No products in the cart.
Description
Pharmacodynamics
Antitumor drug from vincaalkaloids group (alkaloid of pink periwinkle obtained by semi-synthetic way). The drug blocks cell mitosis at G2-M metaphase stage, causing cell death during interphase or subsequent mitosis. On the molecular level, it affects the dynamic equilibrium of tubulin in the microtubule apparatus of the cell. Navelbine inhibits tubulin polymerization by binding predominantly to mitotic microtubules, and in higher concentrations it also affects axonal microtubules. Induction of tubulin spiralization under the action of Navelbine is weaker than with vincristine.
Pharmacokinetics
Absorption and distribution
After oral administration, it is rapidly absorbed from the GI tract. Cmax vinorelbine is reached in 1.5-3 hours. Absolute bioavailability is on average 40%. Food intake does not affect the degree of absorption.
After IV administration the kinetics of vinorelbine is a three-phase exponential process.
The binding to plasma proteins is 13.5%. Intensively binds to blood cells and especially to platelets (78%). It penetrates into the tissues well and stays in them for a long time. High concentrations of vinorelbine are detected in the spleen, liver, kidneys, lungs and thymus gland, moderate – in the heart and muscles, minimal – in adipose tissue and bone marrow. Concentration in lungs is 300 times higher than in plasma. It does not penetrate through the BBB.
Metabolism and excretion
It is biotransformed in liver, mainly under the action of CYP3A4 isoenzyme with formation of several metabolites; basic one, detectable in blood is diacetylvinorelbine, which retains antitumor activity. It is excreted mainly with bile. Mean T1/2 in the terminal phase is 40 h (27.7-43.6 h).
Pharmacokinetics in special clinical cases
The pharmacokinetic parameters of Navelbine (administered at a dose of 20 mg/m2 weekly) are independent of patient age and do not change with moderate to severe hepatic impairment.
Indications
Indications
Non-small cell lung cancer;
breast cancer;
prostate cancer resistant to hormone therapy (in combination with small doses of corticosteroids for oral administration).
Pharmacological effect
Pharmacological effect
Pharmacodynamics
An antitumor drug from the group of vinca alkaloids (vinca rosea alkaloid, obtained semi-synthetically). The drug blocks cell mitosis at the G2-M metaphase stage, causing cell death during interphase or subsequent mitosis. At the molecular level, it affects the dynamic equilibrium of tubulin in the microtubule apparatus of the cell. Navelbine inhibits tubulin polymerization by binding predominantly to mitotic microtubules, and at higher concentrations also affects axonal microtubules. The induction of tubulin helicalization under the influence of Navelbine is less pronounced than when using vincristine.
Pharmacokinetics
Suction and distribution
After oral administration, it is quickly absorbed from the gastrointestinal tract. Cmax of vinorelbine is achieved after 1.5-3 hours. Absolute bioavailability averages 40%. Food intake does not affect the degree of absorption.
After intravenous administration, the kinetics of vinorelbine is a three-phase exponential process.
Plasma protein binding is 13.5%. Intensively binds to blood cells and especially platelets (78%). Penetrates well into tissues and remains in them for a long time. High concentrations of vinorelbine are determined in the spleen, liver, kidneys, lungs and thymus, moderate – in the heart and muscles, minimal – in adipose tissue and bone marrow. The concentration in the lungs is 300 times higher than the concentration in plasma. Does not penetrate the BBB.
Metabolism and excretion
Biotransformed in the liver, mainly under the influence of the CYP3A4 isoenzyme with the formation of a number of metabolites; The main one detected in the blood is diacetylvinorelbine, which retains antitumor activity. It is excreted primarily in bile. The average T1/2 in the terminal phase is 40 hours (27.7-43.6 hours).
Pharmacokinetics in special clinical situations
The pharmacokinetic parameters of Navelbine (administered at a dose of 20 mg/m2 weekly) do not depend on the age of patients and do not change with moderate or severe liver failure.
Special instructions
Special instructions
Treatment with Navelbine should be carried out under the supervision of a physician experienced in working with anticancer drugs.
In case of severe liver dysfunction, the dose of Navelbine should be reduced by 33%.
If renal function is impaired, it is necessary to monitor the patient’s condition.
If signs of neurotoxicity of grade 2 or more appear, the use of Navelbine should be discontinued. If shortness of breath, cough, or hypoxia of unknown etiology occurs, the patient should be examined to rule out pulmonary toxicity.
If extravasation occurs, the drug infusion should be stopped immediately and the remaining dose should be administered into another vein.
If nausea or vomiting occurs after taking Navelbine capsules, the same dose should not be taken again.
During and for at least three months after stopping therapy, reliable methods of contraception must be used.
If the active substance gets into the oral cavity, it is recommended to rinse your mouth with water or any saline solution.
If Navelbine gets into your eyes, rinse them copiously and thoroughly with water.
Because The drug contains sorbitol; Navelbine should not be used in patients with hereditary fructose intolerance.
Control of laboratory parameters
Treatment with the drug is carried out under strict hematological control, determining the number of leukocytes, neutrophils, platelets and hemoglobin level before each injection or oral administration. If the number of neutrophils decreases to less than 1500/μl and/or platelets to less than 75,000/μl (for intravenous administration) or less than 100,000/μl (for oral administration), the use of the next dose of the drug is postponed until the parameters are normalized, while the patient’s condition is monitored.
Active ingredient
Active ingredient
Vinorelbine
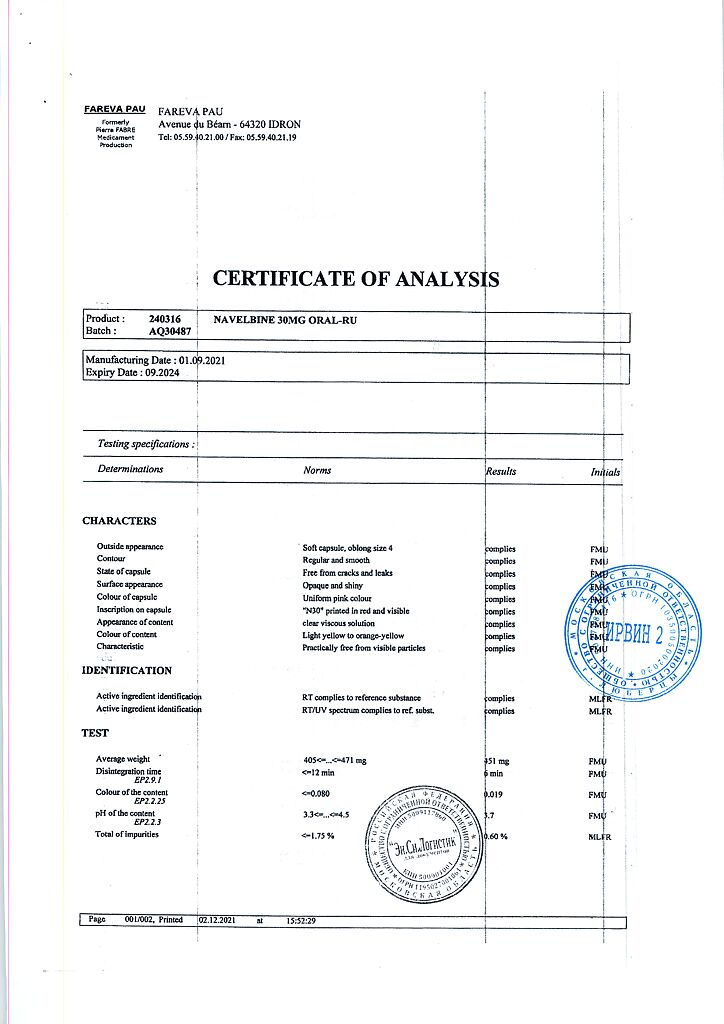
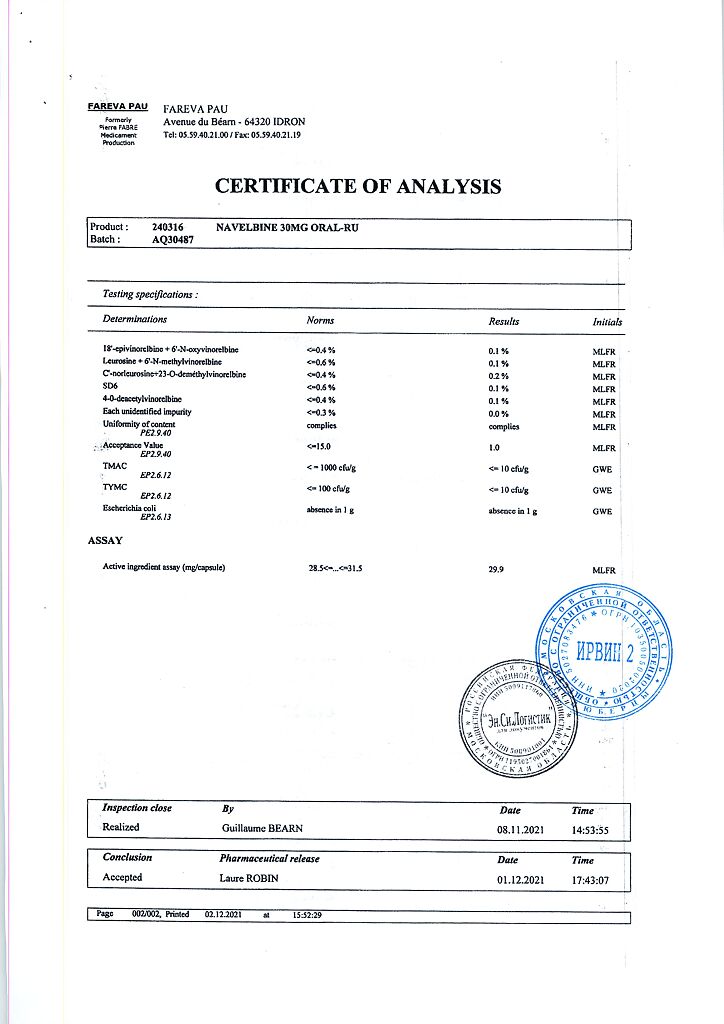
Composition
Composition
1 capsule contains:
Active ingredients:
vinorelbine tartrate 41.55 mg, which corresponds to the content of vinorelbine 30 mg.
Excipients:
ethanol anhydrous – 7.5 mg,
purified water – 18.75 mg,
glycerol – 3 mg,
macrogol 400 – q.s. up to 262.5 mg.
Composition of the capsule shell:
gelatin, glycerol 85%, anidrisorb 85/70 (D-sorbitol, 1,4-sorbitan, mannitol, higher polyols), medium chain triglycerides PHOSAL 53 MST (phosphatidylcholine, glycerides, ethanol), red iron oxide (E172), titanium dioxide (E171).
There is 1 capsule in a blister. The package contains 1 blister.
Pregnancy
Pregnancy
Navelbine is contraindicated for use during pregnancy and lactation (breastfeeding).
Contraindications
Contraindications
Neutrophil count less than 1500/µl;
platelet count less than 75,000/μl (for intravenous administration) and less than 100,000/μl (for oral administration);
severe infectious diseases during the initiation of therapy or suffered during the last two weeks;
severe liver dysfunction not associated with a tumor process;
the need for continuous oxygen therapy in patients with lung tumors;
diseases and conditions leading to decreased absorption from the gastrointestinal tract (for oral administration);
pregnancy;
lactation period (breastfeeding);
hypersensitivity to the drug and to other vinca alkaloids.
With caution: the drug is prescribed for respiratory failure, suppression of bone marrow hematopoiesis (including after previous chemotherapy or radiation therapy), constipation or a history of intestinal obstruction, a history of neuropathy.
Side Effects
Side Effects
The following side effects occurred more often than in isolated cases. The following criteria were used to assess the incidence of adverse events:
very often (> 1/10);
often (> 1/100.1/10);
sometimes (> 1/1000, 1/100);
rare (> 1/10,000, 1/1000);
extremely rare (1/10,000).
From the hematopoietic system: very often – neutropenia, anemia, thrombocytopenia, secondary infections due to suppression of bone marrow hematopoiesis; often – fever (38°C) accompanied by neutropenia; sometimes – sepsis, septicemia; extremely rarely – complicated septicemia, in some cases leading to death. The lowest number of neutrophils is observed on days 7-10 from the start of therapy, recovery occurs in the next 5-7 days. No accumulation of hematotoxicity was observed.
From the peripheral nervous system: very often – paresthesia, hyperesthesia, decrease or loss of deep tendon reflexes; often – weakness in the legs; sometimes – severe paresthesia with sensory and motor symptoms, usually reversible.
From the cardiovascular system: sometimes – increased or decreased blood pressure, hot flashes and cold extremities; rarely – ischemic heart disease (angina pectoris, myocardial infarction), severe hypotension, collapse; extremely rarely – tachycardia, palpitations, cardiac arrhythmia.
From the respiratory system: sometimes – shortness of breath, bronchospasm; rarely – interstitial pneumonia (with combination therapy with mitomycin), acute respiratory distress syndrome.
From the digestive system: very often – nausea, vomiting, stomatitis, constipation, diarrhea, transient increase in liver function tests (ALT, AST); rarely – pancreatitis, increased bilirubin levels, intestinal paresis.
From the immune system: rarely – anaphylactic shock, angioedema.
Dermatological reactions: often – alopecia; rarely – skin rashes.
Local reactions: often – pain/burning or redness at the injection site, discoloration of the vein, phlebitis; with extravasation – cellulite; possibly necrosis of surrounding tissues.
Other: often – increased fatigue, myalgia, arthralgia, fever, pain of various localizations, including chest pain, pain in the lower jaw and in the area of tumor formations; rarely – hyponatremia; very rarely – hemorrhagic cystitis and syndrome of inappropriate ADH secretion.
Interaction
Interaction
When used together with other cytostatics, mutual aggravation of side effects is possible, primarily myelosuppression.
When used together with mitomycin C, acute respiratory failure may develop.
When used in combination with paclitaxel, the risk of neurotoxicity increases.
Use during radiation therapy leads to radiosensitization. The use of Navelbine after radiation therapy can lead to the reappearance of radiation reactions.
Concomitant use of the drug with inducers and inhibitors of cytochrome P450 isoenzymes may lead to changes in the pharmacokinetics of vinorelbine.
Overdose
Overdose
Symptoms: suppression of bone marrow function, neurotoxic reactions.
Treatment: in case of overdose, the patient should be hospitalized; carry out symptomatic therapy with careful monitoring of the functions of vital organs. A specific antidote is unknown.
Storage conditions
Storage conditions
In a place protected from light, at a temperature of 2–8 °C
Shelf life
Shelf life
2.5 years
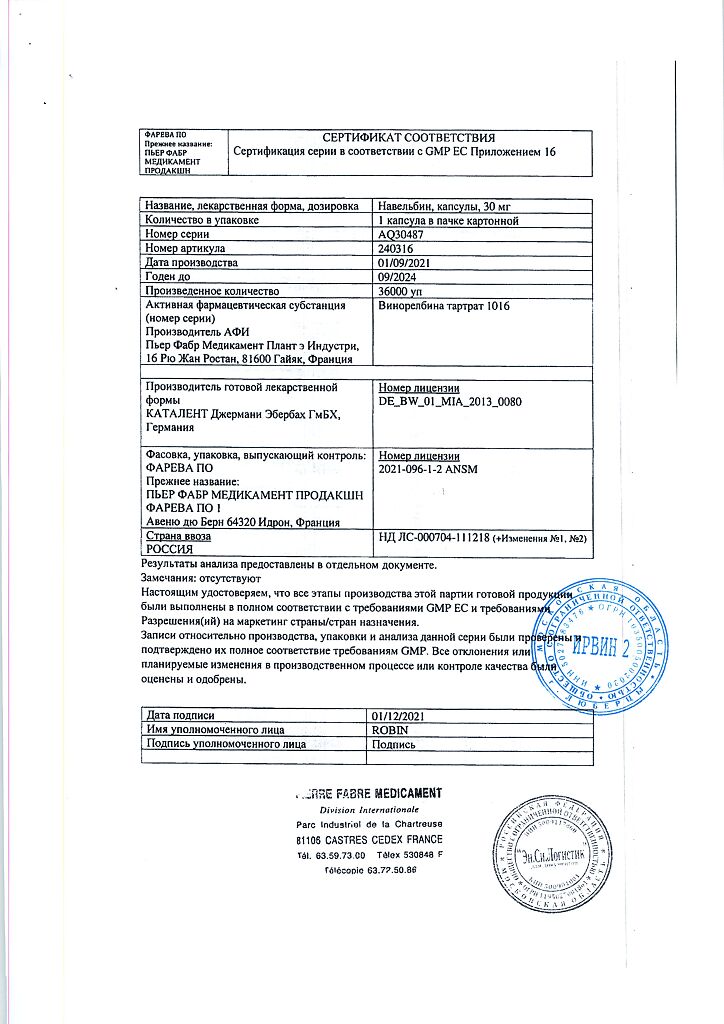
Manufacturer
Manufacturer
Catalent Germani Eberbach GmbH, Germany
Additional information
| Shelf life | 2.5 years |
|---|---|
| Conditions of storage | In a light-protected place, at 2-8 °C |
| Manufacturer | Catalent Germani Eberbach GmbH, Germany |
| Medication form | capsules |
| Brand | Catalent Germani Eberbach GmbH |
Related products
Buy Navelbine, 30 mg capsules with delivery to USA, UK, Europe and over 120 other countries.