No products in the cart.
Nifekard XL, 30 mg 60 pcs
€10.85 €9.49
Description
Pharmacotherapeutic group:
Slow calcium channel blocker.
TAC code: C08CA05.
Pharmacological properties
Pharmacodynamics
Nifedipine is a selective slow calcium channel blocker, a 1,4-dihydropyridine derivative. It has antianginal and antihypertensive effects. Reduces the flow of extracellular calcium inside cardiomyocytes and smooth muscle cells of coronary and peripheral arteries; in high doses it inhibits the release of calcium ions from intracellular depots. Reduces the number of functioning channels without affecting the time of their activation, inactivation and recovery.
Disrupts excitation and contraction processes in myocardium mediated by tropomyosin and troponin, in vascular smooth muscle mediated by calmodulin. In therapeutic doses, it normalizes the transmembrane flow of calcium ions impaired in a number of pathological conditions, primarily in arterial hypertension. It does not affect the tone of the veins. It increases coronary blood flow, improves blood supply to ischemic areas of myocardium without development of the phenomenon of “bypassing”, activates the functioning of collaterals.
It improves myocardial function, reduces the force of heart contractions and myocardial oxygen demand. By dilating the peripheral arteries, it reduces blood pressure (BP) and reduces total peripheral resistance and afterload on the heart. Almost has no effect on the sinoatrial and atrioventricular nodes. Increases renal blood flow, causes moderate natriuresis.
Inhibits platelet aggregation, has antiatherogenic properties (especially with long-term use). Lowers the pressure in the pulmonary artery, has a positive effect on the blood supply to the brain vessels.
Pharmacokinetics
Nifecard® XL, due to delayed release of the active substance, provides a gradual controlled increase in plasma concentrations of nifedipine. Plasma concentration of nifedipine reaches a plateau after approximately 6 hours and is maintained with slight fluctuations for 24 hours. Nifedipine is rapidly and almost completely absorbed after oral administration (92-98%). It is characterized by a high percentage of binding to plasma proteins (90%). The elimination half-life is about 2 hours. It is metabolized in the liver. No active metabolites were found. It is excreted as inactive metabolites mainly by kidneys (80%) and with bile (20%).
Nifedipine penetrates through the blood-brain barrier and placental barrier, is excreted with breast milk.
There is no cumulative effect.
Chronic renal failure, hemodialysis and peritoneal dialysis do not affect pharmacokinetics.
In impaired hepatic function the clearance of nifedipine is reduced. Dose adjustment may be required in severe hepatic impairment.
In elderly patients, when administered intravenously, nifedipine clearance was reduced by 33% compared with young healthy volunteers.
The development of nifedipine tolerance may be observed with long-term use.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Modified release film-coated tablets.
Each modified-release film-coated tablet contains:
core:
nifedipine 30.00 mg/60.00 mg, respectively;
povidone 75.00/150.00 mg,
sodium lauryl sulfate 2.40/4.80 mg,
hypromellose (hydroxypropyl methylcellulose) 185.80/(-) mg,
hypromellose (hydroxypropyl methylcellulose 2906) (-)/203.84 mg,
Hypromellose (hydroxypropyl methylcellulose 2208) (-)/123.36 mg,
*Ludipress® 70.00/50.00 mg,
p> magnesium hydrosilicate (talc) 6.00/6.00 mg,
magnesium stearate 0.80/2.00 mg;
coating:
Hypromellose phthalate (hydroxypropyl methylcellulose phthalate) 18,200/40,000 mg, triethylcitrate 1,800/4,000 mg, hypromellose (hydroxypropyl methylcellulose 2910) 3,000/4,500 mg, Hyprolose (hydroxypropyl cellulose) 3,000/4,500 mg, macrogol (polyethylene glycol) 1.0/1.5 mg, magnesium disilicate (talc) 0.500/0.750 mg, titanium dioxide 1.930/2.900 mg, iron oxide yellow dye 0.570/0.850 mg.
*Ludipress® is a mixture of lactose monohydrate, povidone, crosspovidone in the ratio 93:3.5:3.5.
How to take, the dosage
How to take, the dosage
The tablets should be taken at the same time of the day, without chewing; they should not be crushed or divided. The dosing regimen is set individually. The tablets should not be washed down with grapefruit juice.
The dose of Nifekard® XL is 1 tablet of the drug 30 mg or 60 mg once daily. The dose is started at 30 mg/day and is corrected at 7-14 day intervals.
The maximum daily dose of Nifekard® XL is 90 mg.
It is possible that excretion of nifedipine may be slower in elderly patients, so lower maintenance doses of the drug may be required compared to younger patients.
In patients with impaired hepatic function, the use of nifedipine should be closely monitored and a reduction in the drug dose may be required if necessary.
In patients with impaired renal function no dose adjustment is required.
Patients with severe cerebrovascular disease should be treated with a low dose.
If discontinuation of Nifecard® XL is necessary, the dose should be reduced gradually.
Interaction
Interaction
Nifedipine is metabolized primarily by the CYP3A4 isoenzyme, so drugs that inhibit or induce this enzyme may alter the presystemic metabolism or clearance of nifedipine.
CYP3A4 isoenzyme inducers
Rifampicin
Rifampicin is a strong inducer of the CYP3A4 system. When concomitant use with rifampicin the bioavailability of nifedipine is significantly reduced and effective plasma concentrations cannot be achieved.
Phenytoin, carbamazepine, phenobarbital
Phenytoin induces CYP3A4 isoenzyme. It can decrease the bioavailability of nifedipine and reduce its effectiveness. If phenytoin and nifedipine are used concomitantly the clinical effect of the latter should be evaluated and if necessary the dose should be increased.
If the dose of nifedipine was increased during combination therapy, this should be taken into account when withdrawing phenytoin.
There have been no reliable studies of interaction between nifedipine and carbamazepine and phenobarbital when used concomitantly. In other studies carbamazepine and phenobarbital decrease plasma concentration of another “slow” calcium channel blocker – nimodipine, therefore we cannot exclude the possibility of decrease of nifedipine plasma concentration when used simultaneously with carbamazepine and phenobarbital.
CYP3A4 isoenzyme inhibitors
The concomitant use of nifedipine and agents that have inhibitory effect on CYP3A4 isoenzyme causes increase of nifedipine plasma concentration.
The blood pressure should be monitored and if necessary the dose of nifedipine should be reduced.
Macrolide antibiotics (e.g., erythromycin)
Some macrolide antibiotics are known to inhibit CYP3A4-mediated metabolism of other drugs. Therefore, a potential increase in plasma concentration of nifedipine cannot be excluded when they are used together.
Azithromycin, although structurally close to the class of macrolide antibiotics, does not inhibit CYP3A4 isoenzyme.
HIV protease inhibitors (e.g., amprenavir, indinavir, nelfinavir, ritonavir or saquinavir)
There are no reliable clinical studies on drug interactions between nifedipine and HIV protease inhibitors. Drugs of this class are known to inhibit CYP3A4 isoenzyme. In addition, in an in vitro study, drugs of this class have been shown to inhibit the metabolism of nifedipine. When concomitant use of nifedipine with protease-HIV inhibitors, an increase in its plasma concentration cannot be excluded.
Imidazole derivatives (e.g., ketoconazole, itraconazole or fluconazole)
There have been no reliable studies on interaction of nifedipine with azole antifungal drugs, but the latter are known to inhibit CYP3A4 isoenzyme.
Concomitant oral administration with nifedipine cannot be ruled out an increase in its plasma concentration.
Fluoxetine
There have been no reliable studies on the interaction of nifedipine with fluoxetine.
In an in vitro study, fluoxetine has been shown to inhibit CYP3A4-mediated metabolism of nifedipine. Therefore, an increase in the plasma concentration of nifedipine when using them together cannot be excluded.
Nefazodone
There have been no reliable studies on the interaction of nifedipine and nefazodone.
In an in vitro study, nephadosone has been shown to inhibit CYP3A4-mediated metabolism of nifedipine. Therefore, an increase in the plasma concentration of nifedipine when they are used together cannot be excluded.
Qinupristin/dalfopristin
Concomitant use of quinupristin/dalfopristin and nifedipine may lead to increased plasma concentrations of the latter.
Valproic acid
There have been no reliable studies of interaction between nifedipine and valproic acid during concomitant use. In other studies valproic acid decreased plasma concentration of another “slow” calcium channel blocker – nimodipine; therefore we can not exclude the possibility of decrease of nifedipine plasma concentration with valproic acid.
Cimetidine
Due to inhibition of CYP3A4 isoenzyme, cimetidine increases plasma concentrations of nifedipine and may increase antihypertensive effect.
. Thus, when nifedipine is used concomitantly with cimetidine, quinupristine, dalfopristine, erythromycin, fluoxetine, nefazodone, valproic acid, protease-HIV inhibitors (e.g, amprenavir, indinavir, nelfinavir, ritonavir, or saquinavir) and azole derivatives (ketoconazole, itraconazole, or fluconazole) should be monitored and the drug dose should be reduced if necessary.
Other drugs that affect nifedipine metabolism
Cisapride
Concomitant use of cisapride and nifedipine may increase the plasma concentration of nifedipine.
Diltiazem
Diltiazem reduces the clearance of nifedipine and therefore increases the plasma concentration of nifedipine. Thus, caution should be exercised when using the drugs in combination and the dose of nifedipine should be reduced if necessary.
Cyclosporine
Simultaneous use may increase the plasma concentration of nifedipine.
The effects of nifedipine on other drugs
Hypotensive drugs
Nifedipine may enhance the antihypertensive effects of diuretics, beta-adrenoblockers, angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists, other “slow” calcium channel blockers, alpha-adrenoblockers, phosphodiesterase-5 (PDE-5) inhibitors, alpha-metaldopa.
When using nifedipine concomitantly with beta-adrenoblockers, close monitoring of the patient is required, since a worsening of symptoms of heart failure may occur (single cases have been described).
Digoxin
Concomitant use of nifedipine and digoxin may increase plasma concentrations of digoxin; therefore, serum digoxin concentrations should be monitored and the digoxin dose should be adjusted if necessary.
Hinidine
Concomitant use of nifedipine and quinidine decreases the plasma concentration of quinidine, and in some cases, when nifedipine is withdrawn, an increase in its plasma concentrations has been noted. Therefore, it is recommended to adjust the quinidine dose if necessary. Some authors indicate an increase in nifedipine plasma concentrations when both drugs are used simultaneously. Thus, BP should be monitored carefully, and if necessary, the dose of nifedipine should be decreased.
Tacrolimus
Cyclosporine has been shown to be metabolized by the CYP3A4 isoenzyme.
Published data indicate that it may be necessary to reduce the dose of tacrolimus when used concomitantly with nifedipine.
Vincristine
Concomitant use with nifedipine decreases the excretion of vincristine and may require a dose reduction.
Magnesium sulfate
Magnesium sulfate must be monitored carefully when administered intravenously to patients taking nifedipine because there may be a marked decrease in BP.
Cephalosporins
Simultaneous use with nifedipine increases plasma concentration of cephalosporins.
Phenytoin
Nifedipine may slow down the metabolism of phenytoin and increase its toxic effects.
In patients taking phenytoin, it is recommended to monitor the plasma concentration of phenytoin at the beginning of treatment with nifedipine.
Nitrates
Synergistic effects should be considered when nifedipine and nitrates are used simultaneously.
Theophylline
Nifedipine increases plasma concentrations of theophylline when used concomitantly.
Fentanyl
The concomitant use of nifedipine and fentanyl may result in marked arterial hypotension, so it is recommended that nifedipine (if possible) be stopped at least 36 hours before anesthesia with fentanyl.
Indirect anticoagulants
There have been rare reports of increased prothrombin time when nifedipine is used concomitantly with indirect anticoagulants (e.g., warfarin). The relationship to nifedipine therapy has not been established, the clinical significance of this effect is unknown.
Other forms of interaction
In spectrophotometric determination of vanillylmindalic acid in urine, nifedipine may cause false positive results. Other measurements are recommended.
Grapefruit juice
Grapefruit juice inhibits the CYP3A4 isoenzyme. When concomitantly taken, grapefruit juice increases the plasma concentration of nifedipine due to decreased presystemic metabolism. Due to increased bioavailability of nifedipine in patients with severe arterial hypertension or stable angina pectoris, ischemic complications (heart attack, unstable angina pectoris) may develop.
The consumption of grapefruit juice during treatment with nifedipine is not recommended.
There is no effect on the pharmacokinetics of nifedipine when nifedipine and acetylsalicylic acid, benazepril, candesartan, debrisokvin, doxazosin, irbesartan, omeprazole, orlistat, pantoprazole, ranitidine, rosiglitazone and triamterene/hydrochlorothiazide are used simultaneously.
Special Instructions
Special Instructions
It is recommended that treatment with Nifecard® XL be discontinued gradually.
Particularly after recent abrupt withdrawal of beta-adrenoblockers (the latter should be withdrawn gradually) an angina attack may occur at the start of treatment.
The concomitant use of beta-adreno-blockers should be performed under close medical supervision, as this may cause excessive BP reduction and in some cases worsen the symptoms of heart failure.
In severe heart failure, the drug is dosed with great caution.
Rarely, patients with severe coronary artery stenosis at the beginning of therapy or with increasing dose of nifedipine may increase the frequency and severity of angina pains, up to the development of myocardial infarction.
The diagnostic criteria for use of the drug in vasospastic angina are: classic clinical presentation accompanied by ST-segment elevation on ECG, occurrence of ergonovine-induced angina or coronary artery spasm, detection of coronarospasm on angiography, or detection of an angiospastic component without confirmation (e.g., different voltage threshold or unstable angina when electrocardiogram data suggest transient angiospasm).
In patients with severe hypertrophic obstructive cardiomyopathy, there is a risk of increased frequency, severity and duration of angina attacks after nifedipine use; in this case, withdrawal of the drug is necessary.
In patients with diabetes mellitus, plasma glucose concentrations may need to be monitored while using Nifekard® XL.
In patients on hemodialysis, with high BP and irreversible renal impairment, with reduced circulating blood volume, the drug should be used with caution; a sharp drop in BP may occur.
Patients with impaired liver function are monitored closely and if necessary, the dose of the drug is reduced and/or other dosage forms of nifedipine are used.
In patients with severe stenosis of any part of the gastrointestinal tract, development of intestinal obstruction is possible. In very rare cases, bezoars may develop, which may require surgery to remove. In isolated cases, symptoms of intestinal obstruction may be observed in patients without gastrointestinal pathology. The risk of bezoars is increased in patients with decreased intestinal peristalsis (constipation, gastroesophageal reflux, obesity, hypothyroidism, diabetes), intestinal tumors, diverticulitis, inflammatory bowel changes, vertical gastroplasty, gastric bypass, after resection of the small intestine, colostomy placement, as well as when concomitantly used with H2-histamine receptor blockers, opiates, nonsteroidal anti-inflammatory drugs, anticholinergic drugs, neuromuscular blockers (muscle relaxants), laxatives (laxatives).
There have been isolated reports of pills “sticking” to the intestinal wall with the formation of ulcers that required hospitalization and surgery.
Please note that barium-guided x-ray examination of the intestine may reveal false-positive polyp symptoms (a “filling” defect).
If the patient requires surgery under general anesthesia during therapy, the anesthesiologist must be informed of the nature of the therapy.
Nifedipine, like other slow calcium channel blockers, inhibits platelet aggregation in vitro. Few reports support evidence of a statistically significant decrease in platelet aggregation and increase in bleeding time. The clinical significance of this is not known.
Positive direct Coombs reaction and increased antinuclear antibody titers are possible during treatment.
Impact on ability to drive, operate machinery
When treating with Nifekard® XL, caution must be exercised while engaged in potentially hazardous activities requiring increased concentration and rapid psychomotor reaction, and alcohol must be avoided.
Special precautions for disposal of unused product
There is no need for special precautions for disposal of unused product.
Contraindications
Contraindications
Hypersensitivity to nifedipine or components of the drug and other 1,4-dihydropyridine derivatives;
– severe arterial hypotension (systolic blood pressure below 90 mm Hg).Severe aortic valve stenosis with clinically significant hemodynamic disorders;
– Unstable angina pectoris;
– Chronic heart failure in decompensation stage, cardiogenic shock (risk of myocardial infarction), acute period of myocardial infarction (during the first 4 weeks);
– concomitant use of rifampicin;
– rare hereditary forms of lactose intolerance, lactase deficiency or glucose/galactose absorption disorders (because the composition contains lactose).as it contains lactose);
– pregnancy before the 20th week, breastfeeding period;
– age under 18 years (efficacy and safety are not established).
With caution
Aortic or mitral valve orifice stenosis; hypertrophic obstructive cardiomyopathy; severe tachycardia; sinus node weakness syndrome; malignant arterial hypertension; myocardial infarction with left ventricular failure; cerebrovascular disease; hepatic and/or renal function disorders; hemodialysis (risk of arterial hypotension); diabetes mellitus; intestinal obstruction; pregnancy after 20 weeks; simultaneous use of beta-adrenoblockers or cardiac glycosides, with inducers or inhibitors of CYP3A4 isoenzyme.
Side effects
Side effects
According to the World Health Organization (WHO), adverse reactions are classified according to their frequency of development as follows: Very common (≥1/10), common (≥1/100, < 1/10), infrequent (≥1/1000, < 1/100), rare (≥1/10000, < 1/1000) and very rare (< 1/10000); frequency unknown – the incidence could not be determined from available data.
Blood and lymphatic system
frequency unknown: agranulocytosis, leukopenia, anemia, thrombocytopenia.
Immune system disorders
infrequent: allergic reactions, allergic edema/angioneurotic edema;
rare: skin itching, skin rash, urticaria;
frequency is unknown: anaphylactic/anaphylactoid reaction, toxic epidermal necrolysis, exfoliative dermatitis, photodermatitis, autoimmune hepatitis, thrombocytopenic purpura.
Metabolism and nutrition
frequency unknown: hyperglycemia.
Nervous system disorders
often: headache;
infrequently: dizziness, migraine, increased fatigue, tremor;
rarely: paresthesia/dysesthesia of the extremities;
frequency unknown: with long-term use in high doses – depression, anxiety, extrapyramidal (parkinsonian) disorders (ataxia, “mask-like” face, “shuffling” gait, stiffness of arm and leg movements, tremor of hands and fingers, difficulty swallowing, hyposthesia, sleepiness), increased excitability, sleep disorders (includingincluding insomnia), nightmares, decreased libido.
Visually impaired
infrequent: visual impairment (transient);
frequency unknown: eye pain.
Hearing organ and labyrinth disorders
infrequent: “ringing” in the ears, dysgeusia (taste disorder).
Cardiovascular system disorders
often: peripheral edema, increased symptoms of vasodilation (asymptomatic BP decrease, “rushes” of blood to the facial skin, facial hyperemia, feeling of fever);
infrequently: tachycardia, palpitations, arrhythmia, excessive BP reduction (especially in patients on dialysis with malignant hypertension and reduced circulating blood volume), syncope, syncope;
very rare: in some patients, especially at the beginning of treatment, angina attacks may occur, which requires withdrawal of the drug. There have been described single cases of myocardial infarction; frequency is unknown: retrosternal pain, worsening of symptoms of heart failure.
Respiratory system disorders
infrequent: nasal bleeding, nasal congestion, cough, sinusitis, difficulty in breathing, upper respiratory tract infections;
frequency unknown: dyspnea, bronchospasm, pulmonary edema.
Digestive system disorders
often: constipation;
infrequently: dry oral mucosa, decreased appetite, dyspepsia (nausea, diarrhea), abdominal pain;
rarely: Gingival hyperplasia (bleeding, soreness, swelling);
frequency unknown: dysphagia, erosive and ulcerative lesions of intestinal mucosa, vomiting, insufficiency of gastroesophageal sphincter, with prolonged use – liver function disorders (intrahepatic cholestasis, increased activity of “liver” transaminases, jaundice), bezoars (lumps in the stomach from undigested food residues).
Musculoskeletal system and connective tissue
infrequent: cramps of the upper and lower extremities, joint swelling, back pain, gout;
frequency unknown: arthritis, arthralgia, myalgia.
Urogenital system disorders
infrequent: increased/decreased daily diuresis, erectile dysfunction;
rare: Gynecomastia (in elderly patients, completely disappearing after drug withdrawal);
frequency unknown: galactorrhea, worsening of renal function (in patients with renal insufficiency).
Skin and subcutaneous tissue
infrequent: alopecia, increased sweating, hemorrhagic rash.
General disorders and disorders at the site of administration
often: asthenia, weakness;
infrequently: nonspecific pain, chills, facial edema, periorbital edema, fever, weight gain.
Overdose
Overdose
Symptoms: peripheral vasodilation with pronounced and possibly prolonged pronounced BP decrease (headache, facial skin hyperemia, sinus node suppression, bradycardia and/or tachycardia, bradyarrhythmia), hyperglycemia, metabolic acidosis, hypoxia, cardiogenic shock with the development of pulmonary edema. In severe poisoning – loss of consciousness, coma.
Treatment of overdose consists of standard procedures for elimination of the drug from the body (administration of activated charcoal, gastric lavage), restoration of stable hemodynamic parameters, close monitoring of the heart, lungs and excretory system.
In cases of overdose of prolonged action drugs it is necessary to ensure the most complete elimination of the drug from the body, if possible, to flush the small intestine in order to prevent further absorption of the active substance. When using laxatives it should be taken into account that blockers of “slow” calcium channels may cause decrease in intestinal muscle tone up to intestinal atony.
Hemodialysis is not effective; plasmapheresis is recommended due to the high degree of binding to proteins and relatively small volume of distribution.
The treatment of bradyarrhythmias is symptomatic with the use of atropine and/or beta-sympathomimetics; if life-threatening bradyarrhythmias occur, a temporary pacemaker should be placed.
In case of persistent marked BP decrease as a result of cardiogenic shock and arterial vasodilation, calcium (1-2 g calcium gluconate, intravenously), dopamine (up to 25 µg/kg/min), dobutamine (up to 15 µg/kg/min), epinephrine (adrenaline) or norepinephrine (noradrenaline) should be used. Doses of these drugs should be determined solely on the basis of the effect obtained.
In view of possible volume overload of the heart, infusion therapy is recommended to be performed with caution under control of hemodynamic parameters.
The antidote is calcium preparations. Clearance of nifedipine is increased in patients with impaired liver function.
Similarities
Similarities
Additional information
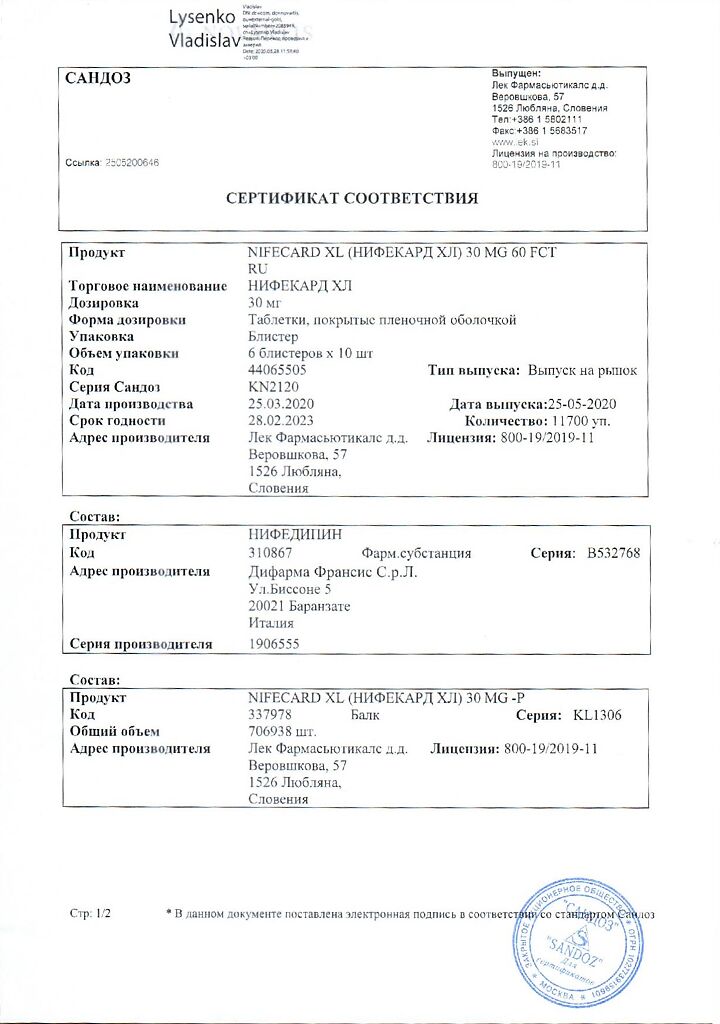
| Manufacturer | Lek d.d., Slovenia |
|---|---|
| Medication form | sustained release tablets |
| Brand | Lek d.d. |
Other forms…
Related products
Buy Nifekard XL, 30 mg 60 pcs with delivery to USA, UK, Europe and over 120 other countries.