No products in the cart.
NovaRing, vaginal rings 0.015 mg+0.120 mg/day
€46.06 €39.92
Out of stock
(E-mail when Stock is available)
EAN: 4601909000052
SKU: 206791
Categories: Contraceptive, Gynecology and Obstetrics, Hormonal, Medicine
Description
Pharmacodynamics
NovaRing® is a hormonal combined contraceptive containing etonogestrel and ethinylestradiol. Etonogestrel is a progestagen (a derivative of 19-nortestosterone) that binds with high affinity to progesterone receptors in target organs. Ethinyl estradiol is an estrogen and is widely used to produce contraceptives.
The contraceptive effect of NovaRing® is due to a combination of different factors, the most important of which is suppression of ovulation.
Effectiveness
In clinical studies, the Perl index (a measure of the frequency of pregnancy in 100 women over 1 year of contraception) for NovaRing® was found to be 0.96 (95% CI: 0.64-1.39) and 0.64 (95% CI: 0.35-1.07) in statistical analyses of all randomized participants (ITT analyses) and analyses of study participants who completed them according to protocol (PP analyses), respectively. These values were similar to the Perl index values obtained in comparative studies of combined oral contraceptives (OCs) containing levonorgestrel/ethinylestradiol (0.150/0.030 mg) or drospirenone/ethinylestradiol (3/0.30 mg).
The use of NovaRing® makes the cycle more regular, reduces the pain and intensity of menstrual bleeding, which helps to reduce the incidence of iron deficiency. There is data on reduction of risk of endometrial and ovarian cancer during use of the drug.
The nature of bleeding
. A one-year comparison of bleeding patterns in 1000 women using NovaRing® and OCs containing levonorgestrel/ethinylestradiol (0.150/0.030 mg) showed significantly less breakthrough bleeding or smear-like bleeding with NovaRing® compared to OCs. In addition, the incidence of bleeding occurring only during a break in use was significantly higher among women using NovaRing®.
Effects on bone mineral density
A comparative two-year study of the effects of NovaRing® (n=76) and the non-hormonal IUD (n=31) found no effect on bone mineral density in women.
Children
The safety and effectiveness of NovaRing® for adolescent girls under 18 years of age has not been studied.
Pharmacokinetics
Etonogestrel
absorption
The etonogestrel released from the NovaRing® vaginal ring is rapidly absorbed through the vaginal mucosa. The maximum plasma concentration of etonogestrel, about 1700 pg/ml, is reached about 1 week after the insertion of the ring. Plasma concentrations vary over a small range and slowly decrease to about 1600 pg/mL after 1 week, 1500 pg/mL after 2 weeks, and 1400 pg/mL after 3 weeks of use. Absolute bioavailability is about 100%, which exceeds bioavailability with oral administration of etonogestrel. According to the results of measurements of cervical and intrauterine concentrations of etonogestrel in women using NovaRing® and women using oral contraceptives containing 0.150 mg of desogestrel and 0.020 mg of ethinylestradiol, the observed values of etonogestrel concentrations were comparable.
Distribution
Atonogestrel binds to plasma albumin and sex hormone binding globulin (hGHB). The apparent volume of distribution of etonogestrel is 2.3 L/kg.
Metabolism
Biotransformation of etonogestrel occurs by the known pathways of sex hormone metabolism. The apparent blood plasma clearance is about 3.5 L/h. No direct interaction with ethinylestradiol taken simultaneously has been revealed.
Evacuation
The plasma concentrations of etonogestrel decrease in two phases. In the terminal phase, the elimination half-life is approximately 29 h. Etonogestrel and its metabolites are excreted by the kidneys and through the intestine with the bile at a ratio of about 1.7:1. The elimination half-life of metabolites is about 6 days.
Ethinylestradiol
absorption
Ethinylestradiol released from the NovaRing® vaginal ring is rapidly absorbed through the vaginal mucosa. The maximum plasma concentration of approximately 35 pg/ml is reached 3 days after ring insertion and decreases to 19 pg/ml after 1 week, to 18 pg/ml after 2 weeks and 18 pg/ml after 3 weeks of use. Absolute bioavailability is approximately 56% and is comparable to that of oral ethinylestradiol. According to the results of measurements of cervical and intrauterine ethinylestradiol concentrations in women using NovaRing® and women using oral contraceptives containing 0.150 mg of desogestrel and 0.020 mg of ethinylestradiol, the observed values of ethinylestradiol concentrations were comparable.
Ethinylestradiol concentrations were studied in a comparative randomized trial of NovaRing® (vaginal daily release of ethinylestradiol 0.015 mg), a transdermal patch (norelgestromin/ethinylestradiol; daily ethinylestradiol release 0.020 mg) and OCs (levonorgestrel/ethinylestradiol; daily ethinylestradiol release 0.030 mg) during one cycle in healthy women. Systemic exposure to ethinylestradiol over one month (AUC 0-∞) for NovaRing® was statistically significantly lower than for the patch and OC, at 10.9, 37.4, and 22.5 ng/h/mL, respectively.
Distribution
Ethinylestradiol binds nonspecifically to plasma albumin. The apparent volume of distribution is about 15 l/kg.
Metabolism
Ethinylestradiol is metabolized by aromatic hydroxylation. Its biotransformation produces a large number of hydroxylated and methylated metabolites. They circulate in free form or as sulfate and glucuronide conjugates. The apparent clearance is approximately 35 l/h.
Elimation
The plasma concentrations of ethinylestradiol decrease in two phases. The terminal phase elimination half-life varies widely; the median is about 34 h. Ethinylestradiol is not excreted unchanged. Metabolites of ethinylestradiol are excreted by the kidneys and through the intestine with the bile at a ratio of 1.3:1. The elimination half-life of metabolites is about 1.5 days.
Special patient groups
Children
The pharmacokinetics of NovaRing® in healthy adolescent girls under 18 years of age who have already menstruated have not been studied.
Renal dysfunction
The effect of renal disease on the pharmacokinetics of NovaRing® has not been studied.
Hepatic dysfunction
The effect of liver disease on the pharmacokinetics of NovaRing® has not been studied. However, patients with liver dysfunction may have impaired sex hormone metabolism.
Ethnic groups
The pharmacokinetics of the drug in ethnic groups have not been specifically studied.
Indications
Indications
Contraception.
Pharmacological effect
Pharmacological effect
Pharmacodynamics
The drug NuvaRing® is a hormonal combined contraceptive containing etonogestrel and ethinyl estradiol. Etonogestrel is a progestogen (19-nortestosterone derivative) that binds with high affinity to progesterone receptors in target organs. Ethinyl estradiol is an estrogen and is widely used in the production of contraceptives.
The contraceptive effect of NovaRing® is due to a combination of various factors, the most important of which is the suppression of ovulation.
Efficiency
In clinical studies, it was found that the Pearl index (an indicator reflecting the incidence of pregnancy in 100 women during 1 year of contraception) in women aged 18 to 40 years for the drug NuvaRing® was 0.96 (95% CI: 0.64-1.39) and 0.64 (95% CI: 0.35-1.07) in a statistical analysis of all randomized participants (ITT analysis) and analysis of study participants who completed them according to the protocol (PP analysis), respectively. These values were similar to the Pearl index values obtained in comparative studies of combined oral contraceptives (COCs) containing levonorgestrel/ethinyl estradiol (0.150/0.030 mg) or drospirenone/ethinyl estradiol (3/0.30 mg).
With the use of the drug NuvaRing®, the cycle becomes more regular, the pain and intensity of menstrual-like bleeding decreases, which helps reduce the incidence of iron deficiency conditions. There is evidence of a reduction in the risk of endometrial and ovarian cancer with the use of the drug.
Nature of bleeding
A comparison of bleeding patterns over one year in 1000 women using the drug NuvaRing® and COCs containing levonorgestrel / ethinyl estradiol (0.150/0.030 mg) showed a significant reduction in the frequency of breakthrough bleeding or spotting when using the drug NovaRing® compared with COCs. In addition, the frequency of cases where bleeding occurred only during a break in the use of the drug was significantly higher among women using the drug NuvaRing®.
Effect on bone mineral density
A comparative two-year study of the effect of the drug NovaRing® (n=76) and a non-hormonal intrauterine device (n=31) did not reveal any effect on bone mineral density in women.
Children
The safety and effectiveness of NuvaRing® in adolescent girls under 18 years of age has not been studied.
Pharmacokinetics
Etonogestrel
Suction
Etonogestrel, released from the NuvaRing® vaginal ring, is rapidly absorbed through the vaginal mucosa. The maximum concentration of etonogestrel in blood plasma, approximately 1700 pg/ml, is achieved approximately 1 week after insertion of the ring. Plasma concentrations vary within a small range and decrease slowly to approximately 1600 pg/ml after 1 week, 1500 pg/ml after 2 weeks and 1400 pg/ml after 3 weeks of use. Absolute bioavailability is about 100%, which exceeds the bioavailability of etonogestrel when taken orally. Based on the results of measurements of etonogestrel concentrations in the cervix and inside the uterus in women using the drug NuvaRing® and women using oral contraceptives containing 0.150 mg of desogestrel and 0.020 mg of ethinyl estradiol, the observed values of etonogestrel concentrations were comparable.
Distribution
Etonogestrel binds to plasma albumin and sex hormone binding globulin (SHBG). The apparent volume of distribution of etonogestrel is 2.3 L/kg.
Metabolism
Biotransformation of etonogestrel occurs through known pathways of sex hormone metabolism. The apparent clearance of blood plasma is about 3.5 l/h. No direct interaction with ethinyl estradiol taken concomitantly has been identified.
Removal
Plasma concentrations of etonogestrel decrease in two phases. In the terminal phase, the half-life is approximately 29 hours. Etonogestrel and its metabolites are excreted by the kidneys and through the intestines with bile in a ratio of about 1.7:1. The half-life of metabolites is approximately 6 days.
Ethinyl estradiol
Suction
Ethinyl estradiol, released from the NuvaRing® vaginal ring, is rapidly absorbed through the vaginal mucosa. The maximum plasma concentration of about 35 pg/ml is achieved 3 days after administration of the ring and decreases to 19 pg/ml after 1 week, to 18 pg/ml after 2 weeks and 18 pg/ml after 3 weeks of use. Absolute bioavailability is approximately 56% and is comparable to that of oral ethinyl estradiol. Based on the results of measurements of ethinyl estradiol concentrations in the cervix and inside the uterus in women using the drug NuvaRing® and women using oral contraceptives containing 0.150 mg of desogestrel and 0.020 mg of ethinyl estradiol, the observed values of ethinyl estradiol concentrations were comparable.
Ethinyl estradiol concentrations were studied in a comparative randomized study of NovaRing® (daily vaginal release of ethinyl estradiol 0.015 mg), transdermal patch (norelgestromin / ethinyl estradiol; daily release of ethinyl estradiol 0.020 mg) and COC (levonorgestrel / ethinyl estradiol; daily release ethinyl estradiol 0.030 mg) during one cycle in healthy women. Systemic exposure to ethinyl estradiol over a month (AUC 0-∞) for NovaRing® was statistically significantly lower than for the patch and COCs, and amounted to 10.9, 37.4 and 22.5 ng h/ml, respectively.
Distribution
Ethinyl estradiol binds nonspecifically to plasma albumin. The apparent volume of distribution is approximately 15 l/kg.
Metabolism
Ethinyl estradiol is metabolized by aromatic hydroxylation. During its biotransformation, a large number of hydroxylated and methylated metabolites are formed. They circulate freely or as sulfate and glucuronide conjugates. The apparent clearance is approximately 35 l/h.
Removal
Plasma ethinyl estradiol concentrations decrease in two phases. The half-life in the terminal phase varies widely; the median is about 34 hours. Ethinyl estradiol is not excreted unchanged. Ethinyl estradiol metabolites are excreted by the kidneys and through the intestines with bile in a ratio of 1.3:1. The half-life of metabolites is about 1.5 days.
Special patient groups
Children
The pharmacokinetics of NovaRing® in healthy adolescent girls under 18 years of age who have already menstruated have not been studied.
Renal dysfunction
The effect of kidney disease on the pharmacokinetics of NovaRing® has not been studied.
Liver dysfunction
The effect of liver diseases on the pharmacokinetics of NovaRing® has not been studied. However, in patients with impaired liver function, the metabolism of sex hormones may deteriorate.
Ethnic groups
The pharmacokinetics of the drug in representatives of ethnic groups has not been specifically studied.
Special instructions
Special instructions
If any of the diseases, conditions or risk factors listed below are present, the benefits of using the drug NuvaRing® and the possible risks for each individual woman should be assessed before she starts using the drug NuvaRing®. In case of exacerbation of diseases, deterioration of the condition, or the first occurrence of any of the conditions listed below, a woman should consult a doctor to decide on the possibility of further use of the drug NuvaRing®.
Circulatory disorders
The use of hormonal contraceptives may be associated with the development of venous thrombosis (deep vein thrombosis and pulmonary embolism) and arterial thrombosis, as well as associated complications, sometimes fatal.
The use of any COC increases the risk of developing venous thromboembolism (VTE) compared to the risk of VTE in patients not using COCs. The greatest risk of developing VTE is observed in the first year of COC use.
Data from a large prospective cohort study of the safety of various COCs suggest that the greatest increase in risk, compared with the risk in women not using COCs, is observed in the first 6 months after starting COC use or resuming their use after a break (4 weeks or more). In nonpregnant women not using oral contraceptives, the risk of developing VTE is 1 to 5 per 10,000 woman-years (WY).
In women using oral contraceptives, the risk of developing VTE ranges from 3 to 9 cases per 10,000 women. The increase in risk occurs to a lesser extent than in pregnancy, where the risk is 5-20 per 10,000 YL (pregnancy data are based on the actual duration of pregnancy in standard studies; based on the assumption that pregnancy lasts 9 months, the risk is 7 to 27 per 10,000 YL). In postpartum women, the risk of developing VTE ranges from 40 to 65 cases per 10,000 women. VTE is fatal in 1-2% of cases.
According to research results, the increased risk of developing VTE in women using the drug NuvaRing® is similar to that in women using COCs (for adjusted risk ratio, see the table below). A large prospective observational study, TASC (Transatlantic Active Study of the Cardiovascular Safety of NuvaRing®), assessed the risk of developing VTE in women who started using NuvaRing® or COCs, switched to NovaRing® or COCs from other contraceptives, or resumed use of NovaRing® or COCs in a population of typical users.
The women were followed for 24-48 months. The results showed a similar level of risk of developing VTE in women using the drug NuvaRing® (frequency 8.3 cases per 10,000 YL) and in women using COCs (frequency 9.2 cases per 10,000 YL). For women using COCs other than those containing desogestrel, gestodene and drospirenone, the incidence of VTE was 8.5 cases per 10,000 women.
A retrospective cohort study initiated by the FDA (United States Food and Drug Administration) showed that the incidence of VTE in women who started using the drug NuvaRing® was 11.4 cases per 10,000 YL, while in women who started using COCs containing levonorgestrel, the incidence of VTE was 9.2 cases per 10,000 YL.
Assessment of the risk (risk ratio) of developing VTE in women using the drug NuvaRing®, compared with the risk of developing VTE in women using COCs
Epidemiological study, population:
TASC (Dinger, 2012) Women who started using the drug (including again after a break) and switched from other contraceptives.
“FDA Initiated Study” (Sydney, 2011) Women who started using combined hormonal contraceptives (CHCs) for the first time during the study period.
Comparator drug(s):
All available COCs during the study1. RR2: 0.8 (0.5-1.5) Available COCs, except those containing desogestrel, gestodene, drospirenone.
COCs available during the study period3.
Risk ratio (RR) (95% CI):
OR2: 0.8 (0.5-1.5); RR2: 0.9 (0.4-2.0).
RR4: 1.09 (0.55-2.16); RR4: 0.96 (0.47-1.95).
1 – Including low-dose COCs containing the following progestins: chlormadinone acetate, cyproterone acetate, desogestrel, dienogest, drospirenone, ethynodiol diacetate, gestodene, levonorgestrel, norethindrone, norgestimate or norgestrel.
2 – Taking into account age, BMI, duration of use, history of VTE.
3 – Including low-dose COCs containing the following progestins: norgestimate, norethindrone or levonorgestrel.
4 – Taking into account age, place and year of inclusion in the study.
There are extremely rare cases of thrombosis of other blood vessels (for example, arteries and veins of the liver, mesenteric vessels, kidneys, brain and retina) with the use of COCs. It is unknown whether these cases are related to the use of COCs.
Possible symptoms of venous or arterial thrombosis may be unilateral swelling and/or pain in the lower extremity, local increase in temperature in the lower extremity, hyperemia or discoloration of the skin on the lower extremity; sudden severe chest pain, possibly radiating to the left arm; attack of shortness of breath, cough; any unusual, severe, prolonged headaches; sudden partial or complete loss of vision; double vision; slurred speech or aphasia; dizziness; collapse, accompanied or not accompanied by a focal epileptic seizure; sudden weakness or severe numbness on one side of the body or any part of the body; movement disorders; “acute” stomach.
Risk factors for the development of venous thrombosis and embolism:
Age;
Presence of diseases in the family history (venous thrombosis and embolism in brothers/sisters at any age or in parents at a young age). If a hereditary predisposition is suspected, before starting any hormonal contraceptives, the woman should be referred to a specialist for consultation;
Prolonged immobilization, major surgery, any surgery on the lower extremities, or serious trauma. In such situations, it is recommended to stop using the drug (in the case of a planned operation, at least 4 weeks in advance) with subsequent resumption of use no earlier than 2 weeks after complete restoration of motor activity;
Obesity (body mass index more than 30 kg/m2);
Possibly thrombophlebitis of the superficial veins with varicose veins.
There is no consensus on the possible role of these conditions in the etiology of venous thrombosis.
Risk factors for the development of complications of arterial thromboembolism:
Age;
Smoking (with heavy smoking and with age, the risk increases even more significantly, especially in women over 35 years of age);
Dyslipoproteinemia;
Obesity (body mass index more than 30 kg/m2);
Increased blood pressure;
Migraine;
Heart valve disease;
Atrial fibrillation;
Presence of diseases in the family history (arterial thrombosis in brothers/sisters at any age or in parents at a relatively early age). If a hereditary predisposition is suspected, the woman should be referred to a specialist for consultation before starting any hormonal contraceptives. Biochemical factors that may indicate hereditary or acquired predisposition to venous or arterial thrombosis include activated protein C resistance, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
Other conditions that can cause unwanted circulatory problems include diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome and chronic inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), as well as sickle cell anemia.
It is necessary to take into account the increased risk of thromboembolism in the postpartum period. An increase in the frequency or severity of migraine (which may be a prodromal symptom of cerebrovascular accidents) while using hormonal contraceptives may be a reason to immediately discontinue use of hormonal contraceptives.
Women using CHCs should be advised to consult a doctor if possible symptoms of thrombosis occur. If thrombosis is suspected or confirmed, CHC use should be discontinued. In this case, it is necessary to use effective contraception, since anticoagulants (coumarins) have a teratogenic effect.
Risk of developing tumors
The most important risk factor for developing cervical cancer is infection with the human papillomavirus (HPV). Epidemiological studies have shown that long-term use of COCs further increases this risk, but it is unclear how much of this is due to other factors, such as increased frequency of cervical smears and differences in sexual behavior, including the use of barrier contraceptives. It remains unclear how this effect is related to the use of the drug NuvaRing®.
A meta-analysis of 54 epidemiological studies found a small increase (1.24) in the relative risk of breast cancer in women taking combined hormonal oral contraceptives. The risk gradually decreases over 10 years after stopping the drugs. Breast cancer rarely develops in women under 40 years of age, so the additional incidence of breast cancer in women who take or have taken COCs is small compared to the overall risk of developing breast cancer. Breast cancer diagnosed in women who use COCs is clinically less severe than cancer diagnosed in women who have never used COCs. The increased risk of breast cancer may be due to the earlier diagnosis of breast cancer in women taking COCs, the biological effects of COCs, or a combination of both.
In rare cases, cases of development of benign, and even more rarely, malignant liver tumors have been observed in women taking COCs. In some cases, these tumors led to the development of life-threatening bleeding into the abdominal cavity. The doctor should consider the possibility of a liver tumor in the differential diagnosis of diseases in a woman taking NuvaRing® if symptoms include acute pain in the upper abdomen, liver enlargement, or signs of intra-abdominal bleeding.
Other states
Women with hypertriglyceridemia or a corresponding family history have an increased risk of developing pancreatitis when taking hormonal contraceptives.
Many women taking hormonal contraceptives experience a slight increase in blood pressure, but clinically significant increases in blood pressure are rare. A direct connection between the use of hormonal contraceptives and the development of arterial hypertension has not been established. If, when using the drug NuvaRing®, there is a constant increase in blood pressure, you should contact your doctor to decide whether it is necessary to remove the vaginal ring and prescribe antihypertensive therapy. With adequate control of blood pressure using antihypertensive drugs, it is possible to resume use of the drug NuvaRing®.
During pregnancy and during the use of combined oral contraceptives, the development or worsening of the following conditions has been noted, although their relationship with the use of contraceptives has not been definitively established: jaundice and/or itching caused by cholestasis, formation of gallstones, porphyria, systemic lupus erythematosus, hemolytic-uremic syndrome, Sydenham’s chorea (minor chorea), herpes of pregnancy, hearing loss due to otosclerosis, (hereditary) angioedema.
Acute or chronic liver diseases may serve as a reason to discontinue the drug NuvaRing® until liver function indicators normalize. Recurrence of cholestatic jaundice, previously observed during pregnancy or during the use of sex hormones, requires discontinuation of the drug NuvaRing®.
Although estrogens and progestogens may influence peripheral insulin resistance and tissue glucose tolerance, there is no evidence to support the need to change hypoglycemic therapy during the use of hormonal contraceptives. However, women with diabetes should be under constant medical supervision when using NuvaRing®, especially in the first months of contraception.
There is evidence of a worsening of Crohn’s disease and ulcerative colitis with the use of hormonal contraceptives.
In rare cases, pigmentation of the facial skin (chloasma) may occur, especially if it occurred earlier during pregnancy. Women predisposed to the development of chloasma should avoid exposure to sunlight and ultraviolet radiation while using NovaRing®.
The following conditions may prevent the ring from being inserted correctly or may cause it to fall out: cervical prolapse, bladder and/or rectal hernia, severe chronic constipation.
In very rare cases, women have unintentionally inserted the NuvaRing® vaginal ring into the urethra and possibly into the bladder. When symptoms of cystitis appear, it is necessary to consider the possibility of incorrect insertion of the ring.
Cases of vaginitis have been described during use of the drug NuvaRing®. There is no evidence that treatment of vaginitis affects the effectiveness of the use of the drug NuvaRing®, as well as evidence of the effect of the use of the drug NovaRing® on the effectiveness of treatment of vaginitis.
Very rare cases of difficult ring removal have been described that required removal by a medical professional.
Medical examination/consultation
Before prescribing the drug NuvaRing® or resuming its use, you should carefully review the woman’s medical history (including family history) and conduct a gynecological examination to exclude pregnancy. It is necessary to measure blood pressure, conduct an examination of the mammary glands, pelvic organs, including a cytological examination of cervical smears and some laboratory tests, to exclude contraindications and reduce the risk of possible side effects of the drug. The frequency and nature of medical examinations depend on the individual characteristics of each patient, but medical examinations are carried out at least once every 6 months. A woman should read the instructions for use and follow all recommendations. The woman should be informed that NuvaRing® does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Reduced efficiency
The effectiveness of NovaRing® may decrease if the regimen is not followed or if concomitant therapy is carried out.
Reduced cycle control
During use of the drug NovaRing®, acyclic bleeding (spotting or sudden bleeding) may occur. If such bleeding is observed after regular cycles with the correct use of the drug NuvaRing®, you should contact your gynecologist to conduct the necessary diagnostic studies, including to exclude organic pathology or pregnancy. A diagnostic curettage may be required.
Some women do not bleed after the ring is removed. If the drug NuvaRing® was used according to the instructions, it is unlikely that the woman is pregnant. If the recommendations of the instructions are not followed and there is no bleeding after removing the ring, as well as if there is no bleeding for two cycles in a row, pregnancy must be excluded.
Effects of ethinyl estradiol and etonogestrel on a sexual partner
The possible pharmacological effects and extent of exposure of ethinyl estradiol and etonogestrel to male sexual partners (due to absorption through penile tissue) have not been studied.
Ring damage
In rare cases, when using the drug NuvaRing®, ring rupture was observed. The core of the drug NuvaRing® is solid, so its contents remain intact, and the release of hormones does not change significantly. If the ring ruptures, it usually falls out of the vagina (see the recommendations in the subsection “What to do if the ring has been temporarily removed from the vagina” in the “Dosage and Administration” section). If the ring ruptures, a new ring must be inserted.
Ring falling out
Sometimes the NuvaRing® vaginal ring may fall out of the vagina, for example, if it is inserted incorrectly, when a tampon is removed, during sexual intercourse, or due to severe or chronic constipation. In this regard, it is advisable for a woman to regularly check the presence of the NuvaRing® vaginal ring in the vagina. If the NuvaRing® vaginal ring falls out of the vagina, you must follow the recommendations of the subsection “What to do if the ring has been temporarily removed from the vagina” in the “Method of administration and dosage” section.
Impact on the ability to drive vehicles and other mechanisms that require increased concentration
Based on information about the pharmacodynamic properties of the drug NovaRing®, it can be expected that it does not affect the ability to drive vehicles and operate machinery.
Active ingredient
Active ingredient
Ethinyl estradiol, Etonogestrel
Composition
Composition
Active ingredients:
Etonogestrel – 11.7 mg;
Ethinyl estradiol – 2.7 mg.
Excipients:
Ethylene and vinyl acetate copolymer (28% vinyl acetate) – 1677 mg;
Ethylene and vinyl acetate copolymer (9% vinyl acetate) – 197 mg;
Magnesium stearate – 1.7 mg.
Pregnancy
Pregnancy
The drug NuvaRing® is intended to prevent pregnancy. If a woman wants to stop using the drug in order to become pregnant, it is recommended to wait for the restoration of the natural cycle to conceive, as this will help to correctly calculate the date of conception and birth.
Pregnancy
The use of NovaRing® during pregnancy is contraindicated. If pregnancy occurs, the ring should be removed. Extensive epidemiological studies have not revealed an increased risk of congenital malformations in children born to women who took COCs before pregnancy, as well as teratogenic effects in cases where women took COCs in early pregnancy without knowing about it. Although this applies to all COCs, it is not known whether this also applies to NuvaRing®. A clinical study in a small group of women showed that, despite the fact that the drug NuvaRing® is administered into the vagina, the concentrations of contraceptive sex hormones inside the uterus when using the drug NuvaRing® are similar to those when using COCs. Pregnancy outcomes in women who used NuvaRing® during a clinical trial have not been described.
Breastfeeding period
The use of NuvaRing® during breastfeeding is not indicated. The composition of the drug can affect lactation, reduce the amount and change the composition of breast milk. Small amounts of contraceptive sex hormones and/or their metabolites may be excreted in milk, but there is no evidence of their negative impact on the health of children.
Children
The safety and effectiveness of NuvaRing® in adolescent girls under 18 years of age have not been studied.
Contraindications
Contraindications
The drug NuvaRing® is contraindicated in the presence of any of the conditions listed below. If any of these conditions occur during the use of the drug NuvaRing®, you should immediately stop using the drug.
Thrombosis (arterial or venous) and thromboembolism currently or in history (including deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular disorders);
Conditions preceding thrombosis (including transient ischemic attacks, angina) currently or in history;
Predisposition to the development of venous or arterial thrombosis, including hereditary diseases: resistance to activated protein C, antithrombin III deficiency, protein C deficiency, protein S deficiency, hyperhomocysteinemia and antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant);
Migraine with focal neurological symptoms currently or in history;
Diabetes mellitus with vascular damage;
Severe or multiple risk factors for venous or arterial thrombosis: hereditary predisposition to thrombosis (thrombosis, myocardial infarction or cerebrovascular accident at a young age in one of the immediate family), hypertension, lesions of the valvular apparatus of the heart, atrial fibrillation, extended surgery, prolonged immobilization, major trauma, obesity (body weight >30 kg/m2), smoking in women over 35 years of age (see section “Special instructions”);
Pancreatitis with severe hypertriglyceridemia, current or history.
Severe liver diseases;
Liver tumors (malignant or benign), including a history of;
Known or suspected hormone-dependent malignant tumors (for example, genital or breast);
Bleeding from the vagina of unknown etiology;
Pregnancy, including intended;
Hypersensitivity to any of the active or excipients of the drug NuvaRing®.
With caution: if you have any of the following diseases, conditions or risk factors, you should evaluate the benefits of using the drug NuvaRing® and the possible risks for each individual woman before she starts using the drug NuvaRing®. In case of exacerbation of diseases, deterioration of the condition, or the first occurrence of any of the conditions listed below, a woman should consult a doctor to decide on the possibility of further use of the drug NuvaRing®.
The drug NuvaRing® should be used with caution in the following cases: risk factors for the development of thrombosis and thromboembolism: hereditary predisposition to thrombosis (thrombosis, myocardial infarction or cerebrovascular accident at a young age in one of the immediate family), smoking, obesity, dyslipoproteinemia, arterial hypertension, migraine without focal neurological symptoms, heart valve disease, heart rhythm disturbances, long-term immobilization, serious surgical interventions; thrombophlebitis of superficial veins; dyslipoproteinemia; heart valve disease; adequately controlled arterial hypertension; diabetes mellitus without vascular complications; acute or chronic liver diseases; jaundice and/or itching caused by cholestasis; cholelithiasis; porphyria; systemic lupus erythematosus; hemolytic-uremic syndrome; Sydenham’s chorea (minor chorea); hearing loss due to otosclerosis; (hereditary) angioedema; chronic inflammatory bowel diseases (Crohn’s disease and ulcerative colitis); sickle cell anemia; chloasma; Conditions that may make it difficult to use a vaginal ring: cervical prolapse, bladder hernia, rectal hernia, severe chronic constipation.
Side Effects
Side Effects
When using the drug, side effects may occur, occurring with varying frequencies:
often (≥ 1/100);
uncommon (< 1/100, ≥ 1/1,000);
rare (< 1/1,000, ≥ 1/10,000).
Infectious and parasitic diseases: often ≥1/100 – vaginal infection; uncommon <1/100, ≥1/1,000 - cervicitis, cystitis, urinary tract infections.
Immune system disorders: post-marketing data1 – hypersensitivity.
Metabolic and nutritional disorders: uncommon <1/100, ≥1/1,000 - increased appetite.
Mental disorders: often ≥ 1/100 – depression, decreased libido; uncommon <1/100, ≥1/1,000 - mood changes.
Nervous system disorders: often ≥ 1/100 – headache, migraine; infrequently <1/100, ≥1/1,000 - dizziness, hypoesthesia.
Visual impairment: uncommon < 1/100, ≥ 1/1,000 - visual impairment.
Vascular disorders: uncommon <1/100, ≥1/1,000 - “Hot flashes”; rarely <1/1,000, ≥1/10,000 - venous thromboembolism3.
Gastrointestinal disorders: often ≥ 1/100 – abdominal pain, nausea; uncommon <1/100, ≥1/1,000 - bloating, diarrhea, vomiting, constipation.
Disorders of the skin and subcutaneous tissues: often ≥ 1/100 – acne; uncommon <1/100, ≥1/1,000 - alopecia, eczema, itching, rash; post-marketing data1 - urticaria.
Musculoskeletal and connective tissue disorders: uncommon < 1/100, ≥ 1/1,000 - back pain, muscle spasms, pain in the extremities.
Renal and urinary tract disorders: uncommon <1/100, ≥1/1,000 - dysuria, urinary urgency, pollakiuria.
Disorders of the genital organs and mammary gland: often ≥ 1/100 – engorgement and tenderness of the mammary glands, genital itching in women, painful menstrual-like bleeding, pain in the pelvic area, vaginal discharge; uncommon < 1/100, ≥ 1/1,000 - absence of menstrual-like bleeding, discomfort in the mammary glands, enlarged mammary glands, lumps in the mammary glands, cervical polyps, contact (during sexual intercourse) spotting (bleeding), pain during intercourse, ectropion of the cervix, fibrocystic mastopathy, heavy menstrual-like bleeding, acyclic bleeding, discomfort in the pelvic area, premenstrual-like syndrome, burning sensation in the vagina, vaginal odor, pain in the vagina, discomfort and dryness of the vulva and vaginal mucosa; data from post-marketing use1 - local reactions in the partner2.
General disorders and disorders at the injection site: often ≥ 1/100 – discomfort when using the vaginal ring, loss of the vaginal ring; infrequently <1/100, ≥1/1,000 - fatigue, irritability, malaise, swelling, foreign body sensation, difficulty using a contraceptive, rupture (damage) of the ring.
Impact on the results of laboratory and instrumental studies: often ≥ 1/100 – increase in body weight; infrequently <1/100, ≥1/1,000 - increased blood pressure.
1 – the list of side effects is based on data obtained from spontaneous reports. It is not possible to accurately determine the frequency.
2 – “local partner reactions” includes reports of “local reactions on the penis” (eg pain, flushing, bruising and abrasions).
3 – data from an observational cohort study: ≥ 1/10,000 – < 1/1,000 women-years.
Interaction
Interaction
Interaction with other drugs
Interactions between hormonal contraceptives and other drugs may lead to the development of acyclic bleeding and/or contraceptive failure. The literature describes the following interactions with combined oral contraceptives in general.
Hepatic metabolism: Interactions may occur with drugs that induce liver microsomal enzymes, which may result in increased clearance of sex hormones. Interactions have been established, for example, with phenytoin, barbiturates, primidone, carbamazepine, rifampicin, and also possibly with oxcarbazepine, topiramate, felbamate, ritonavir, griseofulvin and preparations containing St. John’s wort (Hypericum perforatum).
When treating with any of the listed drugs, you should temporarily use a barrier method of contraception (condom) in combination with the use of the drug NuvaRing® or choose another method of contraception. During concomitant use of drugs that induce microsomal enzymes, and for 28 days after their discontinuation, barrier methods of contraception should be used.
If concomitant therapy is to be continued after 3 weeks of ring use, the next ring should be administered immediately without the usual interval.
Antibiotics: Decreased effectiveness of oral contraceptives containing ethinyl estradiol has been observed with concomitant use of antibiotics such as ampicillin and tetracyclines. The mechanism of this effect has not been studied. In a pharmacokinetic interaction study, oral administration of amoxicillin (875 mg, 2 times daily) or doxycycline (200 mg daily, then 100 mg daily) for 10 days while using NovaRing® had little effect on the pharmacokinetics of etonogestrel and ethinyl estradiol. When using antibiotics (excluding amoxicillin and doxycycline), you should use a barrier method of contraception (condom) during treatment and for 7 days after stopping antibiotics. If concomitant therapy is to be continued after 3 weeks of ring use, the next ring should be administered immediately without the usual interval. Pharmacokinetic studies have not revealed the effect of the simultaneous use of antifungal agents and spermicides on the contraceptive effectiveness and safety of the drug NovaRing®. When combined with suppositories and antifungal drugs, the risk of ring rupture slightly increases. Hormonal contraceptives may interfere with the metabolism of other drugs. Accordingly, their concentrations in plasma and tissues may increase (for example, cyclosporine) or decrease (for example, lamotrigine). To exclude possible interactions, you should read the instructions for use of other drugs.
Laboratory research
The use of contraceptive hormonal drugs may affect the results of certain laboratory tests, including biochemical indicators of liver, thyroid, adrenal and kidney function; on the plasma concentration of transport proteins, for example, corticosteroid binding globulin (CBG) and SHBG; for lipid/lipoprotein fractions; on indicators of carbohydrate metabolism; as well as on indicators of blood clotting and fibrinolysis. Indicators, as a rule, vary within normal values.
Combined use with tampons
Pharmacokinetic data show that the use of tampons does not affect the absorption of hormones released from the NuvaRing® vaginal ring. In rare cases, the ring may be accidentally removed when removing the tampon (see the subsection “What to do if the ring has been temporarily removed from the vagina” in the “Dosage and Administration” section).
Overdose
Overdose
Serious consequences of an overdose of hormonal contraceptives have not been described.
Symptoms: Possible symptoms include nausea, vomiting and light vaginal bleeding in young girls.
Treatment: There are no antidotes. Treatment is symptomatic.
Storage conditions
Storage conditions
At a temperature of 2–8 °C.
Shelf life
Shelf life
40 months.
One-time storage by the patient at a temperature not exceeding 30°C is allowed for no more than 4 months from the date of change in storage conditions, but no later than the expiration date. If the storage conditions change on the packaging, you must indicate the new expiration date in the line “Store at a temperature not exceeding 30 °C until: .”
Do not use the drug after the expiration date indicated on the package.
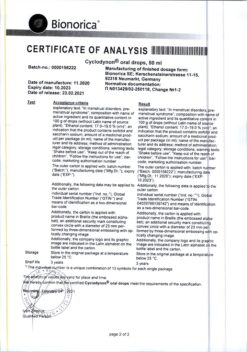
Manufacturer
Manufacturer
N.V.Organon, Netherlands
Additional information
| Shelf life | 40 months. A single storage by the patient at a temperature not higher than 30 ° C is allowed for not more than 4 months from the date of changing the storage conditions, but no later than the expiration date. If the storage conditions are changed, the new expiration date should be indicated on the package in the line "At the temperature not more than 30°С store to:". Do not use the drug after the expiration date specified on the package. |
|---|---|
| Conditions of storage | At a temperature of 2-8 °C. |
| Manufacturer | N.W. Organon, The Netherlands |
| Medication form | vaginal rings |
| Brand | N.W. Organon |
Related products
Buy NovaRing, vaginal rings 0.015 mg+0.120 mg/day with delivery to USA, UK, Europe and over 120 other countries.