No products in the cart.
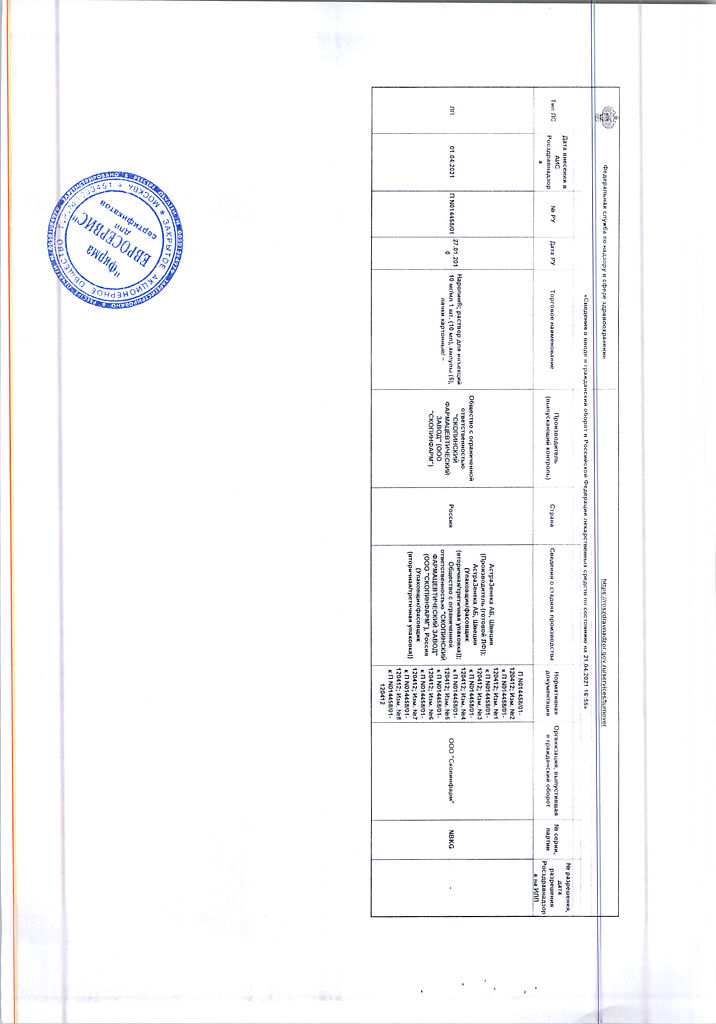
Naropin, 10 mg/ml 5 amp pcs
€40.47 €33.73
EAN: 5060249174462
SKU: 125049
Categories: Anesthesia and resuscitation, Anesthesia solutions, Medicine
Description
A long-acting local anesthetic of the amide type. It reversibly blocks voltage-dependent sodium channels and thus prevents generation of impulses in the endings of sensitive nerves and conduction of impulses along the nerve fibers.
The duration of action depends on the route of administration and the dose of the drug.
Pharmacokinetics
Absorption
After administration, ropivacaine is completely absorbed from the epidural space. Absorption is biphasic. Plasma concentration of ropivacaine depends on the dose, route of administration and vascularization of the injection area. Pharmacokinetics of ropivacaine is linear, Cmax is proportional to the administered dose.
Distribution
The pKa of ropivacaine is 8.1; the distribution coefficient is 141 (n-octanol/phosphate buffer pH 7.4).
Vd is 47 l. The average hepatic extraction rate obtained in the experiment is 0.4. Ropivacaine binds in plasma mainly to α1-acid glycoproteins, the unbound fraction is about 6%.
Long-term epidural administration of ropivacaine leads to an increase in total plasma content of ropivacaine, which is due to a postoperative increase in blood levels of α1-acid glycoproteins. However, the concentration of the unbound, pharmacologically active form of ropivacaine in plasma changes to a much lesser extent than the total concentration.
Ropivacaine passes well through the placental barrier. Binding to plasma proteins is lower in the fetus than in the mother.
Metabolism
The drug is actively biotransformed in the body, mainly by hydroxylation. The main metabolite is 3-hydroxy-ropivacaine.
The T1/2 is biphasic and is 14 min (α-phase) and 4 h (β-phase). Total plasma clearance is 440 ml/min. After IV administration about 86% of the dose is excreted with the urine, mainly as metabolites, and only about 1% of the dose is excreted unchanged with the urine. About 37% of 3-hydroxy-ropivacaine is excreted with the urine mainly in the conjugated form.
Indications
Indications
Anesthesia for surgical interventions:
epidural block during surgical interventions, including caesarean section;
blockade of large nerves and nerve plexuses;
blockade of individual nerves and infiltration anesthesia.
Relief of acute pain syndrome:
extended epidural infusion or intermittent bolus administration, for example, to relieve postoperative pain or labor pain;
blockade of individual nerves and infiltration anesthesia;
prolonged block of peripheral nerves;
intra-articular injection.
Relief of acute pain syndrome in pediatrics:
caudal epidural block in newborns and children up to 12 years of age inclusive;
extended epidural infusion in newborns and children up to 12 years of age inclusive.
Pharmacological effect
Pharmacological effect
Long-acting amide-type local anesthetic. Reversibly blocks voltage-dependent sodium channels and thus prevents the generation of impulses at the endings of sensory nerves and the conduction of impulses along nerve fibers.
The duration of action depends on the route of administration and dose of the drug.
Pharmacokinetics
Suction
After administration, ropivacaine is completely absorbed from the epidural space. Absorption is biphasic. The plasma concentration of ropivacaine depends on the dose, route of administration and vascularization of the injection site. The pharmacokinetics of ropivacaine is linear, Cmax is proportional to the administered dose.
Distribution
pKa of ropivacaine is 8.1; distribution coefficient – 141 (n-octanol/phosphate buffer pH 7.4).
Vd is 47 l. The average hepatic extraction rate obtained in the experiment was 0.4. Ropivacaine binds in blood plasma mainly to α1-acid glycoproteins, the unbound fraction is about 6%.
Long-term epidural administration of ropivacaine leads to an increase in the total content of ropivacaine in the blood plasma, which is due to a postoperative increase in the level of α1-acid glycoproteins in the blood. In this case, the concentration of the unbound, pharmacologically active form of ropivacaine in the blood plasma changes to a much lesser extent than the total concentration.
Ropivacaine passes well through the placental barrier. Plasma protein binding is lower in the fetus than in the mother.
Metabolism
It is actively biotransformed in the body, mainly through hydroxylation. The main metabolite is 3-hydroxy-ropivacaine.
Removal
T1/2 is biphasic and is 14 minutes (α-phase) and 4 hours (β-phase). Total plasma clearance – 440 ml/min. After IV administration, about 86% of the dose is excreted in the urine, mainly in the form of metabolites, and only about 1% of the dose is excreted unchanged in the urine. About 37% of 3-hydroxy-ropivacaine is excreted in the urine, mainly in conjugated form.
Special instructions
Special instructions
Anesthesia must be administered by experienced professionals. Availability of equipment and medications for resuscitation measures is mandatory. An intravenous catheter must be installed before large blockades can be performed.
Personnel providing anesthesia should be appropriately trained and familiar with the diagnosis and treatment of possible side effects, systemic toxic reactions and other possible complications (see section “Overdose”).
A complication of unintentional subarachnoid injection may be a spinal block with respiratory arrest and decreased blood pressure. Convulsions occur more frequently with brachial plexus blocks and epidural blocks, probably due to accidental intravascular injection or rapid absorption at the injection site.
Peripheral nerve blocks may require large volumes of local anesthetic to be injected into highly vascular areas, often close to large vessels, which increases the risk of intravascular administration and/or rapid systemic absorption, which can result in high plasma drug concentrations.
Some procedures that involve the use of local anesthetics, such as injections in the head and neck area, may be associated with an increased incidence of serious side effects, regardless of the type of local anesthetic used. Care must be taken to avoid injecting into an area of inflammation.
Caution should be exercised when administering the drug to patients with degree II and III intracardiac conduction block, patients with severe renal failure, elderly and debilitated patients.
There have been reports of rare cases of cardiac arrest when using Naropin® for epidural anesthesia or peripheral nerve blockade, especially after accidental intravascular administration of the drug, in elderly patients and in patients with concomitant cardiovascular diseases.
In some cases, resuscitation measures were difficult. Cardiac arrest usually requires longer resuscitation efforts.
Since Naropin® is metabolized in the liver, caution should be exercised when using the drug in patients with severe liver disease; in some cases, due to delayed elimination, it may be necessary to reduce repeated doses of anesthetic.
Typically, in patients with renal failure, when the drug is administered once or when the drug is used for a short period of time, no dose adjustment is required. However, acidosis and a decrease in plasma protein concentrations, which often develop in patients with chronic renal failure, may increase the risk of systemic toxicity of the drug (see section “Dosage and Administration”). The risk of systemic toxicity is also increased when using the drug in patients with low body weight and patients with hypovolemic shock.
Epidural anesthesia can lead to a decrease in blood pressure and bradycardia. The introduction of vasoconstrictor drugs or an increase in blood volume may reduce the risk of developing such side effects. The decrease in blood pressure should be promptly corrected by intravenous administration of 5–10 mg of ephedrine, repeated if necessary.
When administering the drug intra-articularly, caution should be exercised if there is a suspicion of recent extensive joint trauma or surgery with exposure of large joint surfaces, due to the possibility of increased absorption of the drug and higher concentrations of the drug in plasma.
Patients receiving therapy with class III antiarrhythmic drugs (eg, amiodarone) should be closely monitored, and ECG monitoring is recommended due to the risk of increased cardiovascular effects.
Long-term use of Naropin should be avoided in patients taking strong P4501A2 inhibitors (such as fluvoxamine and enoxacin).
The possibility of cross-hypersensitivity should be taken into account when using Naropin® simultaneously with other amide-type local anesthetics.
Patients on a sodium-restricted diet should take into account the sodium content of the drug.
The use of the drug in newborns requires taking into account the possible immaturity of organs and physiological functions of newborns. The clearance of the unbound fraction of ropivacaine and pipeloxylidine (PPK) depends on the body weight and age of the child in the first years of life. The influence of age is reflected in the development and maturity of liver function, with clearance reaching its maximum value at about 1–3 years of age. T1/2 of ropivacaine is 5-6 hours in newborns and children aged 1 month compared to 3 hours in older children. Due to insufficient development of liver functions, systemic exposure to ropivacaine is higher in newborns, moderately higher in children from 1 to 6 months compared to older children. Significant differences in plasma concentrations of ropivacaine in neonates observed in clinical studies suggest an increased risk of systemic toxicity in this group of patients, especially with prolonged epidural infusion.
Recommended doses for neonates are based on limited clinical data.
When using ropivacaine in newborns, monitoring of systemic toxicity (monitoring for signs of toxicity from the central nervous system, ECG, monitoring blood oxygenation) and local neurotoxicity is necessary, which should be continued after completion of the infusion due to the slow elimination of the drug in newborns.
The use of the drug in concentrations higher than 5 mg/ml, as well as the intrathecal use of Naropin® in children, have not been studied.
Naropin® has the potential to cause porphyria and should only be used in patients diagnosed with acute porphyria if there is no safer alternative. In case of hypersensitivity of patients, necessary precautions should be taken.
Cases of chondrolysis have been reported with postoperative extended intra-articular infusion of local anesthetics. In most of the reported cases, infusion was performed into the shoulder joint. A cause-and-effect relationship with the use of anesthetics has not been established. Naropin® should not be used for prolonged intra-articular infusion.
Impact on the ability to drive vehicles and other mechanisms. In addition to the analgesic effect, Naropin® may have a weak transient effect on motor function and coordination. Given the side effect profile of the drug, caution must be exercised when driving vehicles and performing other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Ropivacaine
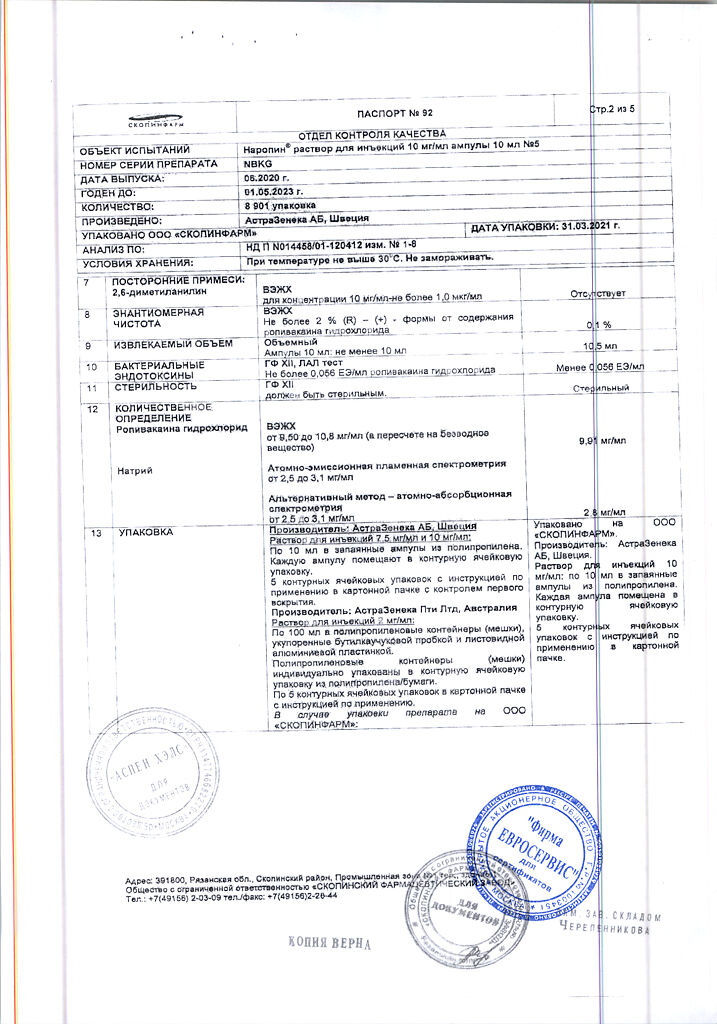
Composition
Composition
Active ingredient:
ropivacaine hydrochloride 10 mg;
Excipients:
sodium chloride;
hydrochloric acid or sodium hydroxide (up to pH 4–6);
water for injections;
Pregnancy
Pregnancy
Pregnancy
There was no effect of ropivacaine on fertility and reproductive function, as well as teratogenic effects. No studies have been conducted to evaluate the possible effect of ropivacaine on fetal development in women.
Naropin can be used during pregnancy only if justified by the clinical situation (in obstetrics, the use of the drug for anesthesia or analgesia is well justified).
Studies of the effect of the drug on reproductive function were carried out on animals. In studies in rats, ropivacaine had no effect on fertility or reproduction over two generations. When maximum doses of the drug were administered to pregnant rats, an increase in offspring mortality was observed in the first three days after birth, which may be explained by the toxic effect of ropivacaine on the mother, leading to disruption of the maternal instinct.
Teratogenicity studies in rabbits and rats showed no adverse effects of ropivacaine on organogenesis or early fetal development. Also, during perinatal and postnatal studies in rats receiving the maximum tolerated dose of the drug, no adverse effects were observed on late stages of fetal development, labor, lactation, viability or growth of the offspring. Perinatal and postnatal comparative studies of ropivacaine with bupivacaine showed that, unlike ropivacaine, the toxic effects of bupivacaine were observed at significantly lower doses of the drug and at lower concentrations of unbound bupivacaine in the blood.
Lactation
The excretion of ropivacaine or its metabolites into breast milk has not been studied. Based on experimental data, the dose of the drug received by the newborn is estimated to be 4% of the dose administered to the mother (drug concentration in milk/drug concentration in plasma). The total dose of ropivacaine that affects the baby during breastfeeding is significantly less than the dose that can enter the fetus when an anesthetic is administered to the mother during childbirth.
If it is necessary to use the drug during breastfeeding, the ratio of potential benefit to the mother and possible risk to the infant should be considered.
Contraindications
Contraindications
Hypersensitivity to the components of the drug.
With caution: the drug should be administered to weakened elderly patients or patients with severe concomitant diseases, such as second and third degree intracardiac conduction blocks (sinoatrial, atrioventricular, intraventricular), progressive liver diseases, severe liver failure, severe chronic renal failure, during the treatment of hypovolemic shock. For these patient groups, regional anesthesia is often preferred. When performing “major” blockades, in order to reduce the risk of severe adverse events, it is recommended to first optimize the patient’s condition, as well as adjust the dose of the anesthetic.
Caution should be exercised when injecting local anesthetics into the head and neck area due to the possible increased incidence of serious side effects.
When administering the drug intra-articularly, caution should be exercised if there is a suspicion of recent extensive joint trauma or surgery with exposure of large joint surfaces due to the possibility of increased absorption of the drug and a higher concentration of the drug in the plasma.
Particular attention should be paid when using the drug in children under 6 months due to the immaturity of organs and functions.
Patients on a sodium-restricted diet should take into account the sodium content of the drug.
Side Effects
Side Effects
Adverse reactions to Naropin® are similar to reactions to other amide-type local anesthetics. These should be distinguished from physiological effects resulting from sympathetic nerve blockade during epidural anesthesia, such as decreased blood pressure, bradycardia, or effects related to the injection technique, such as local nerve injury, meningitis, post-dural puncture headache, and epidural abscess.
Side effects associated with local anesthetics
From the central and peripheral nervous system
Neuropathy and dysfunction of the spinal cord are possible (anterior spinal artery syndrome, arachnoiditis, cauda equina syndrome), usually associated with the technique of regional anesthesia, and not with the effect of the drug.
Complete spinal block may occur as a result of accidental intrathecal administration of an epidural dose.
Serious complications are possible with systemic overdose and unintentional intravascular administration of the drug (see section “Overdose”).
Acute systemic toxicity
Naropin can cause acute systemic toxic reactions when using high doses or when its concentration in the blood rapidly increases due to accidental intravascular administration of the drug or its overdose (see section “Overdose”).
Most common side effects
Various side effects of the drug have been reported, the vast majority of which were related not to the effects of the anesthetic used, but to the technique of regional anesthesia.
The most common (>1%) side effects were the following, which were considered to be of clinical significance, regardless of whether a cause-and-effect relationship with the use of the anesthetic was established: decreased blood pressure*, nausea, bradycardia, vomiting, paresthesia, increased body temperature, headache, urinary retention, dizziness, chills, increased blood pressure, tachycardia, hypoesthesia, anxiety.
Very often
From the cardiovascular system: decreased blood pressure.
From the gastrointestinal tract: nausea.
Often
From the nervous system: paresthesia, dizziness, headache.
From the cardiovascular system: bradycardia, tachycardia, hypertension.
From the gastrointestinal tract: vomiting.
From the genitourinary system: urinary retention.
General: back pain, chills, increased body temperature.
Uncommon
From the nervous system: anxiety, symptoms of toxicity from the central nervous system (convulsions, grand mal seizures, paresthesia in the perioral area, dysarthria, numbness of the tongue, visual disturbances, tinnitus, tremor, muscle cramps), hypoesthesia.
From the vascular system: fainting.
From the respiratory system: shortness of breath, difficulty breathing.
General: hypothermia.
Rarely
From the cardiovascular system: arrhythmia, cardiac arrest.
General: allergic reactions (anaphylactic reactions, angioedema, urticaria).
Interaction
Interaction
Strengthens the toxic effect of other local anesthetics and drugs that are structurally similar to amide-type local anesthetics.
Overdose
Overdose
Acute systemic toxicity
Cases of seizures have been observed following accidental intravascular administration during plexus or other peripheral blockades.
If the epidural dose of anesthetic is administered intrathecally, a complete spinal block may occur.
Accidental intravascular injection of anesthetic may cause immediate toxicity.
In case of overdose during regional anesthesia, symptoms of a systemic toxic reaction appear in a delayed manner 15–60 minutes after injection due to a slow increase in the concentration of local anesthetic in the blood plasma. Systemic toxicity is primarily manifested by symptoms from the central nervous system and cardiovascular system. These reactions are caused by high concentrations of local anesthetic in the blood, which can occur due to (accidental) intravascular injection, overdose or exceptionally high adsorption from highly vascularized areas. CNS reactions are similar for all amide-type local anesthetics, while cardiovascular reactions are more dependent on the drug administered and its dose.
Central nervous system
Manifestations of systemic toxicity from the central nervous system develop gradually: visual disturbances, numbness around the mouth, numbness of the tongue, hyperacusis, tinnitus, and dizziness first appear. Dysarthria, tremor and muscle twitching are more serious manifestations of systemic toxicity and may precede the onset of generalized seizures (these signs should not be mistaken for neurotic behavior of the patient). As intoxication progresses, loss of consciousness, attacks of convulsions lasting from several seconds to several minutes, accompanied by respiratory failure, rapid development of hypoxia and hypercapnia due to increased muscle activity and inadequate ventilation, may occur. In severe cases, breathing may even stop. The resulting acidosis, hyperkalemia, and hypocalcemia enhance the toxic effects of the anesthetic.
Subsequently, due to the redistribution of the anesthetic from the central nervous system and its subsequent metabolism and excretion, a fairly rapid restoration of function occurs, unless a large dose of the drug was administered.
Cardiovascular system
Cardiovascular disorders are signs of more serious complications. A decrease in blood pressure, bradycardia, arrhythmia and, in some cases, even cardiac arrest can occur due to high systemic concentrations of local anesthetics. In rare cases, cardiac arrest is not accompanied by previous symptoms from the central nervous system. In studies on volunteers, intravenous infusion of ropivacaine led to inhibition of cardiac conduction and contractility. Cardiovascular symptoms are usually preceded by central nervous system toxicities, which may not be noticed if the patient is under sedation (benzodiazepines or barbiturates) or general anesthesia.
In children, early signs of systemic toxicity from local anesthetics may be more difficult to detect due to children’s difficulty describing symptoms or when regional anesthesia is used in combination with general anesthesia.
Treatment of acute toxicity
If the first signs of acute systemic toxicity appear, the drug should be discontinued immediately.
When seizures and symptoms of central nervous system depression appear, the patient requires adequate treatment, the purpose of which is to maintain oxygenation, relieve seizures, and maintain the activity of the cardiovascular system. Oxygenation should be ensured and, if necessary, switching to mechanical ventilation. If after 15–20 seconds the seizures do not stop, anticonvulsants should be used: sodium thiopental 1–3 mg/kg IV (provides rapid relief of seizures) or diazepam 0.1 mg/kg IV (the action develops more slowly compared to the action of sodium thiopental). Suxamethonium 1 mg/kg quickly relieves seizures, but its use requires intubation and mechanical ventilation.
If the activity of the cardiovascular system is suppressed (decreased blood pressure, bradycardia), it is necessary to administer 5-10 mg of ephedrine intravenously; if necessary, repeat the administration after 2-3 minutes. If circulatory failure or cardiac arrest develops, standard resuscitation measures should be started immediately. It is vital to maintain optimal oxygenation, ventilation and circulation and correct acidosis. If cardiac arrest occurs, longer resuscitation measures may be required.
When treating systemic toxicity in children, it is necessary to adjust doses according to the age and body weight of the patient.
Storage conditions
Storage conditions
Below 30°C (do not freeze)
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
AstraZeneca AB, Sweden
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At temperatures below 30 °C (do not freeze) |
| Manufacturer | AstraZeneca AB, Sweden |
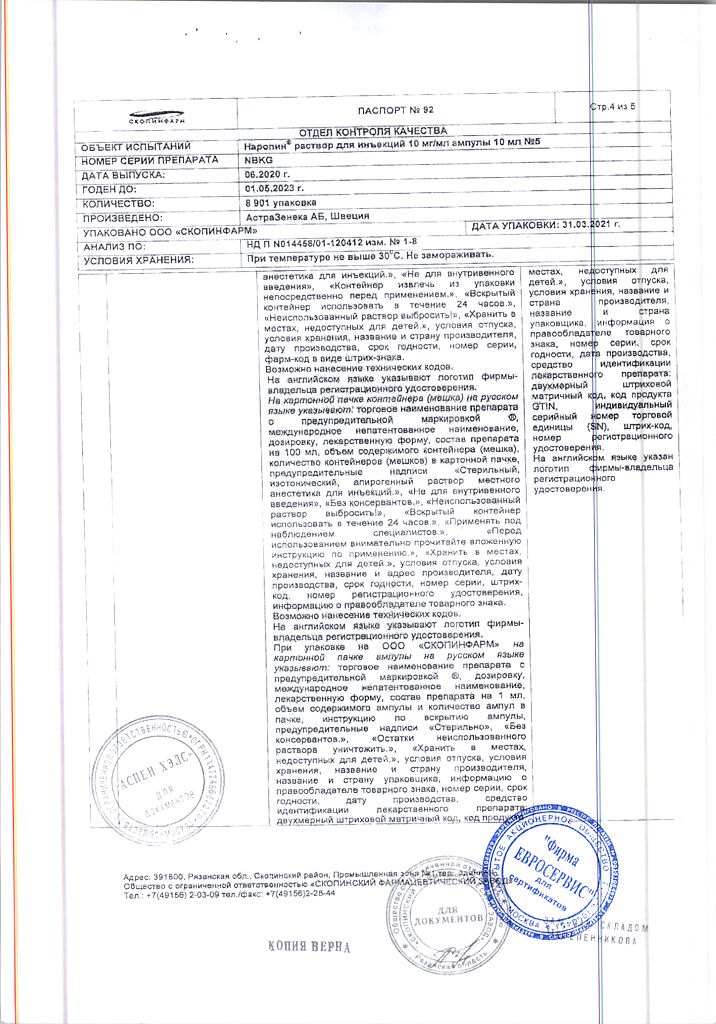
| Medication form | solution for injection |
| Brand | AstraZeneca AB |
Related products
Buy Naropin, 10 mg/ml 5 amp pcs with delivery to USA, UK, Europe and over 120 other countries.