No products in the cart.
Nebivolol-Teva, tablets 5 mg 28 pcs
€15.40 €12.83
Description
Pharmacotherapeutic group: beta1-adrenoblocker selective
Kode ATX: C07AB12
Farmacological properties
Pharmacodynamics
Nebivololol is a racemate, two enantiomers: SRRR-nebivolol (D-nebivolol) and RSSS-nebivolol (L-nebivolol), combining two pharmacological actions:
– D-nebivololol is a competitive and selective blocker of beta1 adrenoreceptors;
– L-nebivololol has a mild vasodilator effect related to its effect on the L-arginine/nitric oxide system and modulates the release of vasodilatory factor nitric oxide (NO) from the vascular endothelium.
Single and repeated administration of nebivololol reduces heart rate (HR) and blood pressure (BP) at rest and during exercise in both patients with normal BP and patients with arterial hypertension. The antihypertensive effect is maintained with long-term treatment.
In therapeutic doses, nebivololol does not have alpha-adrenergic antagonism. During short-term and long-term therapy with nebivolol, a decrease in total peripheral resistance is observed in patients with arterial hypertension. Despite the decrease of HR, the decrease of cardiac output at rest and during physical activity may be limited due to the increase of stroke volume.
In patients with arterial hypertension, nebivololol increases the NO-dependent vascular response to acetylcholine, which is reduced in patients with endothelial dysfunction.
Studies of morbidity and mortality in patients over 70 years of age with stable chronic heart failure (CHF) with reduced or preserved left ventricular (LV) ejection fraction (EF) showed that nebivolol added to standard therapy significantly increased time to death or hospitalization for cardiovascular causes (the primary endpoint for efficacy assessment) with a 14% reduction in relative risk (4.2% reduction in absolute risk). The relative risk reduction was observed after 6 months of treatment and persisted throughout the entire follow-up period. The efficacy of nebivolol was independent of age, sex, and LV EF in the study population. The reduction in all-cause mortality did not reach statistical significance compared with placebo.
There was a decrease in sudden death in patients receiving nebivololol compared with placebo.
The in vitro and in vivo animal experiments showed that nebivolol has no intrinsic sympathomimetic activity and membrane-stabilizing effect in pharmacological doses.
In healthy volunteers nebivololol has no significant effect on exercise tolerance.
Existing preclinical and clinical data showed no adverse effects of nebivololol on erectile function in patients with arterial hypertension.
Pharmacokinetics
absorption
Nebivololol is rapidly absorbed after oral administration. Food intake has no effect on absorption, so nebivololol can be taken regardless of meals.
The bioavailability of nebivololol after oral administration is on average 12% in patients with “fast” metabolism (first pass effect) and is almost complete in patients with “slow” metabolism.
Distribution
In plasma both enantiomers of nebivololol preferentially bind to albumin. Binding to plasma proteins is 98.1% for D-nebivololol and 97.9% for L-nebivolol. At equilibrium and at equal doses, the maximum plasma concentration of unchanged nebivololol in patients with “slow” metabolism is approximately 23 times higher than in patients with “fast” metabolism. When the concentrations of unchanged nebivolol and its active plasma metabolites are combined, the difference in maximum concentrations between “fast” and “slow” metabolizers is 1.3-1.4 times. Taking into account the differences in metabolic rate, the dose of the drug should be adjusted individually: in patients with “slow” metabolism lower doses may be used.
Elimation
Nebivololol is actively metabolized, partially with the formation of active hydroxymetabolites by alicyclic and aromatic hydroxylation, partial N-dealkylation and glucuronidation; in addition, hydroxymetabolite glucuronides are formed.
A week after administration of nebivololol, 38% of the dose is excreted by the kidneys and 48% by the intestine. Excretion of unchanged nebivolol is less than 0.5% of the oral dose. The elimination half-life (T1/2) in patients with “fast” metabolism: hydroxymetabolites – 24 hours, enantiomers of nebivolol – 10 hours; in patients with “slow” metabolism: hydroxymetabolites – 48 hours, enantiomers of nebivolol – 30-50 hours. In patients with “fast” metabolism, plasma levels of RSSS – enantiomers (L-nebivololol) are slightly higher than SRRR – enantiomers (D-nebivolol). In patients with “slow” metabolism this difference is even greater.
The equilibrium plasma concentration of nebivololol in most patients with “fast” metabolism is reached within 24 hours, and for hydroxymetabolites – after several days. Plasma concentrations are proportional to doses from 1 mg to 30 mg. The age of the patient does not affect the pharmacokinetics of the drug.
Indications
Indications
‒ arterial hypertension;
‒ stable chronic heart failure of mild to moderate severity (as part of combination therapy) in patients over 70 years of age.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: selective beta1-blocker
ATX code: C07AB12
Pharmacological properties
Pharmacodynamics
Nebivolol is a racemate of two enantiomers: SRRR-nebivolol (D-nebivolol) and RSSS-nebivolol (L-nebivolol), combining two pharmacological actions:
– D-nebivolol is a competitive and selective beta1-adrenergic receptor blocker;
– L-nebivolol has a mild vasodilatory effect associated with the effect on the L-arginine/nitric oxide system, and modulates the release of the vasodilating factor nitric oxide (NO) from the vascular endothelium.
Single and repeated doses of nebivolol reduce heart rate (HR) and blood pressure (BP) at rest and during exercise in both patients with normal blood pressure and in patients with arterial hypertension. The antihypertensive effect persists with long-term treatment.
At therapeutic doses, nebivolol does not exhibit alpha-adrenergic antagonism. During short-term and long-term therapy with nebivolol in patients with arterial hypertension, a decrease in total peripheral resistance is observed. Despite the decrease in heart rate, the decrease in cardiac output at rest and during exercise may be limited due to the increase in stroke volume.
In patients with arterial hypertension, nebivolol increases the NO-dependent vascular response to acetylcholine, which is reduced in patients with endothelial dysfunction.
A study examining morbidity and mortality in patients over 70 years of age with stable chronic heart failure (CHF) with reduced or preserved left ventricular (LV) ejection fraction (EF) found that nebivolol added to standard therapy significantly increased the time to death or hospitalization from cardiovascular causes (the primary efficacy endpoint) with a 14% relative risk reduction (absolute risk reduction of 4.2%). A reduction in relative risk was observed after 6 months of treatment and persisted throughout the observation period. The effectiveness of nebivolol in the study population did not depend on age, gender and LVEF. The reduction in all-cause mortality did not reach statistical significance compared with placebo.
A reduction in sudden death was found in patients receiving nebivolol compared with placebo.
Experiments in vitro and in vivo on animals have shown that nebivolol does not have intrinsic sympathomimetic activity and membrane-stabilizing effect at pharmacological doses.
In healthy volunteers, nebivolol does not have a significant effect on exercise capacity.
Existing preclinical and clinical data have not revealed a negative effect of nebivolol on erectile function in patients with arterial hypertension.
Pharmacokinetics
Suction
After oral administration, nebivolol is rapidly absorbed. Food intake does not affect absorption, so nebivolol can be taken regardless of meals.
The bioavailability of nebivolol after oral administration averages 12% in patients with “fast” metabolizers (the “first pass effect”) and is almost complete in patients with “slow” metabolizers.
Distribution
In blood plasma, both enantiomers of nebivolol are predominantly bound to albumin. Plasma protein binding for D-nebivolol is 98.1%, and for L-nebivolol – 97.9%. At steady state and at the same doses, the maximum plasma concentration of unchanged nebivolol in patients with “slow” metabolizers is approximately 23 times higher than in patients with “fast” metabolizers. When taking into account the concentrations of unchanged nebivolol and its active metabolites in blood plasma, the difference in maximum concentrations between “fast” and “slow” metabolizers is 1.3–1.4 times. Taking into account differences in metabolic rates, the dose of the drug should be selected individually: in patients with a “slow” metabolism, lower doses may be used.
Removal
Nebivolol is actively metabolized, partially to the formation of active hydroxymetabolites by alicyclic and aromatic hydroxylation, partial N-dealkylation and glucuronidation, in addition, glucuronides of hydroxymetabolites are formed.
A week after using nebivolol, 38% of the dose is excreted by the kidneys, 48% through the intestines. Excretion of unchanged nebivolol through the kidneys is less than 0.5% of the dose taken orally. Half-life (T1/2) in patients with “fast” metabolism: hydroxymetabolites – 24 hours, nebivolol enantiomers – 10 hours; in patients with “slow” metabolism: hydroxymetabolites – 48 hours, nebivolol enantiomers – 30–50 hours. In patients with “fast” metabolism, plasma levels of RSSS enantiomers (L-nebivolol) are slightly higher than SRRR enantiomers (D-nebivolol). In patients with “slow” metabolism, this difference is even greater.
The equilibrium concentration of nebivolol in the blood plasma in most patients with “fast” metabolism is achieved within 24 hours, and for hydroxymetabolites – after several days. Plasma concentrations are proportional to doses from 1 mg to 30 mg. The patient’s age does not affect the pharmacokinetics of the drug.
Special instructions
Special instructions
Discontinuation of therapy or “withdrawal syndrome”
Treatment with nebivolol should not be abruptly interrupted unless absolutely necessary. Particular caution should be exercised when it is necessary to discontinue therapy in patients with coronary artery disease, since worsening attacks of angina pectoris, the development of myocardial infarction and the occurrence of ventricular arrhythmias in patients with coronary artery disease have been observed with sudden cessation of beta-blockers. If discontinuation of treatment is necessary, the dose of nebivolol should be reduced gradually over 1–2 weeks. In case of significant worsening of angina or development of acute coronary syndrome, nebivolol should be temporarily resumed.
Diseases of the cardiovascular system
Monitoring blood pressure and heart rate at the beginning of taking the drug should be daily. Like other beta blockers, nebivolol may cause a prolongation of the PQ interval on the ECG. Nebivolol should be used with caution in patients with first degree atrioventricular block, cardiac conduction disorders, and a history of syncope. The simultaneous use of nebivolol with drugs that can prolong the PQ interval on the ECG is possible only if the expected benefit to the patient outweighs the possible risk of developing or worsening cardiac conduction disorders.
Vasospastic angina (Prinzmetal angina)
Non-selective beta-blockers may increase the frequency and duration of anginal attacks in patients with vasospastic angina (Prinzmetal’s angina), due to alpha-receptor-mediated vasoconstriction of the coronary artery. Cardioselective beta1-blockers should be used with caution in vasospastic angina.
Bradycardia
Beta blockers may cause bradycardia. If the resting heart rate decreases to less than 50–55 beats/min, the dose should be reduced or discontinued nebivolol.
Peripheral vascular diseases
Caution is required when using nebivolol in patients with peripheral vascular disease (including Raynaud’s syndrome), since beta-blockers may increase symptoms of arterial insufficiency.
Decompensated CHF
Beta blockers should not be used for decompensated CHF until the patient’s condition has stabilized. Nebivolol can be used for the treatment of stable mild to moderate CHF concomitantly with thiazide diuretics, digoxin, ACE inhibitors or angiotensin II receptor antagonists (ARA II).
Chronic obstructive pulmonary disease (COPD)
Patients with bronchospastic diseases can be prescribed cardioselective beta1-blockers in case of intolerance and/or ineffectiveness of other antihypertensive drugs.
Beta blockers should be used with caution in patients with chronic obstructive pulmonary disease, as bronchospasm may increase. Patients with a predisposition to bronchospasm may develop shortness of breath when taking beta-blockers as a result of increased airway resistance. Careful monitoring of such patients is necessary at the beginning of treatment and when increasing the dose of the drug, as well as reducing the dose of nebivolol when initial signs of bronchospasm appear. Before starting treatment, it is recommended to conduct a respiratory function test in patients with a history of bronchopulmonary diseases.
The effectiveness of beta-blockers is lower in smokers than in non-smokers.
Diabetes mellitus
Nebivolol does not affect plasma glucose concentrations in patients with diabetes mellitus. However, caution should be exercised when treating these patients because nebivolol may mask certain symptoms of hypoglycemia (eg, tachycardia) caused by oral hypoglycemic agents and insulin.
In patients with unstable diabetes mellitus and a history of episodes of spontaneous hypoglycemia, the use of beta-blockers may lead to worsening glycemic control and an increase in recovery time from hypoglycemia. In this case, dose adjustment of oral hypoglycemic agents and insulin may be necessary. This effect has typically occurred with non-selective beta-blockers and is less likely to occur with cardioselective beta-blockers (such as nebivolol).
Thyrotoxicosis
With hyperfunction of the thyroid gland, beta-blockers can mask tachycardia and reduce the severity of symptoms of thyrotoxicosis. Abrupt withdrawal of the drug can cause exacerbation of symptoms of the disease and the development of thyrotoxic crisis.
Pheochromocytoma
Patients with pheochromocytoma should be given an alpha blocker before starting any beta blocker (including nebivolol).
General surgery and general anesthesia
If surgical interventions are necessary, the anesthesiologist should be warned that the patient is taking beta-blockers (risk of drug interactions with the development of bradyarrhythmias and arterial hypotension). While taking nebivolol, one should use anesthetics that inhibit myocardial contractility with caution. For general anesthesia, it is recommended to use drugs with minimal negative inotropic effects.
It is recommended not to stop taking nebivolol in the perioperative period unless clearly necessary (since beta-adrenergic receptor blockade reduces the risk of arrhythmias during induction of anesthesia and tracheal intubation). If it is necessary to interrupt treatment with nebivolol before surgery, the drug should be discontinued at least 24 hours before surgery.
Hypersensitivity reactions
Beta blockers may increase sensitivity to allergens and the severity of anaphylactic/hypersensitivity reactions. The use of usual therapeutic doses of epinephrine (adrenaline) while taking beta-blockers does not always lead to achieving the desired clinical effect. Therefore, caution should be exercised when prescribing beta-blockers to patients with a history of severe hypersensitivity reactions or undergoing desensitization.
Psoriasis
When deciding on the use of nebivolol in patients with psoriasis, the expected benefits of the drug should be carefully weighed against the possible risk of exacerbation of psoriasis.
Contact lenses
Patients who use contact lenses should take into account that the use of beta-blockers may reduce the production of tear fluid. Preclinical studies using standard techniques did not reveal genotoxic or carcinogenic effects in humans.
Impact on the ability to drive vehicles and machinery
During treatment with Nebivolol-Teva, care must be taken when driving vehicles, using machinery and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions due to the likelihood of developing side effects such as dizziness and increased fatigue.
Active ingredient
Active ingredient
Nebivolol
Composition
Composition
One tablet contains: active substance nebivolol hydrochloride – 5.45 mg, corresponding to 5 mg nebivolol; excipients: colloidal silicon dioxide – 0.65 mg, magnesium stearate – 2.00 mg, croscarmellose sodium – 11.50 mg, macrogol 6000 – 20.00 mg, lactose monohydrate – 192.40 mg.
Pregnancy
Pregnancy
Nebivolol has pharmacological properties that can have a negative effect on the course of pregnancy and/or the fetus/newborn. All drugs from the beta-blocker class are characterized by a decrease in placental blood flow, which is associated with an increase in the incidence of fetal growth restriction, intrauterine fetal death, miscarriage or premature birth. It is also possible to develop such undesirable effects as hypoglycemia and bradycardia in the fetus or newborn (presumably during the first three days). If therapy with beta-blockers is necessary, preference is given to beta1-selective drugs. Nebivolol should not be used during pregnancy. During pregnancy, nebivolol is prescribed only for vital indications, when the benefit to the mother outweighs the possible risk to the fetus or newborn. If treatment with nebivolol is necessary, uteroplacental blood flow and fetal growth should be monitored. In case of a negative effect on the course of pregnancy and the fetus, the possibility of alternative therapy should be considered. The condition of the newborn should be carefully monitored. Symptoms of hypoglycemia and bradycardia can usually be expected within the first 3 days of life.
Animal studies have shown that nebivolol is excreted in breast milk. There are no data on whether nebivolol is excreted into breast milk in humans. Most beta blockers, especially lipophilic compounds such as nebivolol and its active metabolites, pass into breast milk to varying degrees. Therefore, during the use of nebivolol during lactation, breastfeeding should be discontinued.
Contraindications
Contraindications
– hypersensitivity to nebivolol or any of the components of the drug;
‒ liver failure (class B and C according to the Child-Pugh classification) or liver dysfunction;
– acute heart failure; cardiogenic shock; chronic heart failure in the stage of decompensation (requiring intravenous administration of drugs with a positive inotropic effect);
– severe arterial hypotension (systolic blood pressure less than 90 mm Hg);
‒ sick sinus syndrome, including sinoauricular block;
‒ atrioventricular (AV) block of the II and III degrees (without pacemaker);
– bradycardia (heart rate less than 60 beats/min before the start of therapy);
– untreated pheochromocytoma (without simultaneous use of alpha-blockers);
‒ metabolic acidosis;
– history of bronchospasm and bronchial asthma;
– severe peripheral circulatory disorders;
‒ lactose intolerance, lactase deficiency and glucose-galactose malabsorption syndrome;
‒ age under 18 years (efficacy and safety in this age group have not been studied);
‒ breastfeeding period;
– simultaneous use with floctafenine, sultopride (see section Interaction with other drugs);
With caution
– severe renal failure (glomerular filtration rate (GFR) < 30 ml/min/1.73 m2 body surface area);
‒ diabetes mellitus;
‒ hyperfunction of the thyroid gland;
– history of allergic diseases, psoriasis;
‒ chronic obstructive pulmonary disease (COPD);
– obliterating diseases of peripheral vessels (intermittent claudication, Raynaud’s syndrome);
‒ first degree atrioventricular block;
– Prinzmetal’s angina;
– age over 75 years;
– arterial hypotension;
– pheochromocytoma (with simultaneous use of alpha-blockers);
‒ surgical interventions and general anesthesia;
‒ carrying out desensitizing therapy;
‒ pregnancy.
Side Effects
Side Effects
The frequency of side effects is given in accordance with the classification of the World Health Organization: very often (more than 10%), often (more than 1% and less than 10%), infrequently (more than 0.1% and less than 1%), rarely (more than 0.01% and less than 0.1%), very rarely (less than 0.01%), frequency unknown (it was not possible to determine the frequency of occurrence based on available data).
Immune system disorders: frequency unknown – angioedema, hypersensitivity.
Mental disorders: infrequently – depression, nightmares.
Nervous system disorders: often – headache, dizziness, paresthesia; very rarely – fainting.
Visual disturbances: infrequently – visual disturbances.
Cardiac disorders: uncommon – bradycardia, heart failure, slowing of AV conduction.
Vascular disorders: uncommon – marked decrease in blood pressure, worsening intermittent claudication.
Disorders of the respiratory system, chest and mediastinal organs: often – shortness of breath; infrequently – bronchospasm.
Gastrointestinal disorders: often – nausea, constipation, diarrhea; infrequently – dyspepsia, flatulence, vomiting.
Disorders of the skin and subcutaneous tissues: infrequently – itching of the skin; erythematous skin rash; very rarely – aggravation of psoriasis; frequency unknown – urticaria.
Disorders of the genital organs and breast: uncommon – erectile dysfunction.
General disorders and disorders at the injection site: often – increased fatigue, swelling.
When using some beta-blockers, the following undesirable reactions may be observed: psychoses, hallucinations, confusion, coldness/cyanosis of the extremities, Raynaud’s syndrome, dry eye syndrome, oculo-mucotan syndrome of the practolol type.
Chronic heart failure
The most common adverse reactions during nebivolol therapy were bradycardia and dizziness, occurring in 11% of patients. Other adverse reactions, possibly related to the use of nebivolol, related to the treatment of CHF: decompensation of CHF, orthostatic hypotension, drug intolerance, AV block of the first degree, edema of the lower extremities.
Interaction
Interaction
Pharmacodynamic interactions
Contraindicated combinations
Floctafenine
Beta blockers may interfere with compensatory cardiovascular responses to hypotension or shock that may be caused by floctafenine.
Sultopride
Nebivolol should not be co-administered with sultopride as there is an increased risk of ventricular arrhythmias, especially torsade de pointes (TdP).
Combinations not recommended
With simultaneous use of nebivolol with class I antiarrhythmic drugs (for example, quinidine, hydroquinidine, cibenzoline, flecainide, disopyramide, lidocaine, mexiletine, propafenone), atrioventricular conduction time may be prolonged and the negative inotropic effect may be increased.
With the simultaneous use of beta-blockers with blockers of “slow” calcium channels (SCBC) (for example, verapamil, diltiazem), the negative effect on contractility and AV conduction increases. Intravenous administration of verapamil simultaneously with a beta-blocker can lead to severe arterial hypotension and AV block.
When used simultaneously with centrally acting antihypertensive drugs (for example, clonidine, guanfacine, moxonidine, methyldopa, rilmenidine), CHF may worsen due to a decrease in central sympathetic tone (decreased heart rate and cardiac output, vasodilation). Abrupt withdrawal, especially in the case of previous refusal of beta-blocker therapy, may increase the risk of developing rebound hypertension.
Combinations to use with caution
With simultaneous use of nebivolol with class III antiarrhythmic drugs (for example, amiodarone), an increase in AV conduction time may be observed. The simultaneous use of nebivolol and drugs for general anesthesia may suppress reflex tachycardia and increase the risk of developing arterial hypotension. The general rule is to avoid abrupt withdrawal of beta blockers. The anesthesiologist should be informed that the patient is taking nebivolol.
When nebivolol is used simultaneously with insulin and oral hypoglycemic agents, nebivolol does not affect glucose concentrations, but may mask the symptoms of hypoglycemia (palpitations, tachycardia).
With the simultaneous use of nebivolol with baclofen (a muscle relaxant) and amifostine (an antineoplastic drug), a decrease in blood pressure is possible, which requires appropriate adjustment of the dose of nebivolol.
Combinations to Consider
With the simultaneous use of nebivolol and cardiac glycosides, an increase in AV conduction time is possible. In clinical studies, there was no evidence of interaction between the two drugs. Nebivolol does not affect the pharmacokinetics of digoxin.
With the simultaneous use of nebivolol with dihydropyridine BMCC (for example, amlodipine, felodipine, lacidipine, nifedipine, nicardipine, nimodipine, nitrendipine), the risk of arterial hypotension and a decrease in left ventricular contractility in patients with CHF may increase.
With simultaneous use of nebivolol with tricyclic antidepressants, barbiturates and phenothiazine derivatives, the antihypertensive effect may be enhanced (additive effect).
Nonsteroidal anti-inflammatory drugs (NSAIDs) do not affect the antihypertensive effect of nebivolol.
Sympathomimetic agents may reduce the effectiveness of beta-blockers. Beta-agonists may lead to unrestricted alpha-adrenergic activity of sympathomimetic agents with alpha- and beta-adrenergic effects (risk of hypertension, severe bradycardia and cardiac arrest).
Pharmacokinetic interaction
With simultaneous use of nebivolol with drugs that inhibit serotonin reuptake, or other drugs that are biotransformed with the participation of the CYP2D6 isoenzyme (for example, paroxetine, fluoxetine, thioridazine and quinidine), the concentration of nebivolol in the blood plasma increases and the metabolism of nebivolol slows down, which can lead to the development of severe bradycardia and adverse reactions.
With simultaneous use of nebivolol with fingolimod, the negative chronotropic effect of beta-blockers and the development of severe bradycardia may be potentiated. If simultaneous use is necessary, extreme caution should be used.
With simultaneous use of nebivolol with cimetidine, the concentration of nebivolol in the blood plasma increases without affecting the therapeutic effect.
The simultaneous use of nebivolol and ranitidine does not affect the pharmacokinetic parameters of nebivolol. Nebivolol is taken with meals, and the antacid is taken between meals, so the drugs can be used simultaneously.
With simultaneous use of nebivolol with nicardipine, the concentrations of active substances in the blood plasma increase slightly, but do not affect the therapeutic effect.
Concomitant use of nebivolol and ethanol, furosemide or hydrochlorothiazide does not affect the pharmacokinetics of nebivolol.
Nebivolol does not affect the pharmacokinetics and pharmacodynamics of warfarin.
Overdose
Overdose
There is no data on drug overdose.
Symptoms of an overdose of beta-blockers: marked decrease in blood pressure, sinus bradycardia, bronchospasm and acute heart failure.
Treatment
In case of overdose or development of a hypersensitivity reaction, the patient should be constantly monitored in an intensive care unit. It is recommended to monitor plasma glucose concentrations. To prevent further absorption of the drug from the gastrointestinal tract, gastric lavage, activated charcoal and a laxative are necessary. Mechanical ventilation may be required.
For bradycardia or severe vagotonia, 0.5–2 mg of atropine should be administered intravenously (IV). In case of AV block (II–III stage), intravenous administration of beta-agonists is recommended; if they are ineffective, the installation of a pacemaker should be considered. With a pronounced decrease in blood pressure and shock, intravenous administration of plasma-substituting solutions and, if necessary, catecholamines is recommended. If the desired effect is absent, intravenous administration of glucagon at a rate of 50-100 mcg/kg body weight. In case of heart failure, treatment begins with the administration of cardiac glycosides and diuretics; if there is no effect, it is advisable to administer dopamine, dobutamine or vasodilators. For bronchospasm, bronchodilators are used, such as inhaled short-acting beta2-agonists and/or aminophylline. Nebivolol will probably not be eliminated during hemodialysis due to its high degree of binding to plasma proteins.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25°C.
Shelf life
Shelf life
3 years.
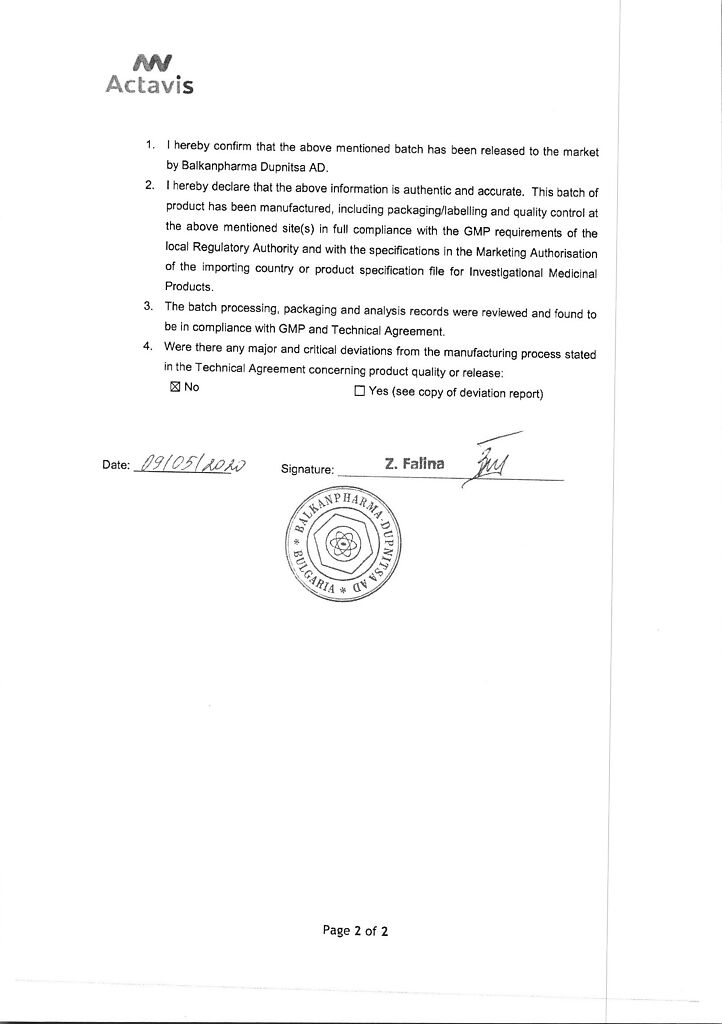
Manufacturer
Manufacturer
Balkanpharma – Dupnitsa AD, Bulgaria
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ° C. |
| Manufacturer | Balkanfarma – Dupnitsa AD, Bulgaria |
| Medication form | pills |
| Brand | Balkanfarma – Dupnitsa AD |
Related products
Buy Nebivolol-Teva, tablets 5 mg 28 pcs with delivery to USA, UK, Europe and over 120 other countries.