No products in the cart.
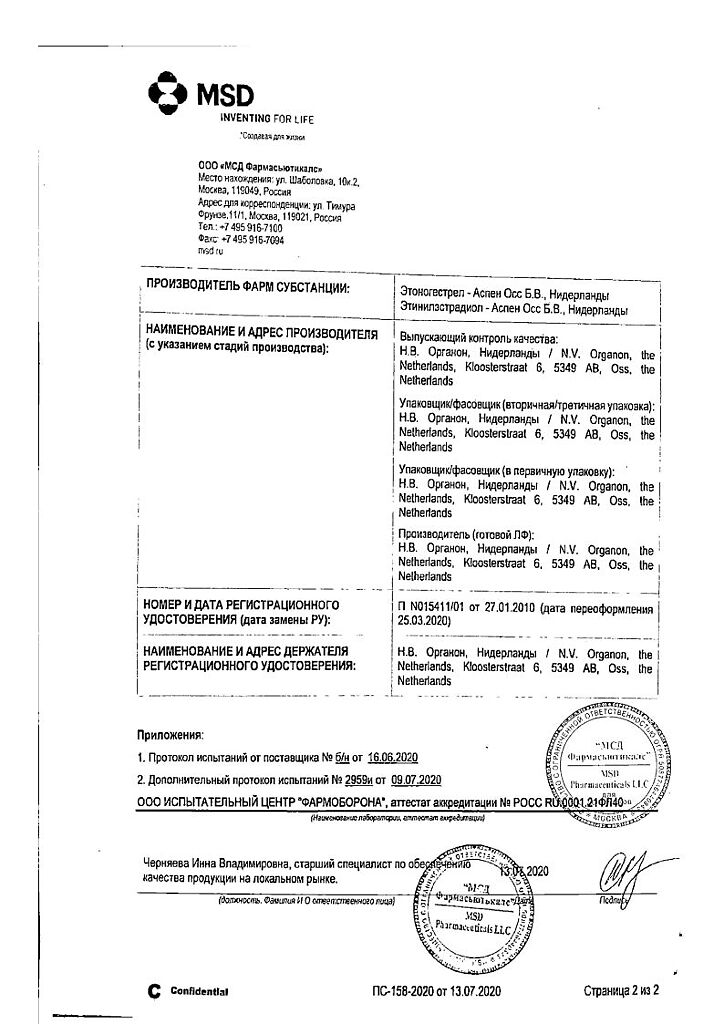
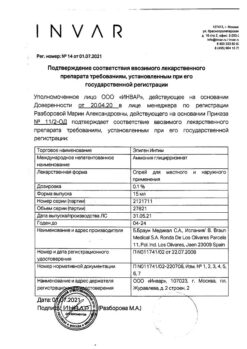
NovaRing, vaginal rings 0.015 mg+0.120 mg/day 3 pcs
€129.37 €107.81
Out of stock
(E-mail when Stock is available)
EAN: 4601910000522
SKU: 206792
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Pharmacodynamics
NovaRing® is a hormonal combined contraceptive containing etonogestrel and ethinylestradiol. Etonogestrel is a progestagen (a derivative of 19-nortestosterone) that binds with high affinity to progesterone receptors in target organs. Ethinyl estradiol is an estrogen and is widely used to produce contraceptives.
The contraceptive effect of NovaRing® is due to a combination of different factors, the most important of which is suppression of ovulation.
Effectiveness
In clinical studies, the Perl index (a measure of the frequency of pregnancy in 100 women over 1 year of contraception) for NovaRing® was found to be 0.96 (95% CI: 0.64-1.39) and 0.64 (95% CI: 0.35-1.07) in statistical analyses of all randomized participants (ITT analyses) and analyses of study participants who completed them according to protocol (PP analyses), respectively. These values were similar to the Perl index values obtained in comparative studies of combined oral contraceptives (OCs) containing levonorgestrel/ethinylestradiol (0.150/0.030 mg) or drospirenone/ethinylestradiol (3/0.30 mg).
The use of NovaRing® makes the cycle more regular, reduces the pain and intensity of menstrual bleeding, which helps to reduce the incidence of iron deficiency. There is data on reduction of risk of endometrial and ovarian cancer during use of the drug.
The nature of bleeding
. A one-year comparison of bleeding patterns in 1000 women using NovaRing® and OCs containing levonorgestrel/ethinylestradiol (0.150/0.030 mg) showed significantly lower rates of breakthrough bleeding or smeary bleeding with NovaRing® compared to OCs. In addition, the incidence of bleeding occurring only during a break in use was significantly higher among women using NovaRing®.
Effects on bone mineral density
A comparative two-year study of the effects of NovaRing® (n=76) and the non-hormonal IUD (n=31) showed no effect on bone mineral density in women.
Children
The safety and effectiveness of NovaRing® for adolescent girls under 18 years of age has not been studied.
Pharmacokinetics
Etonogestrel
absorption
The etonogestrel released from the NovaRing® vaginal ring is rapidly absorbed through the vaginal mucosa. The maximum plasma concentration of etonogestrel, about 1700 pg/ml, is reached about 1 week after the insertion of the ring. Plasma concentrations vary over a small range and slowly decrease to about 1600 pg/mL after 1 week, 1500 pg/mL after 2 weeks, and 1400 pg/mL after 3 weeks of use. Absolute bioavailability is about 100%, which exceeds bioavailability with oral administration of etonogestrel. According to the results of measurements of cervical and intrauterine concentrations of etonogestrel in women using NovaRing® and women using oral contraceptives containing 0.150 mg of desogestrel and 0.020 mg of ethinylestradiol, the observed values of etonogestrel concentrations were comparable.
Distribution
Atonogestrel binds to plasma albumin and sex hormone binding globulin (hGHB). The apparent volume of distribution of etonogestrel is 2.3 L/kg.
Metabolism
Biotransformation of etonogestrel occurs by the known pathways of sex hormone metabolism. The apparent blood plasma clearance is about 3.5 L/h. No direct interaction with ethinylestradiol taken simultaneously has been revealed.
Evacuation
The plasma concentrations of etonogestrel decrease in two phases. In the terminal phase, the elimination half-life is approximately 29 h. Etonogestrel and its metabolites are excreted by the kidneys and through the intestine with the bile at a ratio of about 1.7:1. The elimination half-life of metabolites is about 6 days.
Ethinylestradiol
absorption
Ethinylestradiol released from the NovaRing® vaginal ring is rapidly absorbed through the vaginal mucosa. The maximum plasma concentration of approximately 35 pg/ml is reached 3 days after ring insertion and decreases to 19 pg/ml after 1 week, to 18 pg/ml after 2 weeks and 18 pg/ml after 3 weeks of use. Absolute bioavailability is approximately 56% and is comparable to that of oral ethinylestradiol. According to the results of measurements of cervical and intrauterine ethinylestradiol concentrations in women using NovaRing® and women using oral contraceptives containing 0.150 mg of desogestrel and 0.020 mg of ethinylestradiol, the observed values of ethinylestradiol concentrations were comparable.
Ethinylestradiol concentrations were studied in a comparative randomized trial of NovaRing® (vaginal daily release of ethinylestradiol 0.015 mg), a transdermal patch (norelgestromin/ethinylestradiol; daily ethinylestradiol release 0.020 mg) and OCs (levonorgestrel/ethinylestradiol; daily ethinylestradiol release 0.030 mg) during one cycle in healthy women. Systemic exposure to ethinylestradiol over one month (AUC 0-∞) for NovaRing® was statistically significantly lower than for the patch and OC, at 10.9, 37.4, and 22.5 ng/h/mL, respectively.
Distribution
Ethinylestradiol binds nonspecifically to plasma albumin. The apparent volume of distribution is about 15 l/kg.
Metabolism
Ethinylestradiol is metabolized by aromatic hydroxylation. Its biotransformation produces a large number of hydroxylated and methylated metabolites. They circulate in free form or as sulfate and glucuronide conjugates. The apparent clearance is approximately 35 l/h.
Elimation
The plasma concentrations of ethinylestradiol decrease in two phases. The terminal phase elimination half-life varies widely; the median is about 34 h. Ethinylestradiol is not excreted unchanged. Metabolites of ethinylestradiol are excreted by the kidneys and through the intestine with the bile at a ratio of 1.3:1. The elimination half-life of metabolites is about 1.5 days.
Special patient groups
Children
The pharmacokinetics of NovaRing® in healthy adolescent girls under 18 years of age who have already menstruated have not been studied.
Renal dysfunction
The effect of renal disease on the pharmacokinetics of NovaRing® has not been studied.
Hepatic dysfunction
The effect of liver disease on the pharmacokinetics of NovaRing® has not been studied. However, patients with liver dysfunction may have impaired sex hormone metabolism.
Ethnic groups
The pharmacokinetics of the drug in ethnic groups have not been specifically studied.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Active ingredients:
Etonogestrel, 11.7 mg;
Ethinylestradiol, 2.7 mg.
Auxiliary substances:
Ethylene and vinyl acetate copolymer (28% vinyl acetate) – 1677 mg;
Ethylene and vinyl acetate copolymer (9% vinyl acetate) – 197 mg;
Magnesium stearate – 1.7 mg.
How to take, the dosage
How to take, the dosage
In order to achieve the contraceptive effect, NovaRing® must be used according to the instructions.
The woman can insert the NovaRing® vaginal ring into the vagina on her own.
The physician should inform the woman how to insert and remove the NovaRing® vaginal ring. The woman should choose a comfortable position to insert the ring, such as standing with one leg raised, squatting or lying down. The NovaRing® vaginal ring should be squeezed and inserted into the vagina until the ring is in a comfortable position. The exact position of the ring in the vagina is not decisive for the contraceptive effect.
After insertion (see “How to start using NovaRing®”) the ring must remain in the vagina for 3 weeks. It is advisable for the woman to check regularly whether it remains in the vagina. If the ring is accidentally removed, follow the instructions in “What to do if the ring has been temporarily removed from the vagina.
The NovaRing® vaginal ring should be removed after 3 weeks on the same day of the week that the ring was inserted into the vagina. After a one-week break, a new ring is inserted (e.g., if the NovaRing® vaginal ring was inserted on Wednesday at approximately 10 p.m., it should be removed on Wednesday after 3 weeks at approximately 10 p.m. A new ring is inserted the following Wednesday). To remove the ring, you must pick it up with your index finger or squeeze it with your index and middle finger and pull it out of the vagina. The used ring should be placed in a bag (keep it out of reach of children and pets) and thrown away. Bleeding associated with discontinuation of NovaRing® usually begins 2-3 days after removal of the NovaRing® vaginal ring and may not completely stop until a new ring is placed.
How do I start NovaRing®?
Hormonal contraceptives were not used in the previous cycle
NovaRing® should be inserted on the first day of the cycle (i.e. the first day of menstruation). It is allowed to insert the ring on days 2-5 of the cycle, but in the first cycle in the first 7 days of using NovaRing® additional use of barrier contraceptive methods is recommended.
Transition from combined hormonal contraceptives
A woman should insert the NovaRing® vaginal ring on the last day of the usual interval between cycles in taking combined hormonal contraceptives (pills or patch).
If a woman has taken a combined hormonal contraceptive correctly and regularly and is confident that she is not pregnant, she may switch to using a vaginal ring on any day of her cycle. Under no circumstances should she exceed the recommended hormone-free interval of the previous method.
Transitioning from progestogen-only products (mini-pills, progestin oral contraceptives, implants, injectable forms, or hormone-containing IUDs)
A woman taking mini-pills or progestin oral contraceptives may switch to NovaRing® any day. The ring is inserted on the day the implant or IUD is removed. If the woman has received injections, NovaRing® is started on the day the next injection should have been given. In all these cases, the woman must use a barrier method of contraception for the first 7 days after insertion of the ring.
After a first trimester abortion
The woman can insert the ring immediately after the abortion. In this case, she does not need additional contraceptives. If use of NovaRing® immediately after the abortion is undesirable, the recommendations in the subsection “No hormonal contraceptives used in the previous cycle” should be followed. An alternative method of contraception is recommended for the woman in the interval.
After childbirth or after a second trimester abortion
The woman is advised to insert the ring no earlier than 4 weeks after childbirth (if she is not breastfeeding) or a second trimester abortion. If the ring is inserted at a later date, the use of an additional barrier method for the first 7 days is recommended. However, if sexual intercourse has already occurred, it is necessary to rule out pregnancy or wait until the first menstrual period before using NovaRing®.
Deviations from the recommended regimen
The contraceptive effect and cycle control may be compromised if the woman does not adhere to the recommended regimen. The following recommendations should be followed to avoid reduced contraceptive effect.
What to do if your ring break is too long?
If you have had sex during your ring break, you should always rule out pregnancy. The longer the interval, the greater the chance of pregnancy. If pregnancy is ruled out, a woman should insert a new ring into her vagina as soon as possible. During the next 7 days an additional barrier method of contraception, such as a condom, should be used.
What to do if the ring has been temporarily removed from the vagina?
The ring must remain in the vagina for 3 weeks at all times. If the ring is accidentally removed, it should be rinsed with cold or slightly warm (not hot) water and immediately inserted into the vagina.
What if I use the ring extensively?
If NovaRing® was not used for more than the maximum four weeks, the contraceptive effect remains adequate. A woman can take a one-week break from using the ring and then insert a new ring.
If a NovaRing® vaginal ring is left in the vagina for more than 4 weeks, the contraceptive effect may worsen, so pregnancy should be ruled out before a new ring is inserted.
If a woman does not adhere to the recommended pattern of use and no bleeding occurs after a one-week break in use of the ring, pregnancy should be ruled out before inserting a new ring.
How can I delay or defer menstrual bleeding?
In order to delay menstrual bleeding cancellation, women can insert a new ring without a one-week break. The next ring must be used within 3 weeks. At this time, there may be some spotting or bleeding. Then, after the usual one-week break the woman returns to regular use of NovaRing®.
In order to postpone the start of bleeding to another day of the week, a woman may be advised to take a shorter break from the ring (as many days as necessary). The shorter the interval, the more likely it is that there will be no bleeding when the ring is removed and that there will be no bleeding or spotting when the next ring is used.
Interaction
Interaction
Interactions with other drugs
Interactions between hormonal contraceptives and other drugs can lead to acyclic bleeding and/or contraceptive failure. The following interactions with combined oral contraceptives in general have been described in the literature.
Help metabolism: Can have interactions with drugs that induce microsomal liver enzymes, which may lead to increased clearance of sex hormones. Interactions have been found, for example, with phenytoin, barbiturates, primidone, carbamazepine, rifampicin, and possibly also with oxcarbazepine, topiramate, felbamate, ritonavir, griseofulvin and preparations containing St. John’s wort (Hypericum perforatum).
Treatment with any of the drugs listed should be treated temporarily with a barrier method of contraception (condom) in combination with NovaRing® or choose another method of contraception. During concomitant use of drugs that induce microsomal enzymes and for 28 days after their withdrawal, barrier contraceptive methods should be used.
If the concomitant therapy must be continued after 3 weeks of use of the ring, the next ring must be inserted immediately without the usual interval.
Antibiotics: Decreased efficacy of oral contraceptives containing ethinyl estradiol has been noted with concomitant administration of antibiotics such as ampicillin and tetracyclines. The mechanism of this effect is not understood. In a study of pharmacokinetic interactions, oral administration of amoxicillin (875 mg, twice daily) or doxycycline (200 mg daily and then 100 mg daily) for 10 days during administration of NovaRing® had little effect on the pharmacokinetics of etonogestrel and ethinylestradiol. If antibiotics (excluding amoxicillin and doxycycline) are used, a barrier method of contraception (condom) should be used during treatment and for 7 days after withdrawal of antibiotics. If concomitant therapy should be continued after 3 weeks of ring use, the next ring should be inserted immediately without the usual interval. Pharmacokinetic studies have shown no effect of concomitant use of antifungal agents and spermicides on the contraceptive efficacy and safety of NovaRing®. When the suppositories are used concomitantly with antifungal drugs, the risk of ring rupture is slightly increased. Hormonal contraceptives may cause metabolic disorders of other drugs. Accordingly, their concentrations in plasma and tissues may increase (e.g., cyclosporine) or decrease (e.g., lamotrigine). To exclude possible interaction it is necessary to read the instructions for use of other drugs.
Laboratory studies
The use of contraceptive hormonal drugs may affect the results of certain laboratory tests, including biochemical measures of liver, thyroid, adrenal and renal function; plasma concentrations of transport proteins such as corticosteroid-binding globulin (CRBG) and hCG; lipid/lipoprotein fractions; carbohydrate metabolites; and clotting and fibrinolysis. The indexes tend to change within normal values.
Combined use with tampons
Pharmacokinetic data demonstrate that tampon use has no effect on absorption of hormones released from the NovaRing® vaginal ring. In rare cases the ring may be accidentally removed during tampon extraction (see subsection “What to do if the ring has been temporarily removed from the vagina” in the section “Dosage and administration”).
Special Instructions
Special Instructions
In the presence of any of the following diseases, conditions or risk factors, the benefits of NovaRing® and the possible risks to each individual woman should be evaluated before starting NovaRing®. If any of the following conditions worsen, worsen, or occur for the first time, women should see their physician to determine whether NovaRing® can be continued.
Circulatory disorders
Hormonal contraceptive use may be associated with venous thrombosis (deep vein thrombosis and pulmonary embolism) and arterial thrombosis and related complications, sometimes with death.
The use of any OCs increases the risk of venous thromboembolism (VTE) compared with the risk of VTE in patients not using OCs. The risk of VTE is highest in the first year of OC use. Data from a large prospective cohort study on the safety of different OCs suggest that the greatest increase in risk, compared with the risk in women not using OCs, is in the first 6 months after starting OCs or resuming use after a break (4 weeks or longer). In nonpregnant women not using oral contraceptives, the risk of VTE is 1 to 5 cases per 10,000 women-years (WL). In women using oral contraceptives, the risk of VTE is 3 to 9 cases per 10,000 WL. The increased risk is less than in pregnancy, where the risk is 5 to 20 cases per 10,000 WL (pregnancy data are based on the actual duration of pregnancy in standardized studies; based on the assumption that pregnancy lasts 9 months, the risk is 7 to 27 cases per 10,000 WL). In postpartum women, the risk of VTE is 40 to 65 cases per 10,000 VL. VTE is fatal in 1-2% of cases.
The studies show an increased risk of VTE in women using NovaRing® that is similar to that of women using OCs (see table below for adjusted risk ratio). A large prospective observational TASC (Transatlantic Active Study of Cardiovascular Safety with NovaRing®) study evaluated the risk of VTE in women who started NovaRing® or OC, switched to NovaRing® or OC from other contraceptives, or resumed NovaRing® or OC in a typical user population. Women were followed for 24 to 48 months. The results showed a similar risk of VTE in women using NovaRing® (incidence 8.3 per 10,000 LL) and in women using OCs (incidence 9.2 per 10,000 LL). For women using OCs other than those containing desogestrel, gestoden, and drospirenone, the incidence of VTE was 8.5 cases per 10,000 LL.
A FDA-initiated retrospective cohort study showed that women who began NovaRing® had a VTE rate of 11.4 per 10,000 LL compared to 9.2 per 10,000 LL for women who began levonorgestrel OCs.
Risk assessment (risk ratio) of VTE in women using NovaRing® compared with the risk of VTE in women using OC
The epidemiological study, population:
The comparison drug(s):
Ratio (OR) (95% CI):
1 – Including low-dose OCs containing the following progestins: chlormadinone acetate, cyproterone acetate, desogestrel, dienogestrone, drospirenone, ethinodiol diacetate, gestoden, levonorgestrel, norethindrone, norgestimat or norgestrel.
2 – Taking into account age, BMI, duration of use, history of VTE.
3 – Including low-dose OCs containing the following progestins: norgestimat, norethindrone, or levonorgestrel.
4 – Taking into account age, place, and year of study inclusion.
In extremely rare cases of thrombosis of other blood vessels (e.g., hepatic arteries and veins, mesenteric vessels, kidneys, brain, and retina) with OC use are known. It is not known whether these cases are related to the use of OCs.
Possible symptoms of venous or arterial thrombosis may include unilateral swelling and/or pain in the lower extremity, localized fever in the lower extremity, hyperemia or discoloration of the skin on the lower extremity; sudden severe chest pain, possibly irradiating to the left arm; an attack of shortness of breath, coughing Any unusual, severe, prolonged headache; sudden partial or total loss of vision; double vision; slurred speech or aphasia; dizziness; collapse, with or without a focal seizure; sudden weakness or marked numbness on one side or any part of the body; motor disturbances; “acute” abdomen.
Risk factors for venous thromboses and embolisms:
There is no consensus about the possible role of these conditions in the etiology of venous thrombosis.
Risk factors for arterial thromboembolic complications:
Other conditions that may lead to unwanted circulatory disturbances include diabetes mellitus, systemic lupus erythematosus, hemolytic-uremic syndrome and chronic inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), and sickle cell anemia.
An increased risk of thromboembolism in the postpartum period should be considered. An increase in the frequency or severity of migraines (which may be a prodromal symptom of cerebrovascular disorders) during use of hormonal contraceptives may be a reason for immediate discontinuation of hormonal contraceptives.
Women using CGC should be advised to consult a physician if possible symptoms of thrombosis occur. If thrombosis is suspected or confirmed, the use of CGC should be discontinued. Effective contraception should be used because anticoagulants (coumarins) have teratogenic effects.
Tumor Risk
The most important risk factor for cervical cancer is infection with human papillomavirus (HPV). Epidemiological studies have shown that prolonged use of OCs further increases this risk, but it is unclear how this is related to other factors, such as more frequent cervical smears and differences in sexual behavior, including use of barrier contraceptives. It remains unclear how this effect is related to the use of NovaRing®.
A meta-analysis of results from 54 epidemiologic studies found a small increase (1.24) in the relative risk of breast cancer in women taking combined hormonal oral contraceptives. The risk gradually declines over a 10 year period after withdrawal. Breast cancer rarely develops in women under the age of 40, so the additional incidence of breast cancer in women who are taking or have taken OCs is small compared to the overall risk of developing breast cancer. The breast cancer diagnosed in women who use OCs is clinically less severe than the cancer diagnosed in women who have never used OCs. The increased risk of breast cancer may be due to either the earlier diagnosis of breast cancer in women who use OC, or to the biological effects of OC, or a combination of both.
In rare cases, women who took OC have developed benign, and even more rarely, malignant liver tumors. In some cases, these tumors have resulted in life-threatening bleeding into the abdominal cavity. The physician should consider the possibility of a liver tumor in the differential diagnosis of disease in a woman taking NovaRing® if symptoms include acute upper abdominal pain, liver enlargement or signs of intra-abdominal bleeding.
Other conditions:
Contraindications
Contraindications
NovaRing® is contraindicated for any of the following conditions. If any of these conditions occur while using NovaRing® , the drug should be stopped immediately.
Side effects
Side effects
Side effects may occur with varying frequency when using the drug:
Infectious and parasitic diseases:often â¥1/100 – vaginal infection; infrequent < 1/100, â¥1/1,000 – cervicitis, cystitis, urinary tract infections.
Immune system disorders:postmarketing data1 – hypersensitivity.
Disorders of metabolism and nutrition: infrequent <1/100, â¥1/1,000 – increase in appetite.
Mental disorders:often ⥠1/100 – depression, decreased libido; infrequent < 1/100, â¥1/1,000 – change in mood.
Nervous system disorders:often ⥠1/100 – headache, migraine; infrequent < 1/100, ⥠1/1,000 – dizziness, hypoesthesia.
Visual disorders: infrequent < 1/100, ⥠1/1 000 – visual disturbance.
Vascular disorders: infrequent < 1/100, ⥠1/1,000 – “Tides”; rare < 1/1,000, ⥠1/10,000 – venous thromboembolism3.
Gastrointestinal Disorders:often ⥠1/100 – abdominal pain, nausea; infrequent < 1/100, ⥠1/1,000 – abdominal bloating, diarrhea, vomiting, constipation.
Skin and subcutaneous tissue disorders:often ⥠1/100 – acne; infrequent < 1/100, ⥠1/1,000 – alopecia, eczema, skin itching, rash; postmarketing data1 – urticaria.
Muscular and connective tissue disorders: frequently < 1/100, ⥠1/1,000 – back pain, muscle cramps, pain in the extremities.
Recreational and urinary tract disorders: infrequent < 1/100, ⥠1/1 000 – dysuria, imperative urge to urinate, pollakiuria.
Hdisorders of the genitals and the mammary gland: often ⥠1/100 – breast engorgement and tenderness, genital itching in women, painful menstrual-like bleeding, pelvic pain, vaginal discharge; infrequent < 1/100, ⥠1/1,000 – absence of menstrual-like bleeding, discomfort in the breasts, breast enlargement, breast thickening, cervical polyps, contact (during intercourse) bloody discharge (bleeding), painful sensations during intercourse, cervical ectropion, Cystic fibrosis, heavy menstrual bleeding, acyclic bleeding, pelvic discomfort, premenstrual syndrome, burning sensation in the vagina, vaginal odor, vaginal pain, discomfort and dryness of the vulva and vaginal mucosa; postmarketing use data1 – local reactions in the partner2.
General disorders and disorders at the site of administration: frequently ⥠1/100 – discomfort when applying the vaginal ring, vaginal ring prolapse; infrequent < 1/100, ⥠1/1,000 – fatigue, irritability, malaise, swelling, foreign body sensation, difficulty applying contraceptive, ring rupture (damage).
Influence on laboratory and instrumental findings:often ⥠1/100 – increase in body weight; infrequent < 1/100, ⥠1/1,000 – increase in blood pressure.
1 – The list of side effects is based on data from spontaneous reports. It is not possible to accurately determine the frequency.
2 – “local reactions in the partner” include reports of “local reactions on the penile side” (e.g., pain, hyperemia, bruising and abrasions).
3 – Observational cohort study data: â¥1/10,000 to < 1/1,000 female years.
Overdose
Overdose
Serious consequences of an overdose of hormonal contraceptives have not been described.
Symptoms:possible symptoms include nausea, vomiting, and slight bleeding from the vagina in young girls.
Treatment: There are no antidotes. Treatment is symptomatic.
Pregnancy use
Pregnancy use
NovaRing® is designed to prevent pregnancy. If a woman wants to stop using the drug to get pregnant, it is recommended to wait until the natural cycle is restored to conceive, as this will help correctly calculate the date of conception and delivery.
Pregnancy
The use of NovaRing® during pregnancy is contraindicated. If pregnancy occurs, the ring should be removed. Extensive epidemiologic studies have found no increased risk of birth defects in children born to women who took OCs before pregnancy and no teratogenic effects when women took OCs early in pregnancy without knowing about it. Although this is true for all OCs, it is not known whether this is also true for NovaRing®. A clinical study in a small group of women showed that despite the fact that NovaRing® is injected into the vagina, the concentrations of contraceptive sex hormones inside the uterus with NovaRing® are similar to those with OCs. No pregnancy outcomes have been described in women who used NovaRing® in a clinical trial.
Breastfeeding
The use of NovaRing® during breastfeeding is not indicated. The composition of the drug may affect lactation, reduce the amount and change the composition of breast milk. Small amounts of contraceptive sex hormones and/or their metabolites may be excreted with milk, but no evidence of adverse effects on child health has been obtained.
Children
The safety and effectiveness of NovaRing® for adolescent girls under the age of 18 years has not been studied.
Additional information
| Shelf life | 40 months. It is allowed to store the drug at the temperature not more than 30 °С for not more than 4 months from the date of changing the storage conditions, but not later than the expiration date. If the storage conditions are changed, the new expiration date should be indicated on the package in the line "At a temperature not exceeding 30 ° C store to: ". Do not use the drug after the expiration date indicated on the package. |
|---|---|
| Conditions of storage | At a temperature of 2-8 °C. |
| Manufacturer | N.W. Organon, The Netherlands |
| Medication form | vaginal rings |
| Brand | N.W. Organon |
Related products
Gynecology and Obstetrics
Prepidil, intracervical gel 0.5 mg/3 g syringes with catheter
Gynecology and Obstetrics
Buy NovaRing, vaginal rings 0.015 mg+0.120 mg/day 3 pcs with delivery to USA, UK, Europe and over 120 other countries.