No products in the cart.
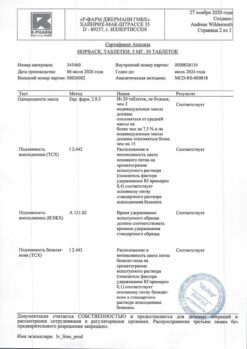
Norvasc, tablets 10 mg 30 pcs
€6.45 €5.73
Description
Norvasc – antihypertensive, antianginal.
Pharmacodynamics
Dihydropyridine derivative – BKK of III generation, has hypotensive and antianginal effect. It blocks slow calcium channels, reduces transmembrane transfer of calcium ions into the cell (more so into vascular smooth muscle cells than into cardiomyocytes).
The antianginal action is due to the dilation of coronary and peripheral arteries and arterioles:
In angina, it reduces the severity of myocardial ischemia; by dilating the peripheral arterioles, it reduces the RPS, reduces the afterload on the heart, and reduces myocardial oxygen demand;
– By dilating coronary arteries and arterioles in unchanged and ischemic areas of the myocardium, increases the flow of oxygen to the myocardium (especially in vasospastic angina); prevents coronary artery spasm (including that caused by smoking).Also caused by smoking).
In patients with stable angina a single daily dose increases exercise tolerance, slows the development of angina attacks and ischemic ST-segment depression, reduces the frequency of angina attacks and consumption of nitroglycerin and other nitrates.
It has a long-term dose-dependent hypotensive effect. The hypotensive effect is due to a direct vasodilating effect on the vascular smooth muscles. In case of arterial hypertension a single dose provides clinically significant BP reduction during 24 hours (in a patient lying and standing position).
Orthostatic hypotension with amlodipine is rare. Amlodipine does not cause decreased tolerance to physical load, left ventricular ejection fraction. It reduces the degree of left ventricular myocardial hypertrophy. It does not affect myocardial contractility and conduction, does not cause reflex increase in HR, inhibits platelet aggregation, increases glomerular filtration rate, has a weak natriuretic effect.
In diabetic nephropathy it does not increase the severity of microalbuminuria. It has no adverse effect on metabolism and plasma lipid concentration and may be used for therapy of patients with bronchial asthma, diabetes mellitus and gout. Significant decrease in BP is observed after 6-10 hours, the duration of effect is 24 hours.
. In patients with diseases of the cardiovascular system (including coronary atherosclerosis with lesion of one vessel and up to stenosis of 3 or more arteries, atherosclerosis of the carotid arteries), who had myocardial infarction, percutaneous transluminal coronary angioplasty (PTCA) or in patients with angina pectoris the use of amlodipine prevents the development of carotid intima-media thickening, reduces mortality from myocardial infarction, stroke, PTCA, aortocoronary bypass; leads to fewer hospitalizations for unstable angina and progression of CHF; reduces the frequency of interventions to restore coronary blood flow.
The therapy with digoxin, diuretics and ACE inhibitors does not increase risk of death or complications and lethal outcomes in patients with CHF (functional class III-IV according to NYHA classification) during therapy. In patients with CHF (functional class III-IV according to NYHA classification) of non-ischemic etiology during amlodipine use there is a possibility of pulmonary edema development.
Pharmacokinetics
After oral administration amlodipine is well absorbed from the gastrointestinal tract. Mean absolute bioavailability is 64-80%, Tmax in serum is 6-12 h. Css are reached after 7-8 days of therapy.
Eating does not affect absorption of amlodipine. The average Vd is 21 l/kg, indicating that most of the drug is in the tissues and less in the blood. Most of the drug in blood (97.5%) is bound to plasma proteins. Amlodipine undergoes slow but active metabolism in the liver with no significant first-pass effect. Metabolites have no significant pharmacological activity.
After a single dose, the T1/2 ranges from 35 to 50 h; when repeatedly administered, the T1/2 is approximately 45 h. About 60% of oral intake is excreted by kidneys mainly as metabolites, 10% – unchanged, and 20-25% – via intestine with bile. Total clearance of amlodipine is 0.116 ml/s/kg (7 ml/min/kg; 0.42 l/h/kg).
The use in elderly patients. In elderly patients (over 65 years) the excretion of amlodipine is slower (T1/2 – 65 h) compared to younger patients, but this difference has no clinical significance.
The use in patients with hepatic impairment. The prolongation of T1/2 in patients with hepatic impairment suggests that the drug cumulation in the body will be higher with long-term use (T1/2 – up to 60 h).
The use in patients with renal failure. Renal insufficiency has no significant effect on the kinetics of amlodipine.
Amlodipine penetrates through the HEB. It is not eliminated by hemodialysis.
Indications
Indications
Arterial hypertension (both in monotherapy and in combination with other hypotensive agents);
/p>
Stable angina and vasospastic angina (Prinzmetal’s angina or variant angina) both in monotherapy and in combination with other antianginal agents.
Active ingredient
Active ingredient
Composition
Composition
Active substance:
amlodipine 10 mg;
Associates:
MCC – 248.111 mg;
calcium hydrophosphate 126 mg;
sodium carboxymethyl starch – 8 mg;
magnesium stearate – 4 mg;
How to take, the dosage
How to take, the dosage
Overly, once daily with the required volume of water (100 ml).
In case of arterial hypertension and angina pectoris, the usual starting dose is 5 mg; depending on the individual reaction of the patient, it may be increased to a maximum dose of 10 mg.
The use in the elderly. It is recommended to use in usual doses, no change in the dose of the drug is required.
The use in patients with impaired liver function. Although the T1/2 of amlodipine, as of all BCCs, is increased in patients with this pathology, no dose adjustment is usually required (see “Special Precautions”).
The use in patients with impaired renal function. It is recommended to use Norvasc® in usual doses, however, a possible slight increase of T1/2 should be taken into account.
Dose adjustment is not required for concomitant use with thiazide diuretics, β-adrenoblockers and ACE inhibitors.
Interaction
Interaction
Amlodipine may be safely used for therapy of arterial hypertension together with thiazide diuretics, α-adrenoblockers, β-adrenoblockers or ACE inhibitors. In patients with stable angina pectoris amlodipine may be combined with other antianginal agents, such as long- or short-acting nitrates, β-adrenoblockers.
Unlike other BCAAs, clinically significant interaction of amlodipine (BCAA III generation) has not been found when combined with NSAIDs, including indomethacin.
The antianginal and hypotensive effects of BCAA may be enhanced when used with thiazide and loop diuretics, ACE inhibitors, β-adrenoblockers and nitrates, and their hypotensive effects may be increased when combined with α1-adrenoblockers and neuroleptics.
While no negative inotropic effects have generally been observed with amlodipine, some BCAAs can exacerbate the negative inotropic effects of antiarrhythmic agents that cause QT interval prolongation (e.g., amiodarone and quinidine).
Amlodipine may also be safely used concomitantly with oral antibiotics and hypoglycemic agents.
A single administration of 100 mg sildenafil in patients with essential hypertension has no effect on the pharmacokinetic parameters of amlodipine.
The repeated use of amlodipine in dose of 10 mg and atorvastatin in dose of 80 mg is not accompanied by significant changes in pharmacokinetic parameters of atorvastatin.
Simvastatin: Simultaneous repeated use of amlodipine in dose of 10 mg and simvastatin in dose of 80 mg leads to 77% increase of simvastatin exposure. In such cases, the dose of simvastatin should be limited to 20 mg.
Ethanol (beverages containing alcohol): Amlodipine in single and repeated use in a dose of 10 mg does not affect the pharmacokinetics of ethanol.
Antiviral agents (ritonavir): increases plasma concentrations of BCAAs, including amlodipine.
Neuroleptics and isoflurane: increases the hypotensive effect of dihydropyridine derivatives.
Calcium preparations may decrease the effect of BKC.
When concomitant use of BPC with lithium preparations (no data available for Norvasc®), there may be an increase of their neurotoxicity (nausea, vomiting, diarrhea, ataxia, tremor, tinnitus).
There have been no studies of concomitant use of amlodipine and cyclosporine in healthy volunteers and all groups of patients, except for patients after kidney transplantation. Various studies on the interaction of amlodipine with cyclosporine in patients after kidney transplantation show that the use of this combination may not lead to any effect or increase the Cmin of cyclosporine to varying degrees up to 40%. These data should be taken into account and cyclosporine concentrations should be monitored in this group of patients when concomitant use of cyclosporine and amlodipine.
There is no effect on the serum concentration of digoxin and its renal clearance.
There is no significant effect on the effect of warfarin (PV).
Cimetidine does not affect the pharmacokinetics of amlodipine.
In in vitro studies amlodipine does not affect the binding to plasma proteins of digoxin, phenytoin, warfarin and indomethacin.
Grapefruit juice: Concomitant administration of 240 mg of grapefruit juice and 10 mg of oral amlodipine is not accompanied by significant changes in amlodipine pharmacokinetics. However, it is not recommended to use grapefruit juice and amlodipine concomitantly, since a genetic polymorphism of CYP3A4 isoenzyme may increase bioavailability of amlodipine and, therefore, increase its hypotensive effect.
Aluminum- or magnesium-containing antacids: their single administration has no significant effect on amlodipine pharmacokinetics.
PUR3A4 isoenzyme inhibitors: concomitant use of diltiazem 180 mg and amlodipine 5 mg in elderly patients (69 to 87 years) with arterial hypertension shows 57% increase of systemic amlodipine exposure. Concomitant use of amlodipine and erythromycin in healthy volunteers (18 to 43 years) does not result in significant changes in amlodipine exposure (22% increase in AUC). Although the clinical significance of these effects is unclear, they may be more pronounced in older patients.
Powerful inhibitors of CYP3A4 isoenzyme (e.g. ketoconazole, itraconazole) may lead to increased plasma concentrations of amlodipine to a greater extent than diltiazem. Caution should be exercised when using amlodipine and CYP3A4 isoenzyme inhibitors.
CYP3A4 isoenzyme inducers: There are no data on the effect of CYP3A4 isoenzyme inducers on amlodipine pharmacokinetics. BP should be carefully monitored when concomitant use of amlodipine and CYP3A4 isoenzyme inducers.
Special Instructions
Special Instructions
Dental hygiene should be maintained and monitoring by a dentist (to prevent soreness, bleeding and gum hyperplasia).
In elderly patients, the T1/2 may be prolonged and drug clearance decreased. No change in doses is required, but closer monitoring of patients in this category is necessary.
The efficacy and safety of Norvasc® in hypertensive crisis have not been established.
Although there is no withdrawal syndrome in BKD, discontinuation of Norvasc® treatment should preferably be done by gradually reducing the dose of the drug.
Amlodipine has been associated with an increased incidence of pulmonary edema in patients with nonischemic CHF class III and IV according to NYHA, despite no signs of worsening heart failure.
Impact on the ability to drive vehicles and operate machinery.
While during the use of the drug Norvasc® no adverse effect on the ability to drive motor transport or operate other mechanisms was observed, however due to possible excessive pressure drop, dizziness, somnolence and other adverse reactions the following measures should be taken with caution, especially at the beginning of treatment and when increasing a dose.
Contraindications
Contraindications
With caution: Liver failure; chronic heart failure of non-ischemic etiology of NYHA functional class III-IV; unstable stenocardia; aortic stenosis; mitral stenosis; hypertrophic obstructive cardiomyopathy; acute myocardial infarction (and period within 1 month after it); sinus node weakness syndrome (significant tachycardia, bradycardia); arterial hypotension; simultaneous use with inhibitors or inducers of CYP3A4 isoenzyme.
Side effects
Side effects
Cardiovascular system: common – palpitations, peripheral edema (ankles and feet), skin flushing; infrequent – excessive decrease of BP; very rare – fainting, dyspnea, vasculitis, orthostatic hypotension, development or aggravation of CHF, cardiac rhythm disorders (including bradycardia, ventricular tachycardia and atrial fibrillation), myocardial infarction, pain in the chest.
Musculoskeletal system disorders: infrequent – arthralgia, muscle cramps, myalgia, back pain, arthrosis; rarely – myasthenia.
Nervous system disorders: frequent – headache, dizziness, increased fatigue, somnolence; infrequent – asthenia, general malaise, hypoesthesia, paresthesia, peripheral neuropathy, tremor, insomnia, mood lability, unusual dreams, increased excitability, depression, anxiety, tinnitus, perversion of taste; very rare – migraine, increased sweating, apathy, agitation, ataxia, amnesia.
Digestive system disorders: frequent – nausea, abdominal pain; infrequent – vomiting, constipation or diarrhea, flatulence, dyspepsia, anorexia, dry oral mucosa, thirst; rare – gum hyperplasia, increased appetite; very rare – pancreatitis, gastritis, jaundice (due to cholestasis), hyperbilirubinemia, increased activity of liver transaminases, hepatitis.
Hematopoietic organs: very rarely – thrombocytopenic purpura, leukopenia, thrombocytopenia.
Respiratory system disorders: infrequent dyspnea, rhinitis, nasal bleeding; very rare – cough.
Sensory system disorders: infrequent – diplopia, accommodation disorders, xerophthalmia, conjunctivitis, eye pain, visual disturbances.
Urogenital system disorders: infrequent – frequent urination, painful urination, nycturia, erectile dysuria; very rare – dysuria, polyuria.
Skin disorders: rare – dermatitis; very rare – alopecia, xeroderma, cold sweats, impaired skin pigmentation.
Metabolic disorders: very rare – hyperglycemia; infrequent – weight gain/loss.
Allergic reactions: infrequent – skin itching, rash (including erythematous, maculopapular rash, urticaria); very rare – angioedema, erythema multiforme.
Laboratory measures: very rarely – hyperglycemia.
Other: infrequent – chills, gynecomastia; very rare – parosmia.
Overdose
Overdose
Symptoms: pronounced BP decrease with possible development of reflex tachycardia and excessive peripheral vasodilation (pronounced and persistent arterial hypotension is possible, including with the development of shock and death).
The treatment: administration of activated charcoal (especially during the first 2 hours after overdose), gastric lavage, elevation of the lower extremities, active support of cardiac function, monitoring of cardiac and lung function parameters, control of blood pressure and diuresis.
In order to restore vascular tone – administration of vasoconstrictors (if there are no contraindications for their use); to eliminate the consequences of calcium channel blockade – IV administration of calcium gluconate. Hemodialysis is ineffective.
Pregnancy use
Pregnancy use
The safety of the drug Norvasc in pregnancy has not been established; therefore, its use in pregnancy is possible only when the estimated benefit to the mother outweighs the potential risk to the fetus.
There are no data indicating excretion of amlodipine with breast milk.
However, other slow calcium channel blockers (dihydropyridine derivatives) are known to be excreted with breast milk.
In this regard, if it is necessary to use the drug Norvasc during lactation, the question of stopping breast-feeding should be considered.
Similarities
Similarities
Additional information
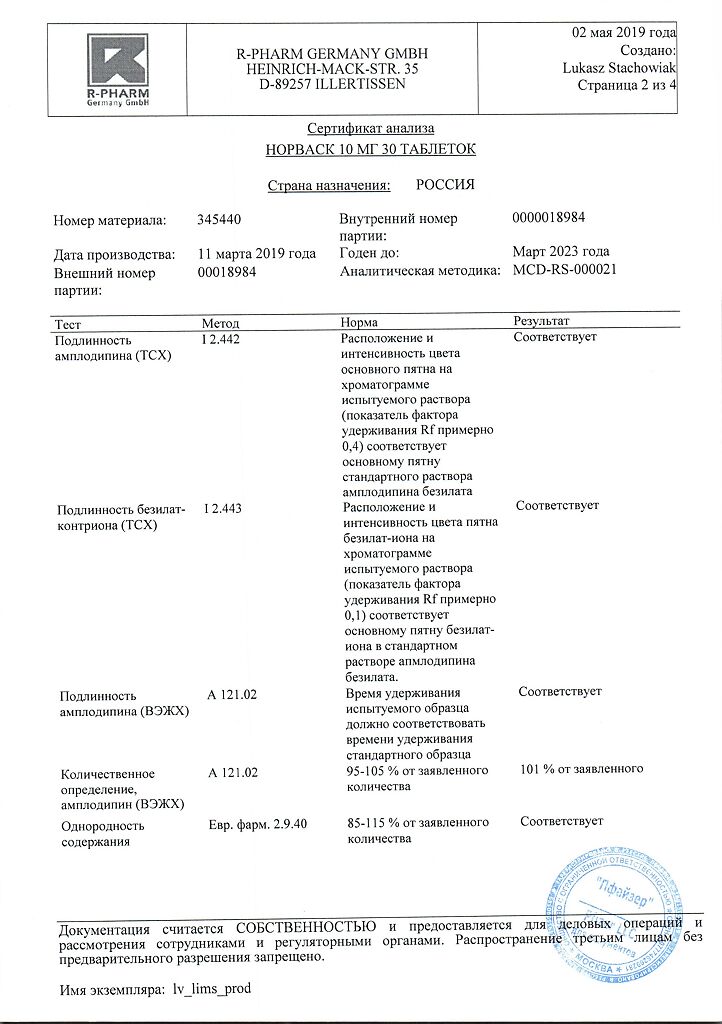
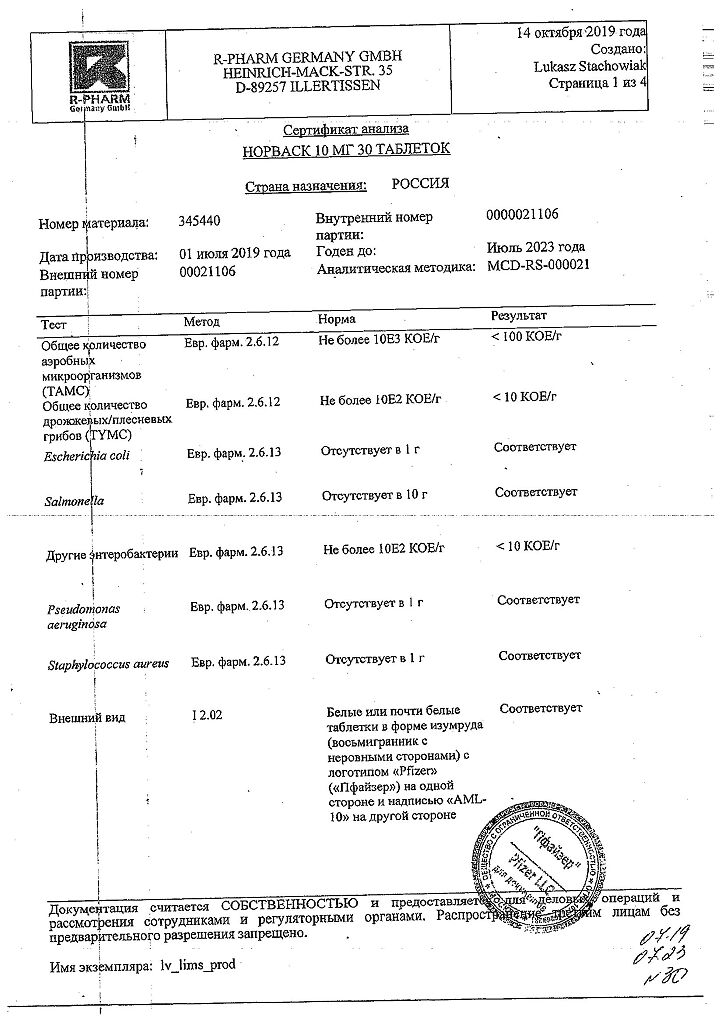
| Shelf life | 4 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
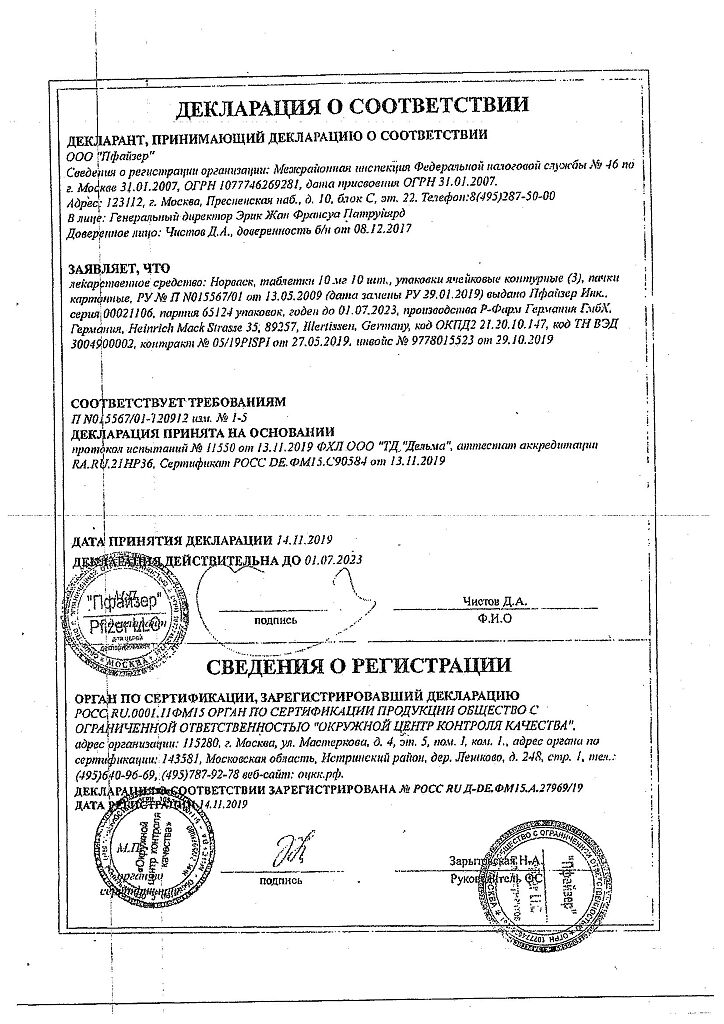
| Manufacturer | Pfizer, Puerto Rico |
| Medication form | pills |
| Brand | Pfizer |
Other forms…
Related products
Buy Norvasc, tablets 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.