No products in the cart.
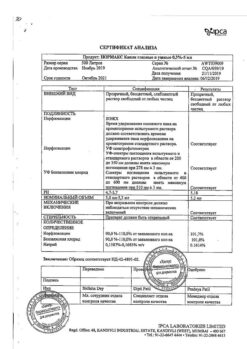
Norfloxacin, 400 mg 10 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Infections caused by Norfloxacin-sensitive strains of microorganisms.
Infections of the urinary tract:
– uncomplicated urinary tract infections (including. cystitis) caused by Enterococcus faecalis, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa, Staphylococcus epidermidis, Staphylococcus saprophyticus, Citrobacter freundii, Enterobacter aerogenes, Enterobacter cloacae, Proteus vulgaris, Staphylococcus aureus or Streptococcus agalactiae in the absence of an alternative treatment option;
– complicated urinary tract infections caused by Enterococcus faecalis, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa or Serratia marcescens.
Sexually transmitted diseases (see Precautions): Uncomplicated urethral and cervical gonorrhea caused by Neisseria gonorrhoeae.
Prostatitis caused by Escherichia coli.
Active ingredient
Active ingredient
Composition
Composition
One film-coated tablet contains:
the active ingredient: norfloxacin – 400,000 mg;
excipients: microcrystalline cellulose – 143,000 mg; croscarmellose sodium – 36,000 mg; povidone (polyvinylpyrrolidone low molecular weight) – 12,000 mg; colloidal silicon dioxide – 3,000 mg; magnesium stearate – 6,000 mg;
film coating: [hypromellose, 9,000 mg; hyprolose (hydroxypropyl cellulose), 3,490 mg; talc, 3,470 mg; titanium dioxide, 1,956 mg; iron oxide yellow (iron oxide), 0.084 mg] or [dry film coating mixture, containing hypromellose (50%), hyprolose (hydroxypropyl cellulose) (19.4%), talc (19.26%), titanium dioxide (10.87%), iron oxide yellow (iron oxide) (0.47%)] – 18,000 mg.
How to take, the dosage
How to take, the dosage
Ingestion at least 1 h before or at least 2 h after a meal with a glass of water.
The safety and effectiveness of oral administration of norfloxacin in children, adolescents, nursing mothers and during pregnancy have not been established.
Disabilities and potentially irreversible serious adverse reactions, including tendinitis and tendon rupture, peripheral neuropathy, and effects on the CNS
The use of fluoroquinolones, including norfloxacin, has been associated with disabling and potentially irreversible serious adverse reactions from different body systems that may occur simultaneously in the same patient. Common adverse reactions include tendinitis, tendon rupture, arthralgia, myalgia, peripheral neuropathy, and CNS effects (hallucinations, anxiety, depression, insomnia, severe headaches, and confusion). These reactions may occur within hours or weeks after initiation of norfloxacin, occur in patients of any age and in the absence of prior risk factors.
The first signs or symptoms of any serious adverse reaction should be discontinued with norfloxacin. The use of norfloxacin should be avoided in patients who have previously had serious adverse reactions associated with the use of fluoroquinols.
Tendinitis and tendon rupture
The use of fluoroquinolones, including norfloxacin, is associated with an increased risk of tendinitis and tendon rupture at any age. This adverse reaction most commonly affects the Achilles tendon, but rotator cuff of the shoulder, arm tendons, biceps muscle, thumb, and other tendons have also been reported. Tendinitis or tendon rupture may occur within hours or days of starting norfloxacin, or within months of completing therapy. Tendinitis and tendon rupture can occur bilaterally.
The risk of tendinitis and tendon rupture associated with fluoroquinolones is increased in patients over 60 years of age receiving GCS and in patients with kidney, heart, or lung transplants. Other factors that may independently increase the risk of tendon rupture include heavy exercise, renal insufficiency, and previous tendon diseases such as rheumatoid arthritis. Tendinitis and tendon rupture have also been observed in patients receiving fluoroquinolones who did not have the above risk factors.
If a patient experiences pain, swelling, inflammation, or tendon rupture, the use of norfloxacin should be stopped immediately. Fluoroquinolones, including norfloxacin, should be avoided if the patient has a history of tendon disease, tendonitis or tendon rupture. The patient should be warned to rest at the first sign of tendinitis or tendon rupture and to contact the attending physician about switching to another antimicrobial therapy without fluoroquinolones.
Peripheral neuropathy
The development of sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons and resulting in paresthesia, hypoesthesia, dysesthesia and weakness has been reported in patients receiving fluoroquinolones, including norfloxacin. Symptoms may occur soon after starting norfloxacin and may be irreversible in some patients. The use of norfloxacin should be stopped immediately if the patient has symptoms of peripheral neuropathy, such as pain, burning, tingling, numbness and/or weakness, or other changes in sensation (light touch, pain, temperature, position sensation, vibration and/or muscle strength) in order to minimize the possibility of developing an irreversible condition. In patients with previously observed peripheral neuropathy, fluoroquinolones, including norfloxacin, should be avoided.
CNS reactions
The use of fluoroquinolones, including norfloxacin, is associated with an increased risk of CNS effects, including reactions such as seizures, increased IOP (including pseudotumor cerebri) and toxic psychoses. Quinolones may also stimulate the CNS, leading to the development of tremors, restlessness, dizziness, confusion, and hallucinations. If these reactions occur in patients receiving norfloxacin, the drug should be discontinued and appropriate measures taken.
The effects of norfloxacin on brain function or electrical activity of the brain have not been studied. Therefore, norfloxacin should be used with caution in patients with known or suspected CNS abnormalities such as severe cerebral arteriosclerosis, epilepsy, and other factors predisposing to seizures.
The exacerbation of myasthenia gravis
Norfloxacin has neuromuscular blocker properties and may exacerbate muscle weakness in patients with myasthenia gravis. In the post-registration period, serious adverse reactions, including fatalities and the need for ventilatory ventilation, associated with the use of fluoroquinolones in patients with myasthenia gravis have been observed. The use of norfloxacin in patients with a history of myasthenia gravis should be avoided.
Hypersensitivity reactions
Serious and sometimes fatal hypersensitivity reactions (anaphylaxis), some of which occurred after the first dose, have been reported in patients receiving therapy with fluoroquinolones, including norfloxacin. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, tingling, swelling of the throat or face, dyspnea, urticaria, and itching. Only a few patients have a history of hypersensitivity reactions. If an allergic reaction to norfloxacin occurs, its administration should be discontinued. Serious acute hypersensitivity reactions require immediate emergency treatment with epinephrine. Oxygen, IV fluids, antihistamines, GCS, pressor amines and respiratory monitoring including intubation should be used when indicated.
Diarrhea associated with Clostridium difficile
Cases of diarrhea associated with Clostridium difficile (CDAD) have been reported with almost all antibacterial drugs, including norfloxacin, and their severity can range from mild to fatal colitis. Treatment with antibacterial drugs alters the normal colon microflora, leading to an overgrowth of C. difficile, producing toxins A and B, which contribute to the development of CDAD. C. difficile strains with hyperproduction of toxins cause increased morbidity and mortality because they may be immune to antimicrobial therapy, and colectomy may be required. The possibility of CDAD should be considered in all patients with diarrhea after antibiotics. Careful history taking is necessary, as it has been reported that CDAD may occur for more than 2 months after antibiotic therapy.
If CDAD is suspected or confirmed, it may be necessary to discontinue antibiotics that have no direct effect on C. difficile. Appropriate fluid and electrolyte monitoring, additional protein administration, treatment of C. difficile infection with antibiotics, and evaluation of the need for surgical intervention should be performed according to the clinical indication.
The treatment of syphilis
The efficacy of norfloxacin in the treatment of syphilis has not been proven. Antimicrobial drugs used in high doses for a short period of time to treat gonorrhea may mask or delay symptoms of incubating syphilis. All patients with gonorrhea should have a serologic test for syphilis at the time of diagnosis. Patients receiving norfloxacin should have a control serologic test for syphilis after 3 months.
Other precautions
In a double-blind, cross-over comparative study, needle-like crystals were found in the urine of some volunteers who received either placebo or 800 or 1600 mg of norfloxacin (the recommended or twice the recommended daily dose). Although crystalluria is not normally expected at the 400 mg twice daily dose, as a precaution, the recommended daily dose should not be exceeded, and the patient is advised to take adequate fluids to ensure adequate hydration and adequate diuresis.
In patients with impaired renal function, the dosing regimen should be modified according to the recommendations in the instructions for medical use.
The use of quinolone antibacterial drugs may be associated with the development of moderate to severe photosensitivity/phototototoxicity after sun or UV exposure. Phototoxicity may manifest as a marked reaction to sunburn (e.g., burning, erythema, exudation, blistering, edema) in areas normally exposed to light (face, neck, extensor surfaces of the forearms, back of the hands). Excessive exposure to light sources should be avoided. If phototoxicity occurs, the drug should be discontinued.
In rare cases hemolytic reactions have been reported in patients with latent or known glucose-6-phosphate dehydrogenase activity disorders receiving quinolone antibacterial drugs, including norfloxacin (see “Adverse effects”).
Prescribing norfloxacin in the absence of proven or strongly suspected bacterial infection or for prophylaxis increases the risk of development of drug-resistant bacteria.
Elderly age
Elderly patients are at increased risk of severe tendon disease, including tendon rupture, when using norfloxacin. This risk is further increased in patients receiving concomitant GCS therapy. Caution should be exercised when prescribing norfloxacin to elderly patients. Patients should be informed about the potential side effects and if symptoms of these conditions appear, norfloxacin should be discontinued and their physician should be consulted.
The increased risk of other adverse reactions in the elderly cannot be excluded.
Norfloxacin is known to be largely excreted by the kidneys and the risk of adverse reactions may be higher in patients with impaired renal function. Since elderly patients are more likely to have impaired renal function, caution should be exercised in dose selection and renal function should be monitored.
In general, elderly patients may be more susceptible to prolongation of the QTc interval. Therefore, caution should be exercised when concomitant use of norfloxacin and drugs that may lead to QTc interval prolongation (e.g., class IA or III antiarrhythmic agents) or in patients with risk factors for torsade de pointes (e.g., known QTc prolongation, unadjusted hypokalemia).
Interaction
Interaction
In vitro quinolones, including norfloxacin, have been shown to inhibit CYP1A2. Concomitant use of norfloxacin with drugs metabolized with participation of this isoenzyme (e.g., caffeine, clozapine, ropinirole, tacrine, theophylline, tizanidine) may lead to increased concentration of these drugs when used in usual doses. Patients receiving any of these drugs concomitantly with norfloxacin should be closely monitored.
In concomitant use with quinolones elevated plasma levels of theophylline have been reported. Theophylline-related side effects have been reported in patients receiving concomitant therapy with norfloxacin and theophylline. Therefore, consideration should be given to monitoring plasma theophylline levels and adjusting theophylline dose if necessary.
Elevated serum levels of cyclosporine have been reported when used concomitantly with norfloxacin. Therefore, when concomitant use of these drugs, serum levels of cyclosporine should be monitored and the dose should be adjusted accordingly.
The quinolones including norfloxacin may increase the effect of oral anticoagulants including warfarin or its derivatives or similar drugs. If these drugs are used concomitantly, PV should be carefully monitored or other appropriate coagulation tests should be performed.
The concomitant use of quinolones, including norfloxacin, with glyburide (sulfonylurea derivative) has rarely resulted in severe hypoglycemia. Therefore, it is recommended to monitor blood glucose levels when using them concomitantly.
A decrease in urinary excretion of norfloxacin has been reported with probenecid.
The concomitant use of nitrofurantoin and norfloxacin is not recommended because nitrofurantoin may counteract the antibacterial effect of norfloxacin in the urinary tract.
Multivitamins, didanosine in the form of chewable/buffered tablets, drugs containing iron or zinc, antacids or sucralfate should not be used simultaneously with norfloxacin or within 2 h after administration of norfloxacin because they may interfere with absorption and lead to lower serum and urinary levels of norfloxacin.
Particular quinolones have been shown to affect caffeine metabolism. This may lead to decreased caffeine clearance and increased T1/2 from plasma, which may lead to plasma accumulation of caffeine when concomitantly used with norfloxacin.
The concomitant use of NSAIDs with quinolones, including norfloxacin, may increase the risk of CNS stimulation and development of seizures. Caution should be exercised when using norfloxacin in patients concomitantly receiving NSAIDs.
Special Instructions
Special Instructions
Use the drug with caution in the following diseases:
Epilepsy, seizure syndrome, renal/liver failure, myasthenia gravis.
During the treatment patients should get plenty of fluids (under diuresis control).
During the therapy it is possible to increase prothrombin index (during surgical interventions the state of the blood clotting system should be controlled).
During treatment it is necessary to avoid direct sunlight.
Norfloxacin, like other fluoroquinolones, may cause tendinitis and tendon rupture. Risk factors: age older than 60 years; taking glucocorticosteroids; kidney, heart, or lung transplant; increased physical activity; CKD; tendonitis in anamnesis (including rheumatoid arthritis). These phenomena may also occur several months after the end of the drug. At the first signs of tendinitis or tendon rupture it is necessary to stop using norfloxacin and consult a physician.
Norfloxacin may decrease seizure threshold and cause seizures; fluoroquinolones may also stimulate the CNS, causing tremors, toxic psychosis, restlessness, confusion and hallucinations; increased intracranial pressure.
Norfloxacin may lead to the development of pseudomembranous colitis caused by Clostridium difficile. In this case it is necessary to cancel the drug and prescribe appropriate treatment (use of oral vancomycin or metronidazole).
It is not effective in syphilis.
Norfloxacin may cause peripheral neuropathy (paresthesias, hypoesthesia, dysesthesias, muscle weakness). At the first signs of neuropathy (pain, tingling, numbness or weakness in the extremities, other types of sensitivity disorders) the drug should be stopped to avoid irreversible changes.
In order to avoid formation of norfloxacin crystals in the kidneys, the recommended doses should not be exceeded; the tablets should be infused with sufficient fluid.
Contraindications
Contraindications
Side effects
Side effects
Single-dose studies
In clinical studies involving 82 healthy volunteers and 228 patients with gonorrhea who received a single dose of norfloxacin, 6.5% of subjects reported side effects related to the medication. However, the data below are calculated without regard to the association with the use of the drug.
The most frequent adverse events (>1%) were dizziness (2.6%), nausea (2.6%), headache (2%), and abdominal cramps (1.6%). In addition, anorexia, diarrhea, hyperhidrosis, asthenia, anal/rectal pain, constipation, dyspepsia, flatulence, tingling in the fingers, and vomiting were reported with a frequency of 0.3-1%.
Diagnostic abnormalities suspected to be related to norfloxacin use have been reported in 4.5% of patients/healthy volunteers. These abnormalities included increased AST levels (1.6%), decreased white blood cell count (1.3%), decreased platelet count (1.0%), increased urinary protein levels (1.0%), decreased hematocrit and Hb levels (0.6%), and increased eosinophil count (0.6%).
Studies with multiple doses
In clinical studies involving 52 healthy volunteers and 1980 patients with urinary tract infections or prostatitis who received multiple doses of norfloxacin, 3.6% of subjects reported side effects associated with the drug. However, the data below are calculated without regard to the association with drug use.
The most frequent adverse events (>1%) were nausea (4.2%), headache (2.8%), dizziness (1.7%), and asthenia (1.3%). In addition, abdominal pain, back pain, constipation, diarrhea, dry mouth, dyspepsia/irritation, fever, flatulence, hyperhidrosis, fluid stools, itching, rash, drowsiness, and vomiting were reported with a frequency of 0.3-1%.
. Less frequent reactions (0.1-0.2%) included abdominal bloating, allergy, anorexia, anxiety, bitter taste in the mouth, blurred vision, bursitis, chest pain, chills, depression, dysmenorrhea, edema, erythema, foot or hand swelling, insomnia, oral ulcers, myocardial infarction, palpitations, anal itching, renal colic, sleep disturbances, and urticaria.
The abnormal laboratory findings seen in these patients/healthy volunteers included eosinophilia (1.5%), increased ALT levels (1.4%), decreased white blood cell and/or neutrophil counts (1.4%), increased AST levels (1.4%) and ALP (1.1%). Less common abnormalities were increased urine protein levels, elevated serum LDH, serum creatinine levels, decreased hematocrit, and glucosuria.
Post-registration experience
The most common adverse reaction reported in the post-registration period was rash.
There have been reports of CNS effects characterized by generalized seizures, myoclonus, and tremor associated with the use of norfloxacin (see Precautions). There have been reports of visual disturbances when taking this class of drugs.
The following additional adverse reactions have been reported since norfloxacin was marketed.
Hypersensitivity reactions, including anaphylactoid reactions, angioedema, dyspnea, vasculitis, urticaria, arthritis, arthralgia and myalgia (see Precautions).
Skin disorders: toxic epidermal necrolysis, Stevens-Johnson syndrome and erythema multiforme, exfoliative dermatitis, photosensitivity/phototototoxicity reactions, leukocytoclastic vasculitis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome).
Gastrointestinal disorders: pseudomembranous colitis, hepatitis, jaundice, including cholestatic, and increased liver function tests, pancreatitis (rare), stomatitis. Symptoms of pseudomembranous colitis may appear during or after antibiotic treatment (see Precautions).
Hepatic disorders: liver failure, including fatal.
CRC: rarely – prolongation of the QTc interval and ventricular arrhythmia, including torsade de pointes.
Renal side: interstitial nephritis, renal failure.
Nervous system disorders/psychiatric disorders: peripheral neuropathy, which may be irreversible, Guillain-Barré syndrome, ataxia, paresthesia, hypoesthesia, psychiatric disorders, including psychotic reactions and confusion.
Muscular system disorders: tendinitis, tendon rupture, exacerbation of myasthenia gravis (see Precautions), elevated creatine kinase levels, muscle spasms.
Blood disorders: neutropenia, leukopenia, agranulocytosis, hemolytic anemia, sometimes associated with glucose-6-phosphate dehydrogenase deficiency, thrombocytopenia.
Sensory organs: hearing loss, tinnitus, diplopia, dysgeusia.
Other adverse events associated with quinolone use include albuminuria, candiduria, crystalluria, cylinduria, dysphagia, elevated blood glucose, elevated serum Chs, potassium, triglycerides, hematuria, hepatic necrosis, symptomatic hypoglycemia, nystagmus, postural hypotension, prolonged PV and vaginal candidiasis.
Overdose
Overdose
When norfloxacin is administered in doses up to 4 g/kg in male and female mice and rats, no significant mortality has been observed.
The treatment: in case of acute overdose vomiting or gastric lavage should be induced, the patient should be closely monitored and appropriate symptomatic and supportive treatment should be given. Adequate hydration should be provided.
Pregnancy use
Pregnancy use
Adequate and well-controlled studies in pregnant women have not been conducted. Norfloxacin should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
It is not known whether norfloxacin is excreted with breast milk. Because other drugs in this class are secreted with breast milk, and because of the possibility of serious adverse reactions in breastfed infants, a decision should be made to discontinue breastfeeding or to discontinue norfloxacin, given its importance to the mother.
Similarities
Similarities
Additional information
| Shelf life | 3 years. Do not use after the expiration date. |
|---|---|
| Conditions of storage | The drug should be stored at a temperature not exceeding 25 ° C in a place out of the reach of children. |
| Manufacturer | Vertex, Russia |
| Medication form | pills |
| Brand | Vertex |
Other forms…
Related products
Buy Norfloxacin, 400 mg 10 pcs with delivery to USA, UK, Europe and over 120 other countries.