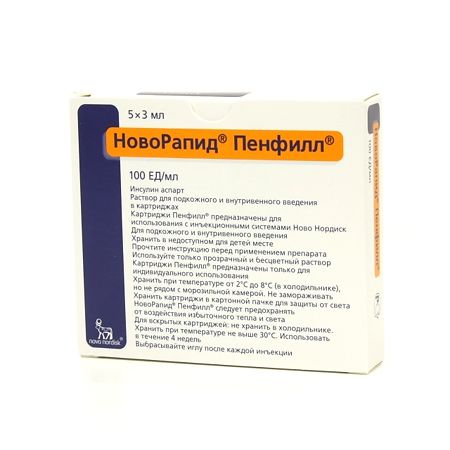
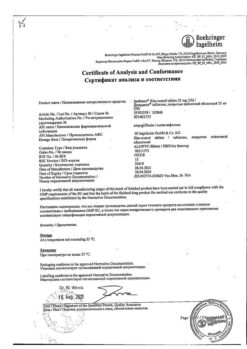
NovoRapid Penfill, 100 me/ml cartridges 3 ml, 5 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
NovoRapid Penfill is hypoglycemic.
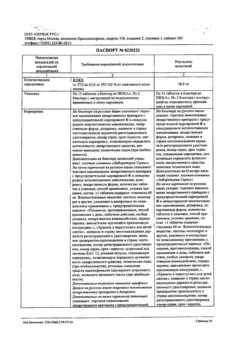
Pharmacodynamics
Insulin aspart is an analogue of human insulin short-acting, produced by recombinant DNA biotechnology using Saccharomyces cerevisiae strain, in which the amino acid proline in position B28 is replaced with asparagic acid.
It interacts with specific receptor on outer cytoplasmic cell membrane and forms insulin-receptor complex, stimulating intracellular processes, including synthesis of several key enzymes (including hexokinase, pyruvate kinase, glycogen synthase). Decrease of glucose content in blood is conditioned by increase of its intracellular transport, increase of absorption by tissues, stimulation of lipogenesis, glycogenogenesis, decrease of glucose production by liver.
The substitution of the amino acid proline at position B28 for asparagic acid in insulin aspart reduces the tendency of molecules to form hexamers, which is observed in regular insulin solution. Aspart insulin is therefore absorbed much faster from the subcutaneous fatty tissue and takes effect faster than soluble human insulin. Insulin aspart more strongly reduces blood glucose in the first 4 hours after a meal than soluble human insulin. The duration of action of aspart insulin after injection is shorter than that of soluble human insulin.
Injection of Aspart within 10-20 minutes after injection. Maximum effect is observed 1-3 hours after injection. The duration of action of the drug is 3-5 hours.
Clinical studies with patients with type 1 diabetes have demonstrated decreased risk of nocturnal hypoglycemia with aspart insulin compared to soluble human insulin. The risk of daytime hypoglycemia was not significantly increased.
Aspart insulin is equipotential to soluble human insulin based on molarity values.
Adults. Clinical studies involving patients with type 1 diabetes demonstrate lower postprandial blood glucose concentrations with insulin aspart compared to soluble human insulin.
Elderly. A randomized, double-blind, cross-over study of the pharmacokinetics and pharmacodynamics (PK/PD) of aspart insulin and soluble human insulin was performed in elderly patients with type 2 diabetes (19 patients aged 65-83 years, mean age 70 years). The relative differences in pharmacodynamic properties between aspart insulin and soluble human insulin in elderly patients were similar to those in healthy volunteers and in younger diabetic patients.
Children and adolescents. Aspart insulin use in children showed similar long-term glycemic control results when compared to soluble human insulin.
A clinical study using soluble human insulin before meals and insulin aspart after meals was conducted in young children (26 patients aged 2 to 6 years); and an FK/FD study using a single dose was conducted in children (6-12 years) and adolescents (13-17 years). The pharmacodynamic profile of insulin aspart in children was similar to that of adult patients.
Pregnancy. Clinical studies comparing safety and efficacy of insulin aspart and human insulin in the treatment of pregnant women with type 1 diabetes (322 pregnant women studied, of whom 157 received insulin aspart and 165 received human insulin) showed no adverse effects of insulin aspart on pregnancy or fetal/newborn health.
An additional clinical trial of 27 women with gestational diabetes receiving aspart insulin and human insulin (14 women received aspart insulin and 13 received human insulin) showed comparable safety profiles along with a significant improvement in postprandial glucose control with aspart insulin treatment.
Preclinical safety data
Preclinical studies have not identified any risk to humans based on data from generally accepted studies of pharmacological safety, repeat use toxicity, genotoxicity and reproductive toxicity.
In in vitro tests, including binding to insulin and insulin-like growth factor-1 receptors and effects on cell growth, the behavior of aspart insulin is very similar to that of human insulin. Studies have also shown that the dissociation of insulin aspart from the insulin receptor is equivalent to that of human insulin.
Pharmacokinetics
After p/k administration of aspart insulin, Tmax in plasma is on average 2 times less than after administration of soluble human insulin. Cmax in plasma averages (492±256) pmol/L and is reached 40 min after a 0.15 units/kg dose of p/c in patients with type 1 diabetes. Insulin concentration returns to baseline 4-6 h after drug administration. The absorption rate is slightly lower in patients with type 2 diabetes, resulting in a lower maximum concentration of (352±240) pmol/L and a longer Tmax (60 min). Intraindividual variability in Tmax is significantly lower with aspart insulin compared with soluble human insulin, whereas the indicated variability in Cmax is greater for aspart insulin.
Pharmacokinetics in children (6-12 years) and adolescents (13-17 years) with type 1 diabetes.Absorption of insulin aspart is rapid in both age groups with Tmax similar to that of adults. However, there are differences in Cmax in the two age groups, which emphasizes the importance of individual dosing of the drug.
Elderly. The relative differences in pharmacokinetics between insulin aspart and soluble human insulin in elderly patients (65-83 years, mean age 70 years) with type 2 diabetes were similar to those in healthy volunteers and in younger diabetic patients. Older patients had a decreased absorption rate, resulting in an increased Tmax of 82 (variability 60-120) minutes, whereas Cmax was similar to that observed in younger patients with type 2 diabetes and slightly less than that observed in patients with type 1 diabetes.
Liver function insufficiency. A pharmacokinetic study was performed on a single dose of Aspart insulin in 24 patients whose liver function ranged from normal to severe impairment. In those with impaired liver function, the absorption rate of aspart insulin was reduced and more erratic, resulting in an increase in Tmax from approximately 50 minutes in those with normal liver function to approximately 85 minutes in those with moderate to severe liver function impairment. AUC, Cmax in plasma, and total clearance (Cl/F) were similar in subjects with impaired and normal liver function.
Inadequate renal function. A study was performed on the pharmacokinetics of insulin aspart in 18 patients whose renal function ranged from normal to severe impairment. There was no apparent effect of creatinine Cl value on the AUC, Cmax, Tmax of insulin aspart. Data were limited to those with moderate to severe renal impairment. Individuals with renal impairment requiring dialysis were not included in the study.
Indications
Indications
Diabetes mellitus in adults, adolescents and children over 2 years old.
Active ingredient
Active ingredient
Composition
Composition
Active ingredient:
Aspart 100 IU (3.5 mg) insulin;
Supplements:
Glycerol – 16 mg;
Phenol – 1.5 mg;
methacresol, 1.72 mg;
Zinc chloride, 19.6 µg;
Sodium chloride, 0.58 mg;
p> sodium hydrophosphate dihydrate – 1.25 mg;
sodium hydroxide 2M – about 2.2 mg;
sodium hydroxide
Hydrochloric acid 2M – about 1.7 mg;
Injection water – up to 1 ml
How to take, the dosage
How to take, the dosage
Intravenously, intravenously.
NovoRapid® Penfill® is a fast-acting analogue of insulin. The dose of NovoRapid® Penfill® is determined by the doctor individually, according to the patient’s needs. Usually the drug is used in combination with medium- or long-acting insulin preparations, which are administered at least once a day. To achieve optimal glycemic control, it is recommended to measure blood glucose concentration regularly and adjust insulin dose.
In adults and children, the normal daily requirement for insulin is 0.5 to 1 unit/kg of body weight. When administered before meals, the requirement for insulin may be satisfied by NovoRapid ® Penfill by 50-70%; the remaining requirement for insulin is satisfied by insulin prolonged action. Increased physical activity, changes in dietary habits, or comorbidities may necessitate dose adjustments.
The NovoRapid® Penfill® has a faster onset and shorter duration of action than soluble human insulin. Because of its faster onset of action, NovoRapid®Penfill® should generally be administered immediately before a meal; if necessary, it may be administered soon after a meal.
Due to the shorter duration of action compared to human insulin, patients receiving NovoRapid® Penfill® have a lower risk of developing nocturnal hypoglycemia.
Particular patient groups. As with other insulin preparations, elderly patients and patients with renal or hepatic impairment should have their blood glucose concentrations monitored more closely and the dose of Aspart insulin adjusted individually.
Children and adolescents. NovoRapid® Penfill® is preferred over soluble human insulin in children when a rapid onset of action is needed, such as when the child has difficulty maintaining the required time interval between injections and meals.
Transfer from other insulin medications. When transferring a patient from other insulin products to NovoRapid® Penfill® doses of NovoRapid® Penfill® and basal insulin may need to be adjusted.
The NovoRapid® Penfill® is injected p/k into the anterior abdominal wall, thigh, shoulder, deltoid or gluteal area. The injection sites within the same body area should be changed regularly to reduce the risk of lipodystrophy. As with all insulin preparations, p/c injection into the anterior abdominal wall provides faster absorption compared to administration at other sites. Duration of action depends on dose, site of administration, blood flow, temperature, and level of physical activity. However, the faster onset of action compared to soluble human insulin persists regardless of injection site localization.
NovoRapid® can be used for prolonged subcutaneous insulin infusions (SPII) in insulin pumps designed for insulin infusions. The PIPI should be given into the anterior abdominal wall. The infusion sites should be changed periodically.
When using an insulin infusion pump, NovoRapid® should not be mixed with other types of insulin.
Patients using an RPI must be fully trained in the use of the pump, the appropriate reservoir and the pump tubing system. The infusion set (tubing and catheter) should be replaced according to the user manual included with the infusion set.
Patients receiving NovoRapid® with a PPI should have extra insulin available in case the infusion system fails.
Intravenous administration. If necessary, NovoRapid® may be administered by IV, but only by qualified medical personnel.
Infusion systems with NovoRapid® are used for intravenous administration 100 IU/ml with a concentration of 0.05 to 1 IU/ml of insulin aspart in 0.9% sodium chloride solution, 5 or 10% dextrose solution containing 40 mmol/L potassium chloride, using polypropylene infusion containers. These solutions are stable at room temperature for 24 h. Although stable for some time, a certain amount of insulin is initially absorbed by the material of the infusion system. Blood glucose concentrations must be monitored continuously during insulin infusions.
Interaction
Interaction
There are a number of drugs that affect the need for insulin. Hypoglycemic effect of insulin is enhanced by oral hypoglycemic drugs, MAO inhibitors, ACE inhibitors, carbohydrate inhibitors, non-selective beta-adrenoblockers, bromocriptine, sulfonamides, anabolic steroids, tetracyclines, clofibrate, ketoconazole, mebendazole, pyridoxine, theophylline, cyclophosphamide, phenfluramine, lithium preparations, salicylates.
The hypoglycemic effects of insulin are impaired by oral contraceptives, GCS, thyroid hormones, thiazide diuretics, heparin, tricyclic antidepressants, sympathomimetics, somatropin, danazol, clonidine, BKK, diazoxide, morphine, phenytoin, nicotine.
Beta-adrenoblockers may mask symptoms of hypoglycemia.
Octreotide/lanreotide can both increase and decrease the need for insulin.
Alcohol can both increase and decrease the hypoglycemic effect of insulin.
Incompatibilities. Some drugs, such as those containing thiol or sulfite groups, when added to NovoRapid® Penfill® may cause destruction of insulin aspart. NovoRapid® Penfill® should not be mixed with other drugs. The exceptions are isophane-insulin and solutions for infusion.
Special Instructions
Special Instructions
Patients should consult with their physician before traveling for an extended period of time because a change in time zone means the patient must eat and inject insulin at a different time.
Hyperglycemia. An insufficient dose of medication or discontinuation of treatment, especially in type 1 diabetes, can lead to the development of hyperglycemia and diabetic ketoacidosis. Typically, symptoms of hyperglycemia appear gradually over a period of hours or days. Symptoms of hyperglycemia include nausea, vomiting, drowsiness, red and dry skin, dry mouth, increased urine output, thirst and loss of appetite, and the smell of acetone in the exhaled air. Without appropriate treatment, hyperglycemia can lead to death.
Hypoglycemia. Skipping a meal, unplanned increased physical activity, or an insulin dose that is too high relative to the patient’s need can lead to hypoglycemia. After compensation of carbohydrate metabolism, e.g. with intensified insulin therapy, typical precursor symptoms of hypoglycemia may change and patients should be informed about them. Common precursor symptoms may disappear with the long-term course of diabetes mellitus.
The consequence of the pharmacodynamic characteristics of short-acting insulin analogues is that the development of hypoglycemia with their use may begin earlier than with soluble human insulin.
As NovoRapid® Penfill® must be used directly in conjunction with food intake, the high rate of onset of the drug effect must be considered when treating patients with comorbidities or those taking drugs that slow the absorption of food.
Concomitant diseases, especially infectious and accompanied with fever, usually increase the body’s need for insulin. Correction of the drug dose may also be necessary if the patient has concomitant kidney, liver, adrenal, pituitary, or thyroid disorders.
If the patient is switched to other types of insulin, the early precursor symptoms of hypoglycemia may become less severe compared to those with the previous type of insulin.
Transferring a patient from other insulin preparations. Conversion of a patient to a new type of insulin or another manufacturer’s insulin medication must be done under strict medical supervision. Changes in concentration, type, manufacturer, and type (human insulin, animal insulin, human insulin analogues) of insulin preparations and/or method of manufacture may require a change in dose or increased frequency of injections compared to the previously used insulin preparations. If a dose adjustment is necessary, it may be made as early as the first administration of the drug or during the first weeks or months of treatment.
Injection site reactions. As with other insulin drugs, injection site reactions may develop, as manifested by pain, redness, urticaria, inflammation, bruising, swelling, and itching. Regularly changing the injection site in the same anatomical area can reduce symptoms or prevent the development of reactions. In very rare cases, NovoRapid® Penfill® may need to be stopped.
The concomitant use of thiazolidinedione group drugs and insulin drugs has been reported in cases of chronic heart failure when treating patients with thiazolidinedione in combination with insulin drugs, especially if such patients have risk factors for chronic heart failure. This fact should be taken into account when prescribing combined therapy with thiazolidinediones and insulin drugs. When prescribing such combination therapy, medical examination of patients should be carried out to detect signs and symptoms of chronic heart failure, weight gain and edema. If patients have worsening symptoms of heart failure, treatment with thiazolidinedione should be discontinued.
Impact on the ability to drive vehicles and operate mechanisms.Patients’ ability to concentrate and reaction speed may be impaired during hypoglycemia, which may be dangerous in situations where these abilities are particularly necessary (e.g., when driving or operating machines and mechanisms). Patients should be advised to take measures to prevent the development of hypoglycemia when driving vehicles and working with mechanisms. This is especially important for patients with no or reduced symptom precursors of developing hypoglycemia or who have frequent episodes of hypoglycemia.
Contraindications
Contraindications
Hypersensitivity to insulin aspart or any of the components of the drug.
The use of NovoRapid® Penfill® in children under 2 years of age is not recommended since no clinical studies have been performed in children under 2 years of age.
Overdose
Overdose
Symptoms. No specific dose required for insulin overdose has been established, but hypoglycemia may develop gradually if doses too high relative to the patient’s need are administered.
Treatment. Mild hypoglycemia can be managed by the patient himself by ingesting glucose or sugary foods. Therefore, it is recommended that diabetics carry sugary foods with them at all times.
In case of severe hypoglycemia, when the patient is unconscious, 0.5 mg to 1 mg of glucagon should be administered by injection or by injection (a trained person can administer it), or an intravenous glucose (dextrose) solution (only a medical professional can administer it). Dextrose should also be administered intravenously if the patient does not regain consciousness 10-15 minutes after glucagon administration. After recovery of consciousness, the patient is advised to take carbohydrate-rich food to prevent recurrence of hypoglycemia.
Additional information
| Shelf life | 30 months |
|---|---|
| Conditions of storage | At 2-8 °C (in the refrigerator) |
| Manufacturer | Novo Nordisk A/S, Denmark |
| Medication form | solution for injection |
| Brand | Novo Nordisk A/S |
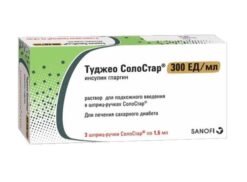
Related products
Buy NovoRapid Penfill, 100 me/ml cartridges 3 ml, 5 pcs. with delivery to USA, UK, Europe and over 120 other countries.